Normal pregnancy
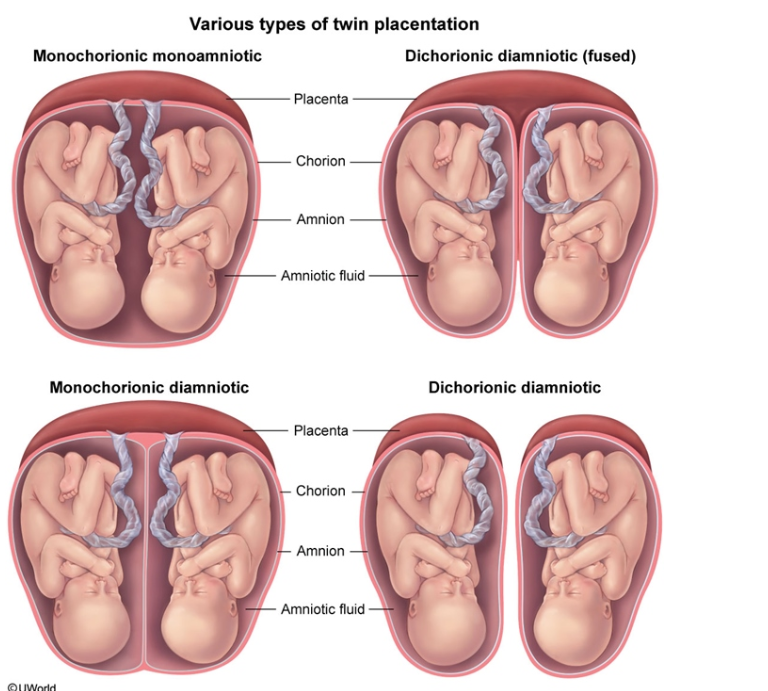
Types of twins
Pemphigoid gestionis
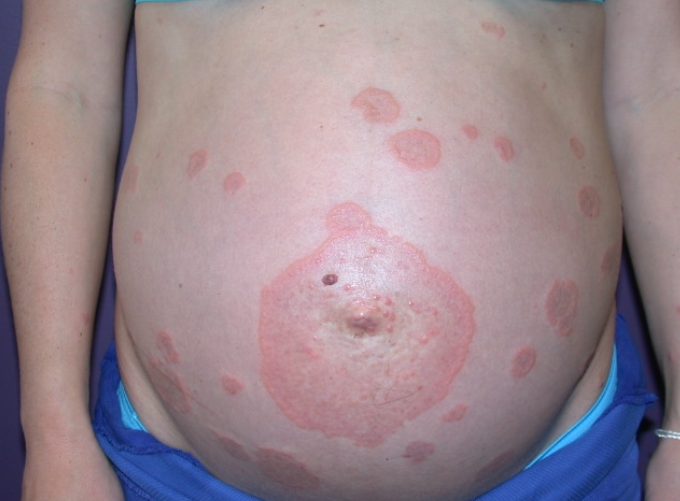
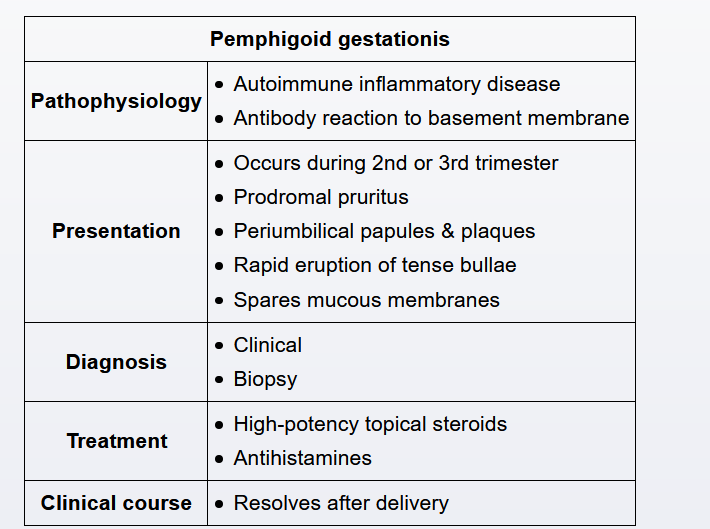
Pemphigoid gestationis (previously called herpes gestationis) is an autoimmune disease that typically presents in the second or third trimester with pruritus that precedes a truncal rash. The characteristic rash of pemphigoid gestationis begins as periumbilical, urticarial papules and plaques that develop into vesicles and bullae. The rash spreads over the entire body but spares the mucous membranes. Diagnosis is clinical but can be confirmed by skin biopsy.
The goal of treatment of pemphigoid gestationis during pregnancy is symptom control: relieving pruritus and limiting bullae formation. Pemphigoid gestationis typically responds to high-potency topical corticosteroids (eg, triamcinolone). Antihistamines (eg, loratadine, cetirizine) can also be added for pruritus relief. Disease that is unresponsive to topical corticosteroids may need systemic corticosteroids (eg, prednisone) or, rarely, immunosuppressants (eg, cyclosporine, azathioprine). Intractable disease may be an indication for early-term delivery. Obstetric complications include prematurity, fetal growth restriction, and neonatal pemphigoid gestationis. Symptoms typically resolve spontaneously after delivery, but women are at risk of recurrence with subsequent pregnancies.
Biophysical profile
A biophysical profile, an ultrasound examination of fetal movement, tone, breathing, and amniotic fluid volume, evaluates for fetal hypoxia after an abnormal nonstress test (eg, decelerations, no accelerations). Because this patient has a normal fetal heart rate tracing, a biophysical profile is not indicated.