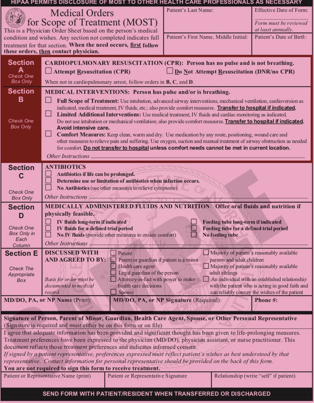
MOST form
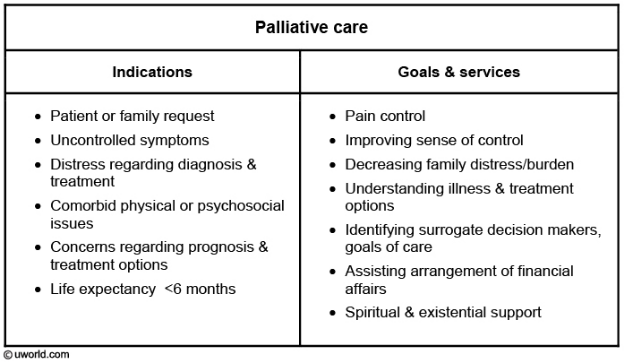
- related: goals of care, palliative care
- tags: #note
-
what is MOST form
- Orders by a Provider
- POLST Paradigm
- Most states have POLST, POST or MOLST
- In some states can be filled out by Advanced Care Providers and Physicians
- It is complete if only A or B is completed
-
Who is it form
- Seriously ill
- People who know what they want and are in the last stage of life…
- People you would not be surprised will die in the next year
-
Discuss:
- CPR (section A)
- Intubation and additional interventions (section B)
- Considered a complete for even if just A or B is completed
- Feeding tubes (section D)
- IV fluids and antibiotics are not necessary to cover and hard for most clinicians and patients to navigate
- I rarely talk about them in GOC discussions
Intubation
- Start with Intubation, not CPR
- Although the form starts with CPR, it can be helpful to discuss intubation first because CPR leads to intubation. If someone does not want intubation, then that person should probably not receive CPR. A picture of a patient who is intubated can be found on the internet, and can be helpful for explaining what it is.
- A Picture is worth a thousand words
- Consider using a stock photo of someone intubated

Intervention
- How do you feel about what you see in this picture?
- "What is your understanding of the ventilator in the ICU?""
- "It can be helpful for a short term problem such as pneumonia or surgery, but not as likely to help when you are terminally ill"
- "When you become sicker, how much are you willing to go through for the possibility of gaining more time?"
- "After CPR it is extremely likely you will be on the ventilator for at least a short period of time, such as a couple days"
- If patient not ok with intubation
- Ask why: understand their reasons
- Discuss risks and benefits
- Have a sense of their values and how they fit/don’t fit with request
- If not ok with intubation, should not have CPR
- If very sick and wants intubation:
- Keep patient’s values in mind
- Can recommend a time limited trial
- Ok to recommend to not be ventilated long term
- Ok to recommend not being intubated depending on their goals or your professional opinion
- If they want intubation and are seriously ill, take the discussion further:
- Keep their values in mind
- Make sense or not?
- Can recommend a time limited trial: a time limited trial is a defined period of time for an intervention to achieve a goal, such as improving enough to be extubated and if not able to be extubated, then discuss discontinuing intubation and focusing on palliative treatments to ensure comfort once extubated
- Ok to recommend to not be ventilated long term, which means receiving a tracheostomy and possibly living on a ventilator
- Ok to recommend not being intubated depending on their values, goals or your professional opinion (what is likely to achieve those goals)
CPR
•A Better Approach: What is your understanding of the outcomes of CPR?... Is it ok if I go over them with you?
•“We get a pulse back about 50% of the time, but we are bad at getting people back to who they were before CPR.” For every person who gets CPR in the hospital, at best only 17 out of 100 leave alive. Results in long hospital stays, often being considerably sicker, might lead to brain damage, Those who survive often need to go to the nursing home for more help”
If I had 100 people like you, however,
Instead of simply asking if someone wants CPR, a better approach is asking what is their understanding of CPR, particularly their understanding of the outcomes. Many know it means pumping on someone’s chest when they are unresponsive, but few know the statistics. These statistics have barely changed in the past 20 years.
•Debilitated patients: 10% •Stage IV Cancer patients survival 6 to 7% •Nursing home patients 5% •Dialysis: 5% •Medical ICU patients 2.2% •And again, those who survive are going to be sicker and spend much more time in the hospital and nursing home
Here are some more statistics to try to tailor a discussion for specific situations. Of course we do not know if someone will go into V-tach or asystole, but there is a striking difference in outcomes. Patients with cancer, patients in nursing homes and patients in the ICU have much worse outcomes.