Urinary incontinence
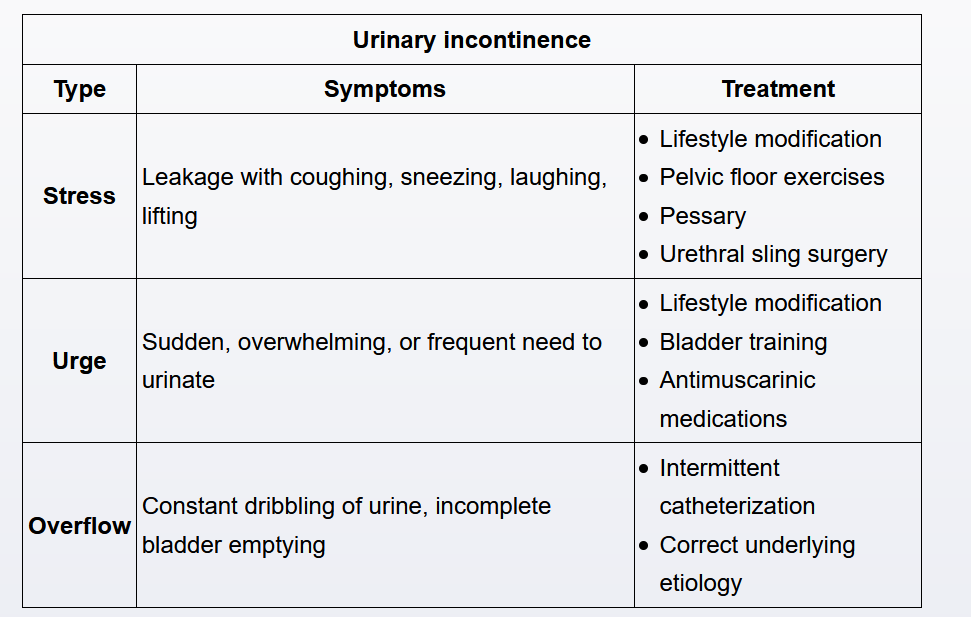
- pathogenesis
- stress: decreased urethral sphincter tone, urethral hypermobility
- urge: detrusor hyperactivity
- overflow: impaired detrusor contractility (DM), bladder outlet obstruction
- treatment
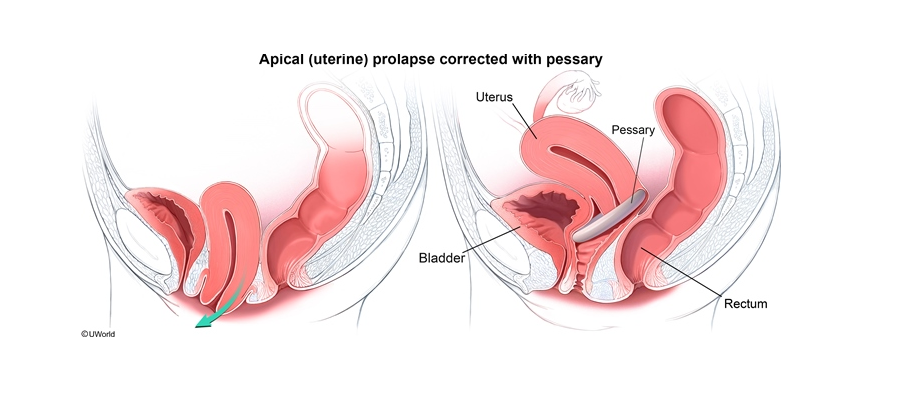
- Stress: kegel, pessary, pelvic floor surgery
- Urge: Antimuscarinic (Oxybutynin)
- Overflow: Muscarinc (Bethanechol, catherterization)
Risk factors for urinary incontinence include increased age, history of multiple vaginal deliveries, obesity, vaginal atrophy, tobacco use, and caffeine intake.
The initial evaluation of patients with urinary incontinence involves a thorough history, physical examination, and urinalysis. Reversible underlying causes of urinary incontinence (eg, excessive fluid intake, stool impaction, medications, delirium) are identified. Physical examination assesses for vulvovaginal atrophy, vesicovaginal fistula, pelvic masses, pelvic organ prolapse, and urethral hypermobility. A bladder stress test (leakage of urine with cough/Valsalva) is performed for evaluation of stress urinary incontinence, as with this patient. Urinalysis evaluates for underlying pathology, including infection or malignancy.
For the majority of patients (including this patient, who has stress incontinence), the initial evaluation is sufficient to classify the type of uncomplicated urinary incontinence (eg, stress, urgency, overflow) and no further evaluation is indicated. Further evaluation is indicated only if the history, physical examination, or urinalysis suggest complicated incontinence (eg, mixed) or underlying pathology.
Urge
Urge incontinence: Although the detrusor overactivity is typically idiopathic, it can be caused by neurologic disease (eg, multiple sclerosis) or bladder abnormalities. Risk factors for urgency incontinence include increasing age, stroke, depression, diabetes mellitus, obesity, caffeine intake, and tobacco abuse.
Overflow
Overflow incontinence is typically a complication of poorly controlled diabetes mellitus (eg, diabetic neuropathy) and presents with constant urinary dribbling from incomplete bladder emptying. Patients with features of overflow incontinence (eg, peripheral or perineal neuropathy) are evaluated with a post-void residual volume (>200 mL is diagnostic of overflow incontinence). Additional evaluation with a hemoglobin A1c can be performed to either diagnose diabetes mellitus or assess blood glucose control. This patient has no features of overflow incontinence; therefore, neither a post-void residual volume nor hemoglobin A1c is indicated.
Tricyclic antidepressants (TCAs) (eg, amitriptyline) inhibit reuptake of serotonin and norepinephrine and are used to treat depression, anxiety, chronic pain syndromes, and eating disorders. TCAs have antimuscarinic (eg, urinary retention, dry mouth, constipation), antihistamine (eg, sedation), and anti–alpha adrenergic (eg, hypotension, tachycardia) effects. This patient's 3-month-history of overflow incontinence is likely due to her recent change in antidepressants (ie, starting a TCA) 4 months ago. TCAs are not generally recommended in the elderly due to the increased risk of falls and injury, and dosing is tapered to minimize side effects.
Patients with overflow incontinence, due to either detrusor underactivity (eg, TCAs) or bladder outlet obstruction (eg, prolapse), exhibit continuous urinary leakage, a palpable lower abdominal mass (due to the persistently full bladder), and an elevated postvoid residual. Treatment focuses on addressing the underlying cause (eg, medication change, lifestyle modifications, correction of prolapse) and intermittent bladder catheterization.
Urodynamic testing evaluates urethral and bladder function and pressure and is indicated in the evaluation of mixed or complicated urinary incontinence.
Patients who have no improvement in their urgency incontinence symptoms despite lifestyle modifications (eg, bladder training) may benefit from the addition of an antimuscarinic medication such as tolterodine, solifenacin, or oxybutynin. Antimuscarinic medications improve bladder capacity and inhibit detrusor muscle contraction during bladder filling by blocking acetylcholine release in the bladder. The anticholinergic properties of these medications frequently result in side effects (eg, dry mouth, constipation, drowsiness, blurry vision) that may limit their usefulness. To minimize these side effects, antimuscarinics are initiated at the lowest dose and titrated up as tolerated. Patients with persistent incontinence symptoms despite the use of antimuscarinic medication can be considered for botulinum toxin injections or percutaneous tibial nerve stimulation.
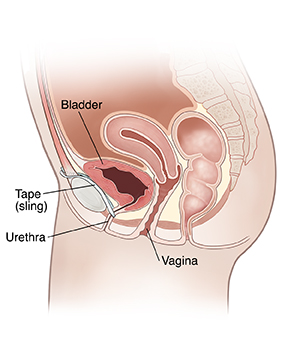
A mid-urethral sling procedure is indicated in the management of stress urinary incontinence, which presents with involuntary leakage of urine associated with increased intraabdominal pressure. Patients with stress incontinence have a positive cough-stress test (ie, leakage with coughing).
The sling (tape) is made from a mesh of artificial material. When the tension of the tape is changed, urine should no longer leak.