amiodarone and thyroid dysfunction
Amiodarone may cause significant thyroid dysfunction due to its high iodine content, direct effects on thyroid follicular cells, and changes in thyroid hormone metabolism. There are 3 thyroid-related syndromes associated with amiodarone use:
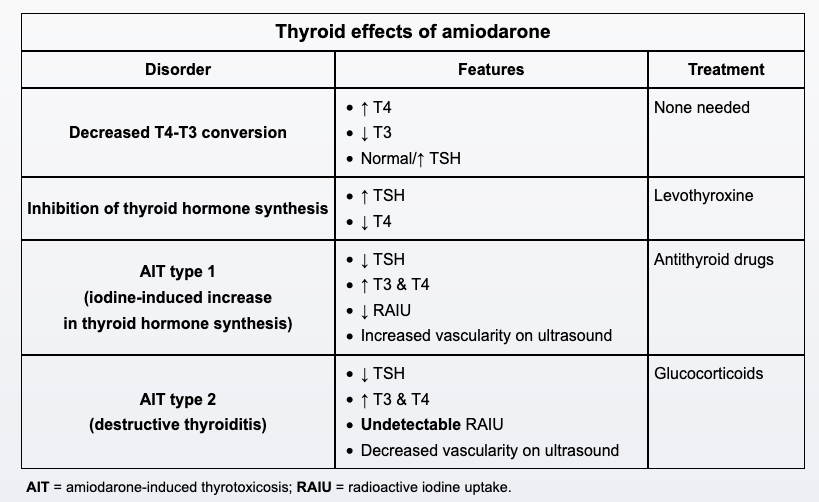
- Amiodarone decreases the peripheral conversion of T4 to T3. As in this patient, this may result in higher T4, lower T3, and normal or mildly elevated TSH (<20 mU/L). The thyroid test abnormalities are most prominent in the first 1-3 months after starting amiodarone and may become less apparent afterward. These patients are clinically euthyroid.
- The high iodine content in amiodarone inhibits thyroid hormone synthesis, leading to primary hypothyroidism (Wolff-Chaikoff effect).
- Amiodarone can also induce thyrotoxicosis (amiodarone-induced thyrotoxicosis [AIT]) due to either increased thyroid hormone synthesis (AIT type 1) or destructive thyroiditis (AIT type 2). In both AIT subtypes, TSH will be low.
Patients on chronic amiodarone therapy should have periodic monitoring of TSH (every 3-4 months).