MEN
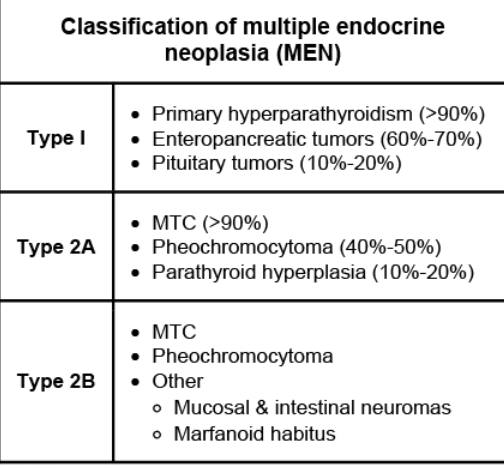
Multiple endocrine neoplasia type 2 (MEN 2) is an autosomal dominant disorder caused by germline mutations involving the RET proto-oncogene located on chromosome 10. MEN 2 can be divided into 3 classifications: MEN 2A, MEN 2B, and familial medullary thyroid cancer (FMTC). MEN 2A predisposes to medullary thyroid cancer (MTC), pheochromocytoma (PCC), and hyperparathyroidism (due to parathyroid hyperplasia or multiple adenomas). MEN 2B is not accompanied by hyperparathyroidism but may be associated with marfanoid habitus, mucosal neuromas, and skeletal deformations (eg, kyphoscoliosis, lordosis). FMTC is a subset of MEN 2A associated with MTC only, without PCC or parathyroid disease.
All patients with MTC require serum calcitonin and carcinoembryonic antigen, neck ultrasound (evaluation for regional metastases), genetic testing for germline RET mutations, and evaluation for coexisting tumors (hyperparathyroidism, PCCs). PCC is present in approximately 40% of patients with MEN 2, and undiagnosed PCC can cause life-threatening hemodynamic complications during and after thyroid surgery. Plasma-free metanephrines are usually elevated in PCC and confirmed with 24-hour urinary fractionated metanephrines, catecholamines, and abdominal imaging. Once PCC has been ruled out, patients with nonmetastatic MTC may proceed to thyroidectomy for definitive management.
Anticancer drugs and external beam radiation do not play a role in initial management of MTC. Radiotherapy is usually reserved for postsurgery patients with extrathyroidal disease or extensive nodal metastases not amenable to surgical resection. Chemotherapy is considered for patients with progressively metastatic MTC not responsive to surgery or radiotherapy.
Radioactive iodine is preferentially taken up by thyroid tissue and is often used following surgery for patients with differentiated thyroid cancer (papillary or follicular) who are at risk for recurrence. Radioactive iodine is not effective for MTC as these cells do not take up iodine.