Therapeutic Principles in Dermatology
- related: Dermatology
- tags: #dermatology
General Considerations
The effectiveness of a topical medication depends largely on its ability to be absorbed through the skin. Absorption is dependent on the chemical structure of the medication, its concentration, skin hydration, skin thickness, and the delivery vehicle.
In general, ointments have a higher potency than creams, which in turn have a higher potency than solutions or suspensions. The various vehicles that are available are listed in Table 3. Creams rub in and dissipate without leaving a residue, and patients tend to favor their use. The alcohol content and drying nature of gels can cause burning and stinging on non-intact skin. An occlusive vehicle such as an ointment increases penetration, but adherence may be low because of its greasy feel.
Table 4 outlines the various categories of topical medications, including those most frequently used and the indications for which they are used.
Topical Glucocorticoids
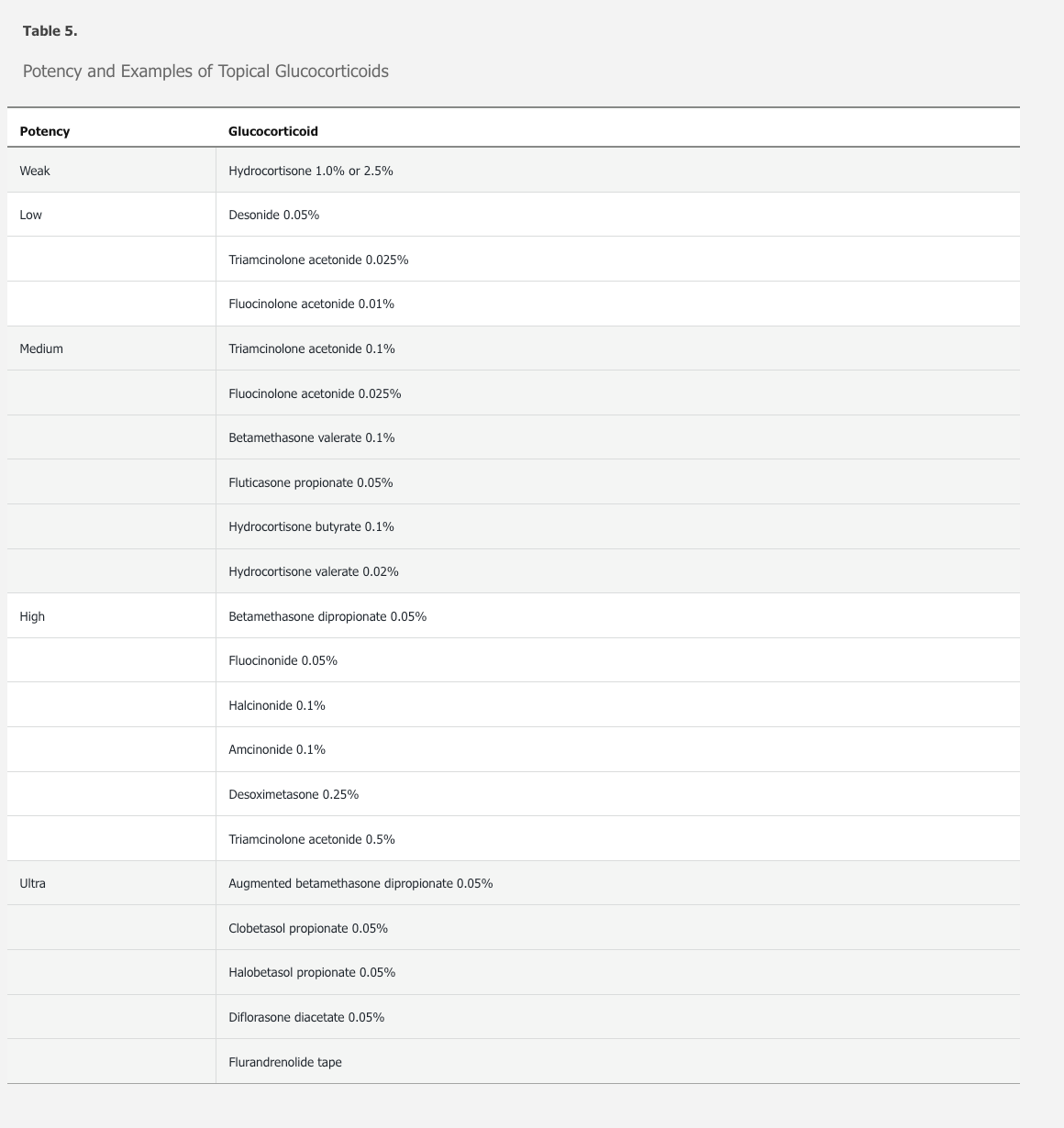
Topical glucocorticoids are used for their anti-inflammatory effects. Because they are applied directly to the area of involvement, systemic adverse effects are minimized. Topical glucocorticoids are classified by their potency level. One should become comfortable with one in each class from weak to ultra-potent. There is a generic equivalent in each class, allowing for a cost-effective approach (Table 5).
In general, twice-daily dosing is the most common dosing schedule, and the medication should be applied in a thin film. A rule of thumb is that 30 grams of a topical glucocorticoid will be enough to cover the entire surface of a 70 kg adult, once. Proportionately less is needed for smaller areas.
Topical glucocorticoids may cause striae, easy bruising, atrophy, and telangiectasia. Side effects are most frequently seen when using higher potencies for longer periods of time; in areas of thin skin (such as the face); skin folds; or when used under occlusion. Use of glucocorticoids around the eyes can exacerbate glaucoma and cause cataracts.
Topical Antifungal Agents
Topical antifungal agents are used to treat tinea or candida infections. Topical azole antifungal agents are suitable for treatment of localized infection, whereas oral agents are used to treat recurrent, recalcitrant, or widespread disease.
Topical glucocorticoids are frequently commercially combined with topical antifungal agents (clotrimazole-betamethasone). These combinations should be avoided. The use of a combination drug can worsen some tinea infections and when used in the groin area has a high risk of causing striae.
Topical Immunomodulators
Topical immunomodulators (tacrolimus ointment and pimecrolimus cream) can be used in place of topical glucocorticoids on the face, in skin folds, or in occlusive areas of the body (axilla/groin) for an extended period of time without the development of atrophy, striae, and telangiectasia. These medications have a black box warning for the rare development of skin cancer and cutaneous lymphoma.
Topical Retinoids
Topical retinoids are used frequently in the treatment of acne and psoriasis. They are vitamin A analogues with effects on keratinocyte proliferation and differentiation. Use should be avoided in pregnancy due to the risk of teratogenicity.
Topical Antibiotics
Clindamycin and erythromycin are two topical antibiotics used in the treatment of acne. They are well tolerated and have few to no side effects. Bacterial resistance has been shown to occur when using the agents as solo therapy. The combination of benzoyl peroxide and a topical antibiotic has shown to limit bacterial resistance. Over-the-counter combination antibiotics are used frequently. They typically have minimal side effects. The most frequent side effect is allergic contact dermatitis. This is seen with neomycin and bacitracin.
Phototherapy
When taken 2 hours before ultraviolet A (UVA) light exposure, oral psoralen increases the absorption of UVA. Historically, the combination of psoralen plus UVA (PUVA) phototherapy for the treatment of psoriasis has been shown to be effective but significantly increased the risk for developing skin cancer. Newer phototherapy units using a narrow band of ultraviolet B (UVB) has been shown to be safe and effective with a much smaller risk of skin cancer.
Narrowband ultraviolet B (UVB) therapy has become the standard form of phototherapy used in the initial treatment of psoriasis. The light source emits a narrow band of UVB radiation, in this case 311 nm of ultraviolet light. This wavelength was chosen for its efficacy and the fact that this wavelength of light is not absorbed by DNA. The theory is that if the light is not absorbed by DNA, less skin damage will occur, and there will be far fewer skin cancers as a side effect of the therapy. Broadband UVB was the mainstay of therapy until the advent of narrowband UVB. Broadband is still used in some centers today. Broadband UVB emits light in the 280 to 320 nm range; 260 nm is the wavelength of light with the maximum absorption by DNA. DNA absorption of UVB drops off dramatically after 290 nm. Broadband UVB contains wavelengths of light capable of causing DNA damage, leading to ultraviolet skin damage and ultimately skin cancer.
Psoralen plus ultraviolet A (PUVA) therapy is now used almost exclusively for the treatment of cutaneous T-cell lymphoma. It is effective for treating psoriasis, but it has been shown to cause an increase in the risk of nonmelanoma and melanoma skin cancer. For these reasons, it is not used as first-line therapy for psoriasis.