PF ratio
- related: Pulmonology
OVERVIEW
PaO2/FiO2 ratio is the ratio of arterial oxygen partial pressure (PaO2 in mmHg) to fractional inspired oxygen (FiO2 expressed as a fraction, not a percentage)
- also known as the Horowitz index, the Carrico index, and (most conveniently) the P/F ratio
- at sea level, the normal PaO2/FiO2 ratio is ~ 400-500 mmHg (~55-65 kPa)
- MD Calc is an example of an online P/F ratio calculator – however it is quite easy to do “in your head”
P/F ratio is a widely used clinical indicator of hypoxaemia, though its diagnostic utility is controversial.
ALTERNATIVES TO P/F RATIO
Alternative indices of oxygenation include:
- Oxygen saturations in arterial blood (SpO2 and SaO2)
- S/F ratio (SpO2 to FiO2 ratio)
- PaO2 (arterial oxygen tension)
- A-a gradient (difference between alveolar oxygen tension (PAO2) and PaO2)
- Oxygenation index (OI) (the reciprocal of P/F times mean airway pressure (MAP): OI = (FiO2×MAP)/PaO2)
- P/FP Ratio (PaO2/(FiO2 X PEEP)
- a/A ratio (ratio of PaO2 and PAO2)
- Respiratory index (RI) (RI = pO2(A-a)/_p_O2(a), ie. the A-a gradient divided by the PaO2; normal RI is <0.4)
- Shunt fraction
ADVANTAGES OF P/F RATIO
- Quick and simple (probably the main reason for it’s widespread use)
- can be used as a rough guide to whether there is a significant A-a gradient present:
- PaO2 should = FiO2 x 500 (e.g. 0.21 x 500 = 105 mmHg)
- see caveats below
- More practical than the a/A ratio, as measurement of alveolar oxygen tension (PAO2) is not required
- Used in severity scoring systems
- e.g. APACHE IV, SOFA, SAPS-II and SAPS-III
- e.g. SMART-COP risk score for intensive respiratory or vasopressor support in community-acquired pneumonia (P/F ratio <333 mmHg if age <50y or PF ratio <250mmHg if age >50y)
- e.g. part of the Berlin definition of Acute Respiratory Distress Syndrome (ARDS) (P/F ratio <300mmHg), and correlates with mortality (see below)
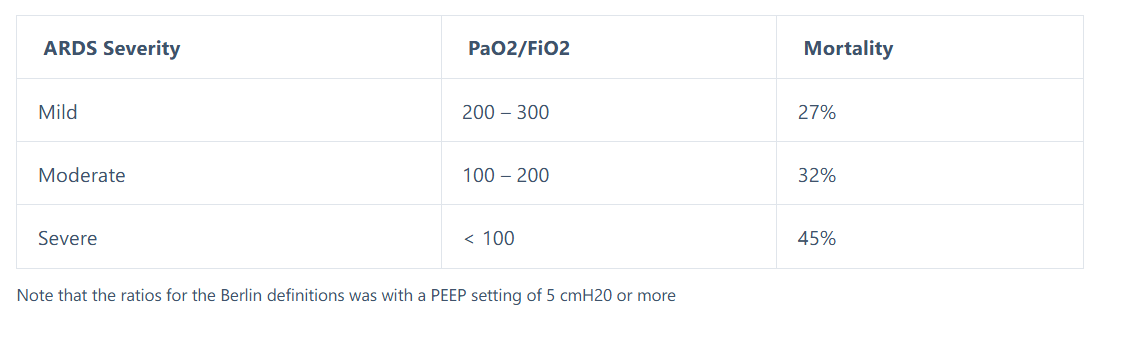
Note that the ratios for the Berlin definitions was with a PEEP setting of 5 cmH20 or more
DISADVANTAGES OF P/F RATIO
-
A better P/F ratio may not be associated with better outcomes
- e.g. In the ARDSNet ARMA study the high tidal volume strategy had better P/F ratios, but worse outcomes
-
P/F ratio is dependent on barometric pressure (it is a as a “tension-based index”)
- normal lungs (with a normal A-a gradient) will have lower PF ratios at high altitude and higher PF ratios at supra-atmospheric pressures
-
P/F ratio alone cannot distinguish hypoxaemia due to alveolar hypoventilation (high PACO2) from other causes such as V/Q mismatch and shunt
- whereas A-a gradient based indices (e.g. a/A ratio and RI) can exclude alveolar hypoventilation
- as shunt increases, the PaO2 tends to become less and less sensitive to the PAO2 and to the FIO2, and more dependent on the mixed venous O2 content and saturation
-
markedly dependent on FiO2
-
May be unreliable unless FiO2 > 0.5 and PaO2 < 100 mmHg
-
variation occurs with both right-to-left shunt (e.g. ARDS) and with widespread V/Q scatter (e.g. COPD)
-
varies with degree of shunt present – increasing the FIO2 causes the PaO2/FIO2 ratio to rise if intrapulmonary shunt is small, but to drop if the shunt is large
-
as a result, P/F ratio will vary according to the chosen SpO2 (and hence PaO2) target, as the required FiO2 will vary
-
-
does not account for mean airway pressure or PEEP
- The Oxygenation Index (OI) may be a more accurate measure of oxygenation dysfunction in ventilated patients as it accounts for mean airway pressure
- P/FP Ratio adjusts the P/F ratio for the set PEEP
-
requires and arterial blood gas measurement
- S/F ratio tends to correlates with P/F ratio and is non-invasive
-
highly dependent on CaO2-CvO2 (oxygen extraction)
- arterial blood may appear well oxygenated despite lung dysfunction if mixed venous oxygen tension is high due to poor oxygen extraction by tissues, e.g. sepsis
- P/F ratio may appear worse due to high oxygen extraction ratio (e.g. cardiogenic shock)
-
does not indicate oxygen content of the blood (dependent on haemoglobin) or oxygen delivery to tissues ( dependent on cardiac output and oxygen content)
RULE OF THUMB FOR USE OF P/F RATIO
P/F ratio should only be used as a rule of thumb for detecting an A-a gradient when:
- the PaCO2 is normal, and
- shunt is not suspected
The FiO2 used should always be specified.
A quick comparison of the patient’s PaO2 to the product of “500 x FiO2” is a magic trick for estimating a-A gradient that should be in the arsenal of every intensivist!