Postpartum thyroiditis
This patient's clinical features (eg, anxiety, palpitations, weight loss, decreased lactation, tremor, moist skin) and suppressed TSH are consistent with thyrotoxicosis. In light of her recent pregnancy, this is most likely due to postpartum thyroiditis (PT). PT is characterized by autoimmune inflammation of thyroid follicles and release of preformed thyroid hormone. It is similar to silent thyroiditis but by definition occurs within a year of pregnancy. Both PT and silent thyroiditis are associated with a positive thyroid peroxidase (TPO) antibody assay and are considered variants of chronic lymphocytic (Hashimoto) thyroiditis. PT is more common in women with preexisting autoimmune thyroid disorders and other autoimmune endocrinopathies (eg, type 1 diabetes mellitus) and women may have recurrences with subsequent pregnancies.
Many of the features of hyperthyroidism in PT are mediated by increased responsiveness to catecholamines. Patients with only mild symptoms may not need specific treatment, but those with bothersome symptoms should be treated with beta blockers (eg, atenolol, propranolol). Although most beta blockers are excreted in breast milk in small amounts, their use during lactation is acceptable with close monitoring of the child.
Postpartum thyroiditis (PT) typically follows a triphasic course, with a 1- to 3-month hyperthyroid phase, followed by hypothyroidism for 4-6 months and an eventual recovery to a euthyroid state within a year. Some patients may have only transient thyrotoxicosis or transient hypothyroidism.
However, a significant minority of patients (20%-40%) may develop persistent or recurrent hypothyroidism with a palpable goiter, similar to classic chronic lymphocytic (Hashimoto) thyroiditis (Choice E). Patients with a more severe initial hypothyroid phase or a high titer of antithyroid peroxidase antibody are at increased risk. In light of this, patients with PT should be counseled on the symptoms of hypothyroidism, and some experts advise annual measurement of TSH.
Because patients with PT are unlikely to develop chronic hyperthyroidism, there is no indication for radioiodine therapy or thyroidectomy.
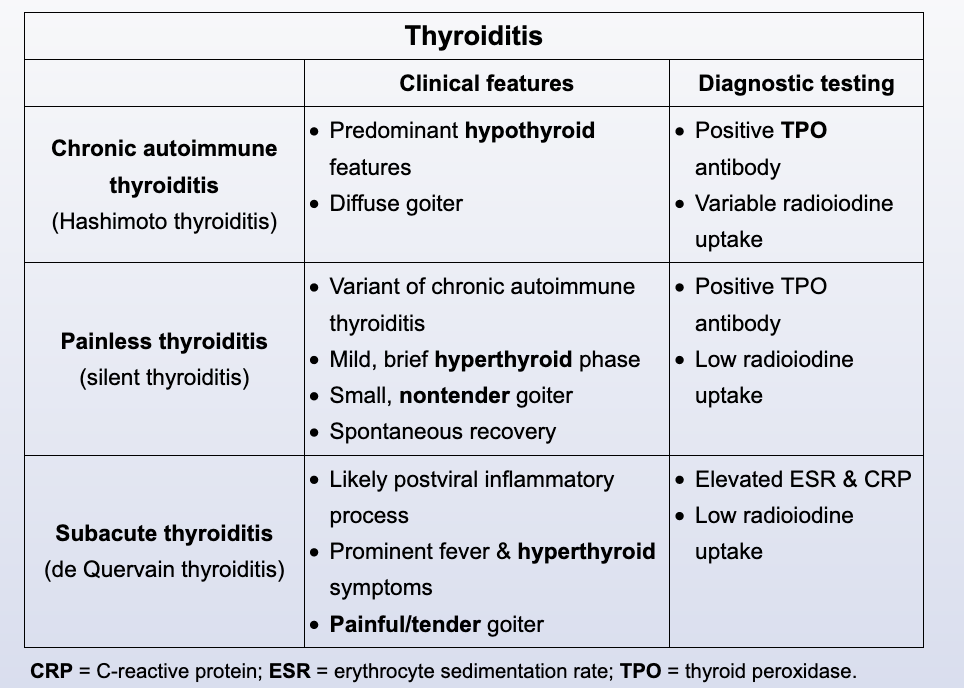
This patient has primary hyperthyroidism (elevated T4, suppressed TSH). In light of her nontender goiter and recent pregnancy, this is consistent with postpartum thyroiditis (PT). PT (by definition occurring <1 year following pregnancy) is similar to silent thyroiditis; both are associated with thyroid peroxidase antibody and are considered variants of chronic lymphocytic (Hashimoto) thyroiditis. Both PT and silent thyroiditis typically have a transient hypothyroid phase before returning to a normal euthyroid state, whereas most patients with classic Hashimoto thyroiditis have residual hypothyroidism.