NMS vs serotonin syndrome
- related: Neurology, pharmacology
- tags: #note
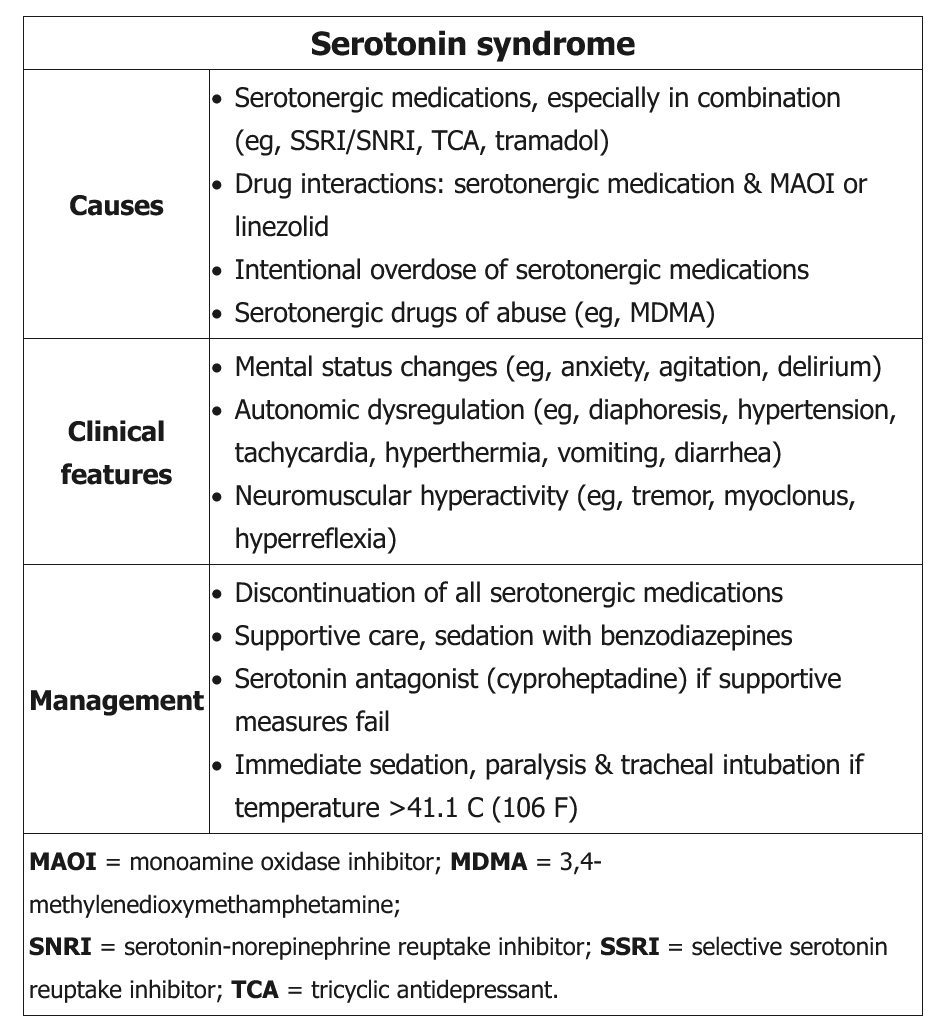 This patient's presentation is consistent with serotonin syndrome, which presents as a triad with varying degrees of:
This patient's presentation is consistent with serotonin syndrome, which presents as a triad with varying degrees of:
- Mental status changes
- Autonomic hyperactivity, and
- Neuromuscular abnormalities
Gastrointestinal symptoms and diaphoresis are also common. This syndrome can occur after initiation or dose increase of a serotonergic drug, administration of >2 drugs with serotonergic effects, or intentional overdose of a serotonergic drug. Common precipitating agents include MDMA, tramadol, selective serotonin reuptake inhibitors/serotonin-norepinephrine reuptake inhibitors, ergot derivatives, linezolid, and tricyclic antidepressants. This patient was given tramadol (a drug that impairs serotonin reuptake) while taking sertraline (a selective serotonin reuptake inhibitor).
Diagnosis is made clinically as there is no diagnostic test for this syndrome. Clonus is an important clinical finding. Treatment involves removing the offending drug, benzodiazepines for symptoms (eg, agitation), and supportive care. Critically ill patients require intubation in the intensive care unit. Cyproheptadine is the preferred antidote if supportive measures are unsuccessful.
Neuroleptic malignant syndrome is a life-threatening condition associated with the use of antipsychotics. It is characterized by delirium, very high fevers (often >40 C [104 F]), autonomic instability, and lead-pipe rigidity (rather than hyperreflexia and myoclonus).