Sickle cell disease
Pathogenesis

Symptoms
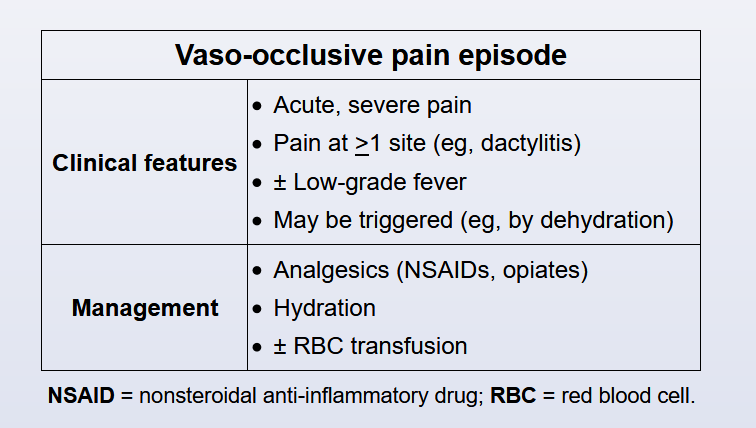
This patient with symmetric swelling and pain of the hands and feet in the setting of known sickle cell disease (SCD) has dactylitis (hand-foot syndrome). Dactylitis, resulting from vaso-occlusion of the blood vessels supplying the metacarpals and metatarsals, may be the earliest manifestation of SCD in young children (ages 6 months to 4 years). Similar to other vaso-occlusive episodes, triggers include stress, illness, temperature changes, and dehydration. Low-grade fever may also be present in addition to pain. Initial radiographs reveal only soft-tissue swelling; recurrent episodes can lead to a mottled appearance of the bones. Although most children with SCD are diagnosed by hemoglobin electrophoresis on newborn screening, the presence of dactylitis in a previously healthy child should prompt evaluation for SCD.
Labs
Baseline changes:
- increased bilirubin, reticulocytes
- decreased Hgb
- chronic pain
Diagnosis
- prenatal screen
- CBC: sickle cells
- Hgb electrophoresis
Treatment
Treatment of dactylitis involves pain control, hydration, and application of heat. Oral nonsteroidal anti-inflammatory drugs (NSAIDs) and oral opioids are typically initiated for mild to moderate pain. Because this patient still appears uncomfortable after treatment with NSAIDs, a short-acting oral opioid (eg, oxycodone) should be given. If the pain fails to improve, intravenous opioids are indicated.
(Choice A) Cold compresses are not recommended as they can trigger local intravascular sickling and worsen vaso-occlusive pain episodes. In contrast, heat packs help by promoting vasodilation.
(Choices B and E) Oral codeine and tramadol are contraindicated in children age <12 because ultra-rapid metabolism of codeine and tramadol causes an unpredictably high concentration of the active drug in the body, which can result in respiratory depression and death.
(Choice C) Hydroxyurea reduces the frequency of vaso-occlusive episodes in patients with SCD but may take several months to take effect. It is not used in the treatment of an acute vaso-occlusive episode.
Acute Chest Syndrome
This patient, who initially presented with sickle cell pain crisis, now has symptoms suggestive of acute chest syndrome (ACS). ACS is defined as a new infiltrate on chest x-ray plus any of the following: fever; chest pain; or respiratory symptoms such as cough, wheezing, decreased oxygen saturation, tachypnea, or accessory respiratory muscle usage. Important etiologies for ACS are infection, asthma, hypoventilation, and pulmonary vasoocclusion from fat emboli. Negative chest x-rays obtained during initial presentation do not rule out subsequent development of ACS. ACS usually occurs within 48-72 hours of admission for pain crisis.
Patients admitted for sickle crisis should be considered to be in the prodromal phases of ACS. Prophylactic measures such as close pulmonary monitoring, cautious hydration, optimal pain control, and incentive spirometry remain essential components of therapy.
Treatment of ACS is based on severity. Simple transfusion for mild ACS and exchange transfusion for moderate-to-severe ACS are recommended with a target Hb of 10 g/dL. ACS and pneumonia are difficult to differentiate from each another. Therefore, empiric antibiotics that include coverage for atypical organisms (eg, Chlamydia and Mycoplasma) must be administered. However, prophylactic use of antibiotics to prevent ACS is not recommended. Hydroxyurea should also be started for all patients with a history of ACS or at risk of developing it (eg, HbSS).
Hypotonic fluids (1/2 normal saline or D51/2 normal saline) are recommended for acute sickle cell crisis. Adequate intravenous fluids are important to reduce sickling, but excess use for prolonged periods can cause pulmonary edema. This patient had received 125 mL/hr for 36 hours with good urine output, which should not lead to pulmonary edema.
Stroke prevention
Strokes in SCD are primarily caused by vascular clogging due to high concentrations of hemoglobin S (Hb S). Therefore, acute strokes are typically managed with urgent exchange transfusion to rapidly reduce Hb S levels. Secondary prophylaxis against recurrent stroke must then be provided using chronic simple transfusion therapy every 4-6 weeks with goal Hb S levels of <30% and total Hb levels of 9-12.5 mg/dL. This strategy reduces the risk of stroke recurrence from 65% to <20% and is superior to medical management with hydroxyurea.
Exchange transfusion is primarily used for patients with SCD who have acute ischemic stroke. Exchange transfusion is expensive and time consuming, requires a catheter, and involves more blood than simple transfusion. As a result, it is not typically used for chronic therapy.
Patients receiving chronic transfusions must be monitored for iron overload; periodic chelation therapy is often required to prevent iron-related morbidity (eg, hepatic fibrosis, cirrhosis).
Nimodipine is a calcium channel blocker that can reduce vasospasm in patients with subarachnoid hemorrhage, which is also a complication of SCD. However, nimodipine is not used for stroke prevention.
Although aspirin is commonly prescribed to patients with SCD who have had a stroke, there is no evidence that it is an effective monotherapy for stroke prevention in SCD as it does not reduce Hb S levels.
Rivaroxaban is a factor Xa inhibitor used primarily to treat deep venous thrombus/pulmonary embolus or to prevent stroke in those with atrial fibrillation. Because strokes in SCD are primarily mediated by high concentrations of Hb S, factor Xa inhibitors are not effective for secondary prophylaxis.