TTP
- related: Hemeonc
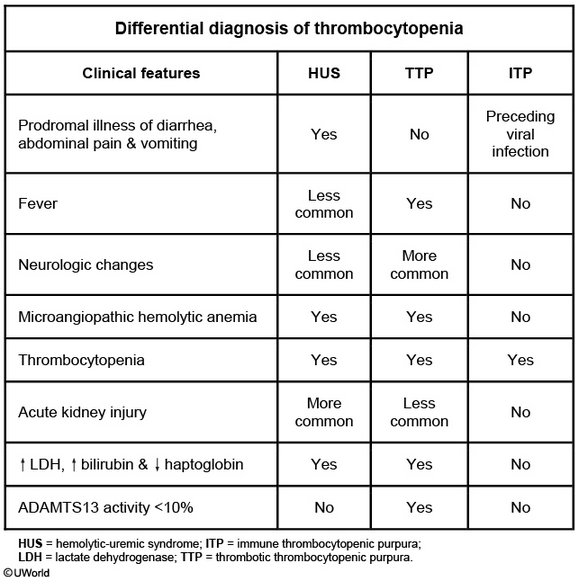
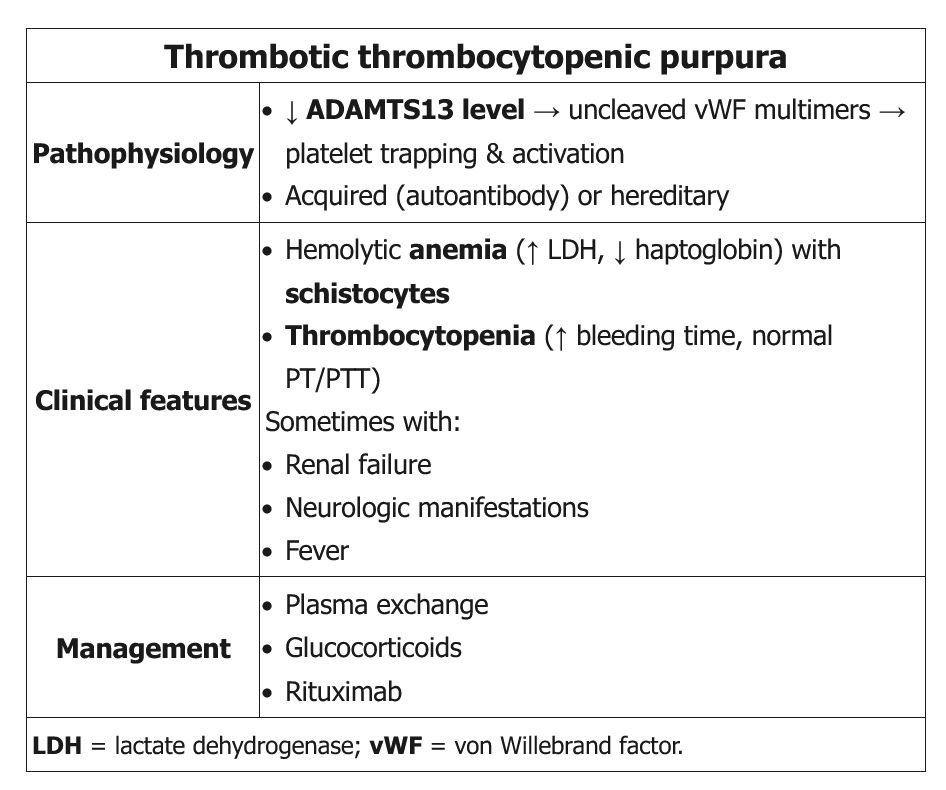 This patient likely has thrombotic thrombocytopenic purpura (TTP), which is characterized by the formation of small-vessel, platelet-rich thrombi due to severe deficiency of the von Willebrand factor–cleaving protein ADAMTS13. TTP can be associated with pregnancy due to the formation of autoantibodies (acquired) or the emergence of a previously unknown heredity case.
This patient likely has thrombotic thrombocytopenic purpura (TTP), which is characterized by the formation of small-vessel, platelet-rich thrombi due to severe deficiency of the von Willebrand factor–cleaving protein ADAMTS13. TTP can be associated with pregnancy due to the formation of autoantibodies (acquired) or the emergence of a previously unknown heredity case.
Patients with TTP can be minimally symptomatic or critically ill but classically have:
- Severe thrombocytopenia (median platelet count ~10,000/mm3)
- Microangiopathic hemolytic anemia (MAHA) - schistocytes on peripheral blood smear
- Organ dysfunction - thrombi-induced ischemia can lead to neurologic manifestations (eg, confusion, headache) and mild renal insufficiency (creatinine usually <2 mg/dL)
Diagnostic evaluation usually reveals normal coagulation studies (unlike disseminated intravascular coagulation [DIC]), negative Coombs testing, and ADAMTS13 levels of <10%. Urgent treatment with plasma exchange, glucocorticoids, and rituximab are required to prevent death.
Pathogenesis
- ADAMTS13 cleaves VWF on endothelial cell and prevents platelet clotting
- ADAMTS13 antibody prevents above process, inactivates or destroys platelets
Sx
- neurologic sx, rash, AKI, chest pain, abdominal pain
Dx
- DIC panel
- smear: schistocytes
- ADAMTS13 < 10%
Rx
- empiric
- plasmapheresis:
- centrifuge
- removes plasma with immunoglobulins
- not good at removing IgG
- add donor plasma
- plasma transfusion
- pulse dexamethasone: decrease antibody
- rituximab
- aspirin
- caplacizumab
It is rare for a patient with TTP to have the full classic pentad (fever, MAHA, thrombocytopenia, renal failure, and neurologic symptoms). The presence of MAHA and thrombocytopenia (not due to other causes) is enough to diagnose suspected TTP and initiate treatment with plasma exchange (even without fever, as in this patient). Measurement of ADAMTS13 activity is not required to make the diagnosis. Replacement of ADAMTS13 via plasma exchange stabilizes and improves most cases of idiopathic TTP. Failure to institute timely therapy can lead to devastating end-organ consequences. Initiating plasma exchange therapy while waiting for additional test results is the most appropriate next step in management. Patients refractory to plasma exchange therapy may respond to rituximab or cyclosporine.
Corticosteroids and other immunosuppressive drugs may reduce antibody formation in idiopathic TTP or prevent bleeding when the platelet count is very low. These are usually given as an adjunct to plasma exchange or later in the course of the disease pending initial response to plasma exchange.