Vulvodynia
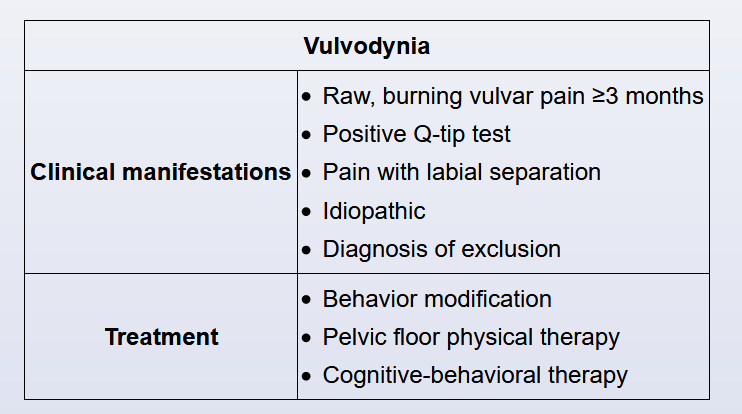
Vulvodynia is a chronic (>3 months), raw, burning vulvar pain that occurs in the absence of a specific disorder (eg, idiopathic). Additional features include dyspareunia, constant irritation, and inability to wear tight-fitting clothing secondary to pain. Patients typically have concomitant depression, irritable bowel syndrome, or fibromyalgia. On physical examination, the external genitalia appear normal and without lesions. Characteristic examination findings include a positive Q-tip test (sharp pain caused by light contact with a cotton applicator) and pain with separation of the labia.
Vulvodynia is due to a combination of physical (eg, pelvic floor muscle dysfunction) and psychological components. Therefore, the management of vulvodynia includes behavioral modifications, pelvic floor physiotherapy, and cognitive behavioral therapy. Pelvic floor physiotherapy decreases the muscle tension associated with vulvodynia, thereby decreasing dyspareunia and chronic pain. Cognitive behavioral therapy is used to reduce stress and anxiety, both of which have been shown to exacerbate symptoms. In addition, patients and their partners can undergo sex therapy or couple-based therapy.
Botulinum neurotoxin-A injection is a treatment option for vulvodynia; however, benefits are temporary. Due to an association with dysphagia and respiratory blockade, it is reserved for patients who have failed first-line treatment (eg, pelvic floor physiotherapy, cognitive behavior therapy).
A 24-year-old woman comes to the office for 3 months of worsening vulvar pain. The patient reports a burning sensation and pain that makes her skin feel "like it is being rubbed raw with sandpaper." The pain prevents the patient from having intercourse or wearing tight-fitting clothing. An over-the-counter antifungal preparation did not improve her symptoms. The patient has had no dysuria, hematuria, or vaginal discharge. She has no other chronic medical conditions and has had no surgeries. All Pap tests have been normal; she has never had a sexually transmitted infection. The patient is using depot medroxyprogesterone acetate for contraception. She drinks alcohol several times a week but does not use tobacco or illicit drugs. The patient has no known allergies. Family history is noncontributory. Blood pressure is 100/60 mm Hg and pulse is 80/min. BMI is 20 kg/m2. On pelvic examination, the external genitalia show no erythema, ulcers, or lesions; light contact of the vulva and labia with a cotton applicator causes sharp pain. Separation of the labia majora for speculum examination causes discomfort; however, insertion of the speculum does not cause vaginal pain. Speculum examination reveals a well-rugated vagina and a normal cervix with no abnormal discharge. A bimanual examination cannot be performed because of patient discomfort. Which of the following is the best next step in management of this patient?