achalasia and pseudoachalasia
Achalasia is a hypertonic motility condition defined by inadequate relaxation of the LES and aperistalsis. Achalasia can be idiopathic or associated with viral, autoimmune, and neurodegenerative disorders and infection (Chagas disease). Damage to the ganglion cells and myenteric plexus in the esophageal body and LES leads to uncontested cholinergic nerve activation, which prevents LES relaxation. Achalasia affects men and women equally, with an annual incidence of 1 in 100,000 individuals. It commonly occurs between 30 and 60 years of age. Patients present with dysphagia occurring with both solids and liquids along with nonacidic regurgitation of undigested food. Additional symptoms include heartburn, weight loss, and chest pain unresponsive to acid-reducing agents. Extrinsic compression from surgical procedures, such as fundoplication or bariatric surgery (gastric band), can also cause secondary achalasia. Barium esophagography is the initial diagnostic test, which shows dilation of the esophagus with narrowing at the gastroesophageal junction (GEJ), known as a “bird's beak” (Figure 5). Upper endoscopy reveals retained food and saliva, no signs of mechanical obstruction or mass, and “tightness” at the GEJ while advancing the scope into the stomach. Esophageal manometry showing incomplete LES relaxation and aperistalsis confirms the diagnosis of achalasia.
Manometry can confirm the diagnosis and shows elevated lower esophageal sphincter (LES) pressure and incomplete relaxation as well as aperistalsis. However, manometry cannot differentiate between primary idiopathic achalasia and pseudoachalasia. As a result, endoscopy is recommended prior to manometry in all suspected cases of pseudoachalasia to rule out malignancy (Choice B). Endoscopy may show a dilated esophagus with residual food debris, possible inflammation or ulceration, and Candida infection from esophageal stasis. The LES may not open spontaneously, but the scope can be advanced into the stomach with gentle pressure. However, in cases of neoplasm or strictures, it is not possible to advance the scope into the stomach.
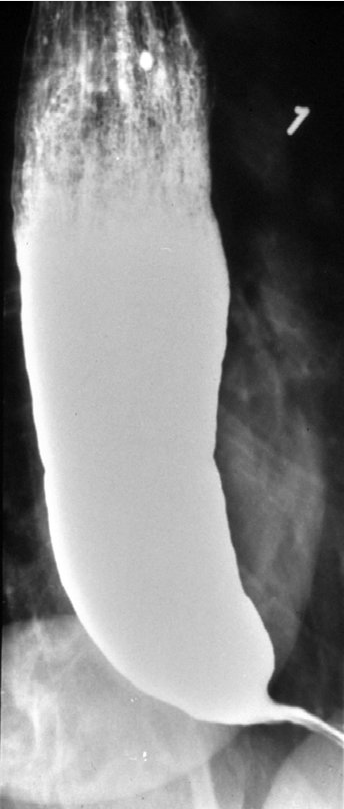
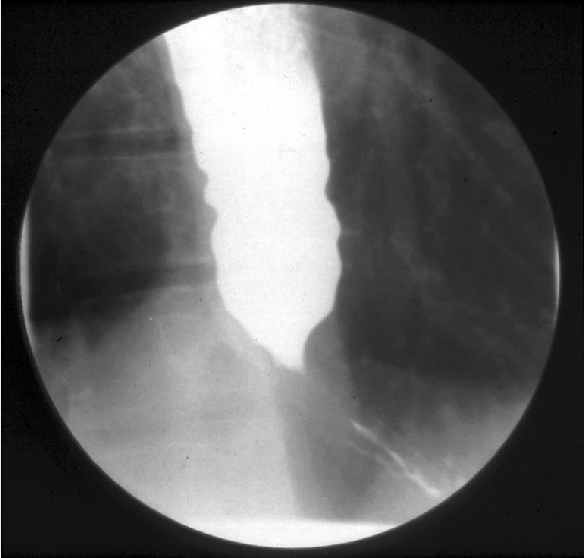 Barium esophagram showing the typical appearance of a dilated esophagus and “bird's beak” narrowing at the gastroesophageal junction in a patient with achalasia.
Barium esophagram showing the typical appearance of a dilated esophagus and “bird's beak” narrowing at the gastroesophageal junction in a patient with achalasia.
Pseudoachalasia is a result of malignant tumor infiltration or other secondary causes, and can present similarly to achalasia causing myenteric plexus damage. Unlike achalasia, this condition has been associated with sudden weight loss later in life, usually after age 50 years. Patients have short duration of symptoms. Tumors capable of infiltrating the myenteric plexus include those of the distal esophagus, gastric cardia, pancreatic, breast, lung, and hepatocellular. Suspected pseudoachalasia should be evaluated with CT or endoscopic ultrasound.
[!NOTE] achalasia: longer sx duration pseudoachalasia: shorter duration, older person
Approaches to treatment of achalasia include endoscopic or surgical intervention with the goal of lowering LES pressure, which relieves symptoms. Medical therapy is uncommonly used.
Endoscopic therapy involves injection of botulinum toxin, pneumatic dilation, or peroral endoscopic myotomy. Botulinum toxin injection into the LES inhibits acetylcholine release, causing LES relaxation. However, after 1 year, only 40% of patients have continued relief of symptoms. Botulinum toxin injection can be repeated, but successive treatments are often less effective for symptom management. Pneumatic dilation is an effective nonsurgical therapy. Dilators ranging from 30 mm to 40 mm in size are used to disrupt the circular muscle. Clinical symptom improvement ranges from 50% to 90%, and the most common complication is perforation. Peroral endoscopic myotomy is a newer endoscopic procedure in which the physician creates an esophageal submucosal tunnel extending to the level of the LES and then performs a myotomy. Studies have shown resolution of symptoms in over 80% of patients. Surgical treatment consists of laparoscopic myotomy of the circular muscle fibers. Fundoplication is also recommended to avoid reflux symptoms after myotomy. Determining whether a patient should receive endoscopic or surgical therapy often depends on local expertise.
Medical therapy is reserved for patients who are poor candidates for endoscopic or surgical therapy. LES pressure can be reduced with medical therapy, including calcium channel blockers (nifedipine) or long-acting nitrates.
Patients with achalasia for more than 10 years have increased risk for squamous cell carcinoma and may benefit from surveillance endoscopy, but there are no established guidelines for frequency of surveillance.