Testicular Pathology
Most common type of testicular tumor (>95% of cases), and they usually occur between 15-40 years of age.
Patients will often present with a firm testicular mass that cannot be transilluminated. (hypoechoic)
Can be classified as one of the following types:
- Seminoma (55% of cases) are highly responsive to radiotherapy, metastasize late, and have an excellent prognosis.
- Nonseminomas (45% of cases) show variable response to treatment and often metastasize early
- Yolk sac tumors
- Embryonal carcinoma and teratoma
- Choriocarcinoma.
Tumor markers:
- Yolk sac: high AFP
- Choriocarcinoma: high b-HCG
- embryonal, teratoma: high AFP or b-HCG
- seminoma: high ALP and rarely HCG..
The risk factors for germ cell tumors of the testicle include the following:
- Cryptorchidism (most common)
- **Androgen Insensitivity **
- Family history of testicular cancer
- **Down Syndrome **
- Klinefelter syndrome.
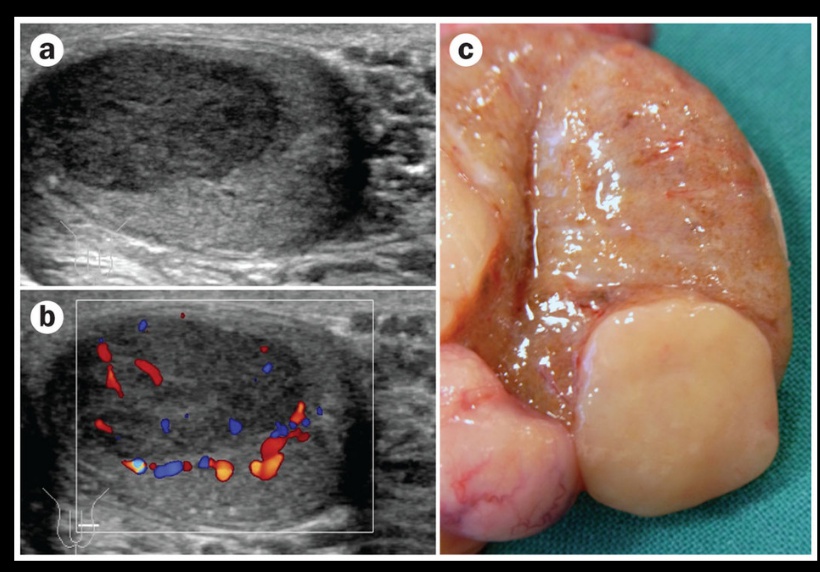
The diagnosis of testicular cancer is often made with ultrasound, which reveals a hypoechoic intratesticular mass..
Seminoma
The most common testicular tumor (40%) that originates in the germinal epithelium or the seminiferous tubules.; resembles ovarian dysgerminoma.
Testicular ultrasound showing a hypoechoic intratesticular mass.
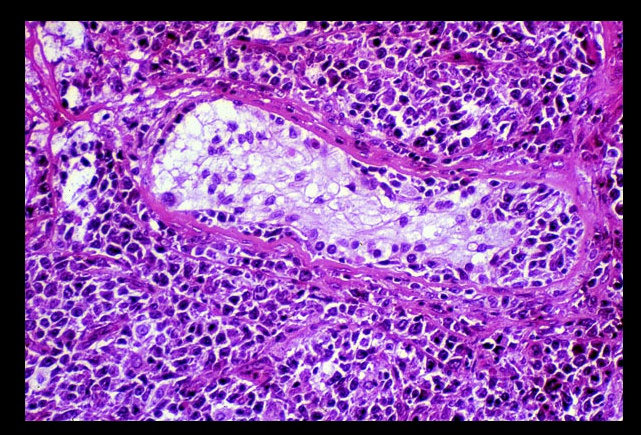
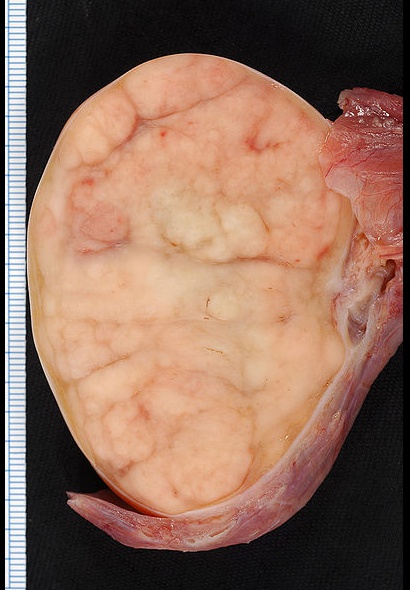
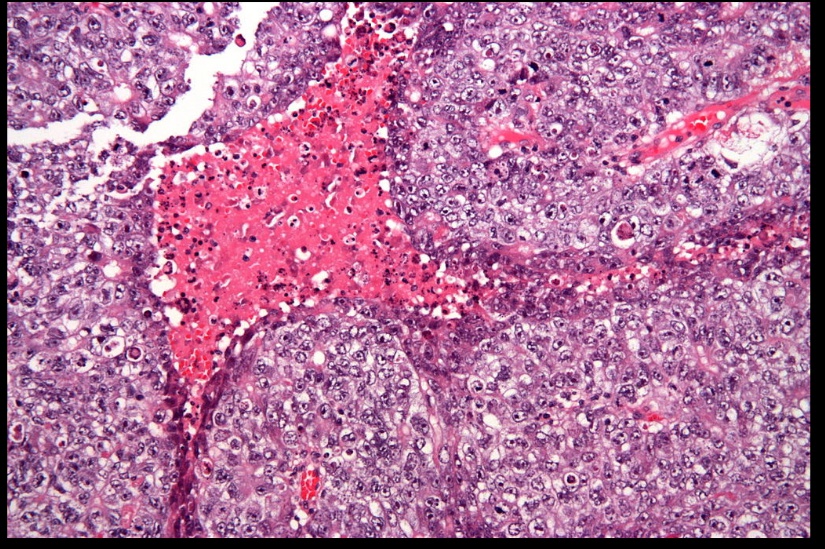
On histology will reveal clear, polygonal germ cells with round nuclei and prominent nucleoli that are arranged into lobules and surrounded by septa. There is often a lymphocytic infiltrate and granulomas. Grossly these tumors appear as a bulky, gray tumor without hemorrhage or necrosis.
lymphocytic infiltrate:
Most commonly present with painless testicular enlargement.
Highly radiosensitive and have an excellent prognosis with treatment. Later stage neoplasms often require surgical resection (orchidectomy)..
Embryonal Carcinoma
Rare malignant tumor comprised of immature, primitive cells that form papillary/glandular structures. Metastasis is commonly hematogenous.
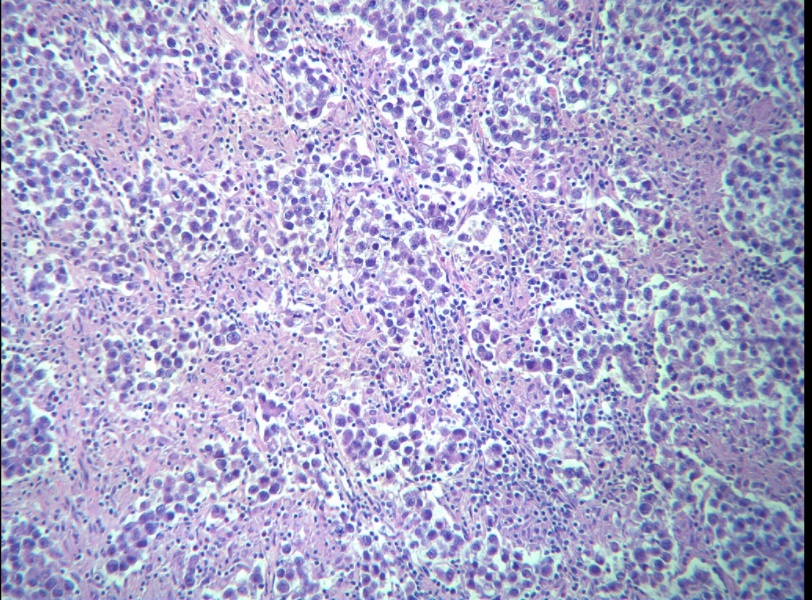
On histology will appear as sheets of undifferentiated cells with marked nuclear atypia, prominent nucleoli, and focal glandular differentiation or papillary morphology.
Neoplastic cells displaying nuclear atypia, prominent nucleoli, and necrosis.
Gross appearance is a pale grey, bulky, hemorrhagic and necrotic tumor.

Are less radiosensitive than seminomas, and also more aggressive with an intermediate prognosis. Chemotherapy may result in differentiation into another type of germ cell tumor (e.g. teratoma).
The clinical presentation includes the following:
- Palpable testicular mass
- Painful. (Note: this is different from other testicular tumors, which are usually painless)
Choriocarcinoma
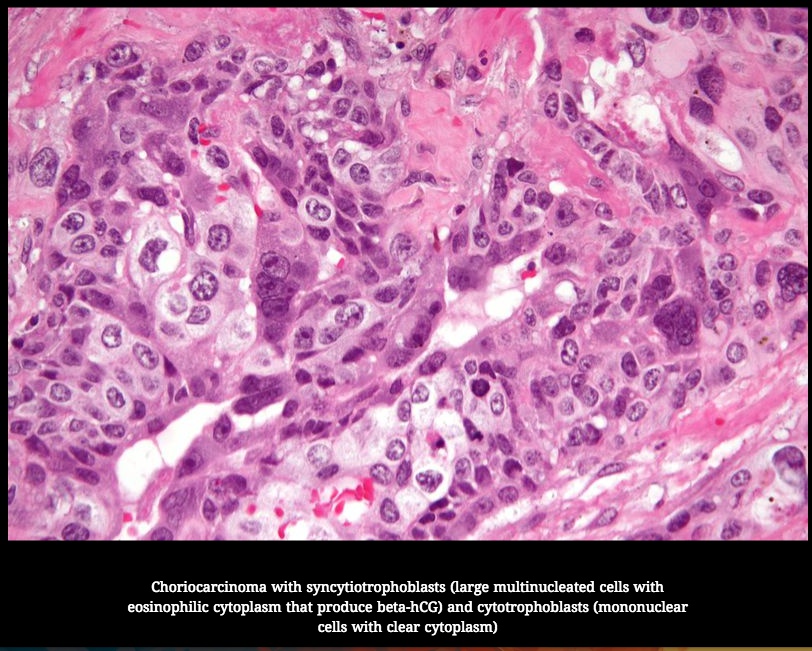
Malignant tumor of syncytiotrophoblasts and cytotrophoblasts (placenta-like tissue, but villi are absent). It is the most aggressive testicular tumor; poor prognosis..
On histology reveal mixed proliferation of syncytiotrophoblasts (large multinucleated cells with eosinophilic cytoplasm that produce beta-hCG) and cytotrophoblasts (mononuclear cells with clear cytoplasm)..
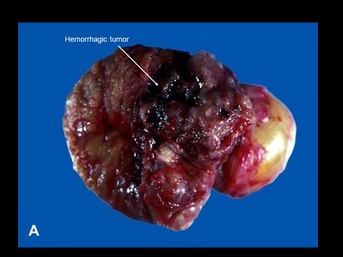
The gross appearance is a small primary tumor with extensive necrosis and hemorrhage.
Tumor marker used to monitor and/or confirm the diagnosis is an elevated hCG (human chorionic gonadotropin) in nearly 100% of cases. This may present as gynecomastia, because if you recall hCG has a similar alpha subunit as LH (↑ LH → breast development)
The alpha-subunit of beta-hCG is similar to the alpha-subunit of LH, FSH, and TSH. This can result in hyperthyroidism. The beta-subunit is the unique subunit to each hormone, and is responsible for the majority of their physiologic effects.
Commonly metastasize hematogenously, most commonly to the lungs (causing hemoptysis), brain (causing hemorrhagic stroke), and liver.
Testicular Teratomas
In males are malignant (often squamous cell malignancy). This is important to remember, because the mature teratoma (dermoid cyst) in females is benign..
aka dermoid cyst.
Non Germ cell
Resemble sex cord-stromal tissues of the testicle, and they are usually benign. The two most common types are Leydig cell and Sertoli cell tumors..
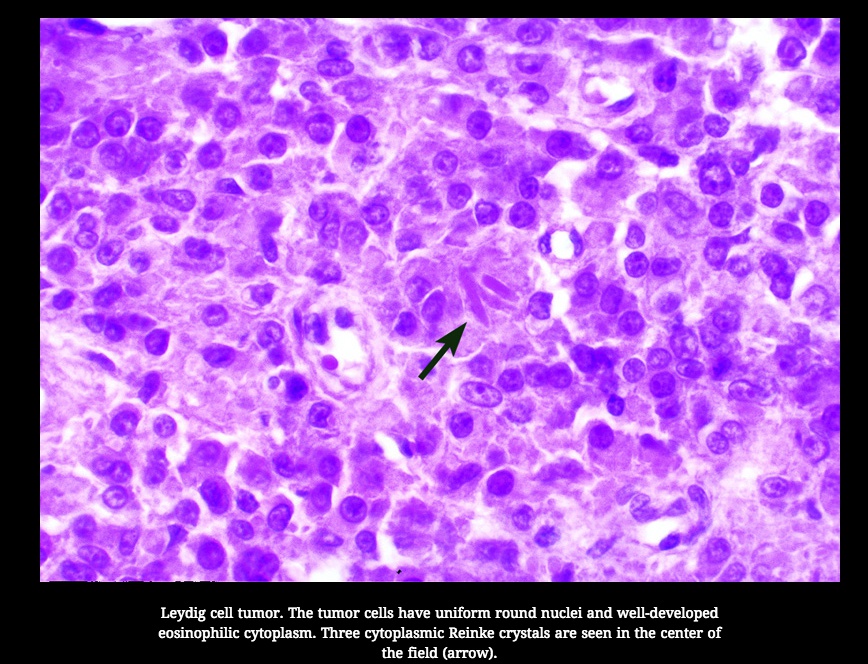
Leydig cell tumor
Benign tumor of Leydig cells that produces androgens and may also produce estrogens..
Patient presentation will depend on age; precocious puberty in children and gynecomastia in adult men.
A characteristic finding on microscopy is intracytoplasmic Reinke crystals(rod-shaped crystals) within the neoplastic Leydig cells..
Sertoli Cell Tumor
Benign tumor of Sertoli cells that is comprised of tubules. It most commonly does not produce hormones and therefore presents as a testicular mass..
Testicular Lymphoma
Most common cause of testicular cancer found in males >60 years old. They are often bilateral, and arise due to metastasis.
Diffuse large B cell Non-Hodgkin
The most common testicular lymphoma subtype.