abdominal compartment syndrome
- related: Nephrology
- tags: #nephrology
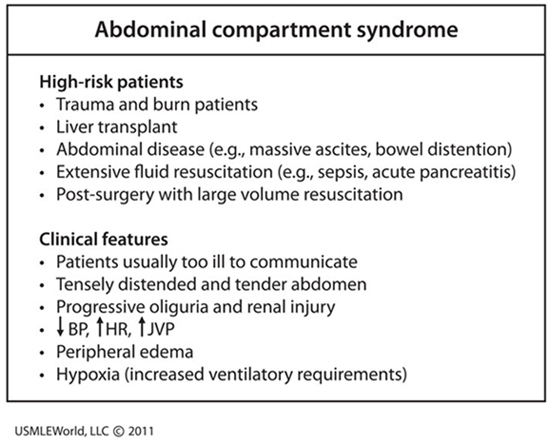
This patient’s presentation is consistent with likely intra-abdominal hypertension (IAH) causing abdominal compartment syndrome (ACS). Intra-abdominal hypertension is defined as pressure > 12 mm Hg; and ACS is defined as IAH with new organ dysfunction. Primary ACS is due to abdominal pelvic disease, while secondary ACS is usually due to extra-abdominal conditions (e.g., burns). Abdominal compartment syndrome occurs in patients receiving large amounts of fluids and almost any organ can be affected (especially the kidney due to its anatomical position).
While the exact pathophysiology is unknown, acute kidney injury is likely due to decreased renal blood flow and elevated renal venous pressure. A diagnosis of ACS can rapidly be confirmed by measuring hydrostatic pressure within the bladder, which is strongly correlated with intra-abdominal pressure. Lowering intra-abdominal hydrostatic pressure often quickly improves renal function; however, most patients require surgical decompression. Abdominal compartment syndrome has a mortality rate ranging as high as 40-100%.
Abdominal compartment syndrome is defined as a sustained intra-abdominal pressure (IAP) >20 mm Hg associated with at least one organ dysfunction. Abdominal compartment syndrome occurs in the setting of abdominal surgery, trauma, hemoperitoneum, retroperitoneal bleed, ascites, bowel obstruction, ileus, and pancreatitis. It can also occur from capillary leak from massive fluid resuscitation or sepsis. Increasing IAP causes hypoperfusion and ischemia of the intestines and other peritoneal and retroperitoneal structures, leading to hemodynamic, respiratory, neurologic, and kidney impairment. Renal vein compression and renal artery vasoconstriction cause oliguric AKI.
Abdominal compartment syndrome is diagnosed by measuring IAP; measurement of bladder pressure with an indwelling catheter is the standard methodology. Management includes supportive therapy, abdominal compartment decompression, and correction of positive fluid balance.