Lyme
- related:ID, post lyme disease syndrome, neuroborreliosis, tick born infections
- tags: #note
Pathogenesis
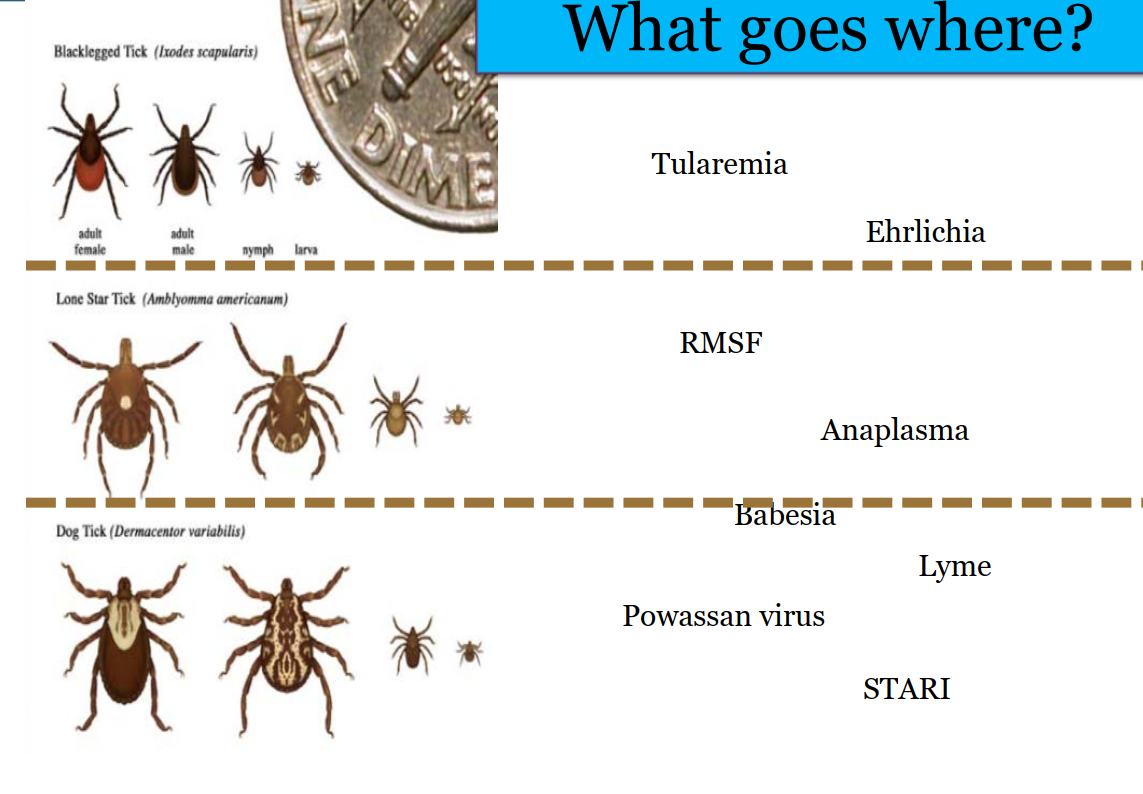
- bacteria: spirochete Borrelia burgdorferi
- tick: Ixodes scapularis "deer ticks"
- carrier: mice > deer
- time: most occur in summer
symptoms
- most patient won't recall tick bite
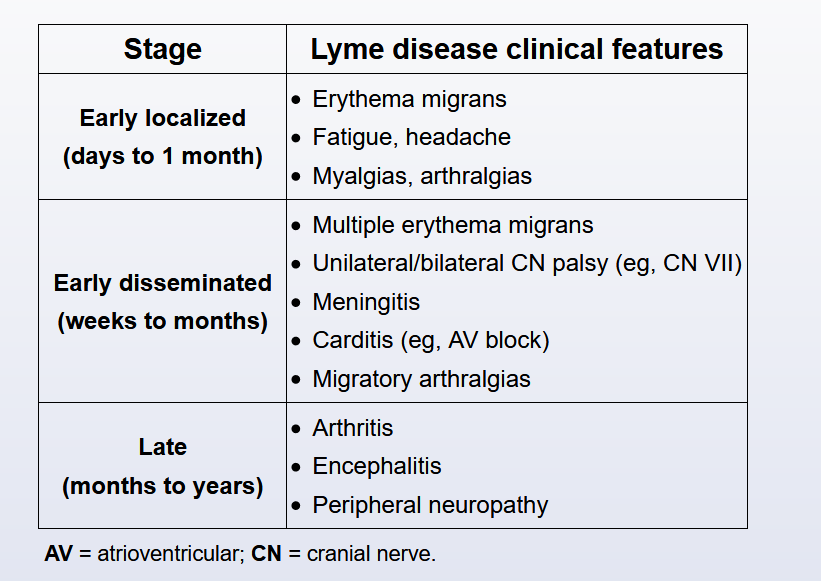
- early localized
- early disseminated
- late
- early and late are localized diseases. Early disseminated is widely distributed in multiple organs
Early localized
- fatigue, myalgia, headache
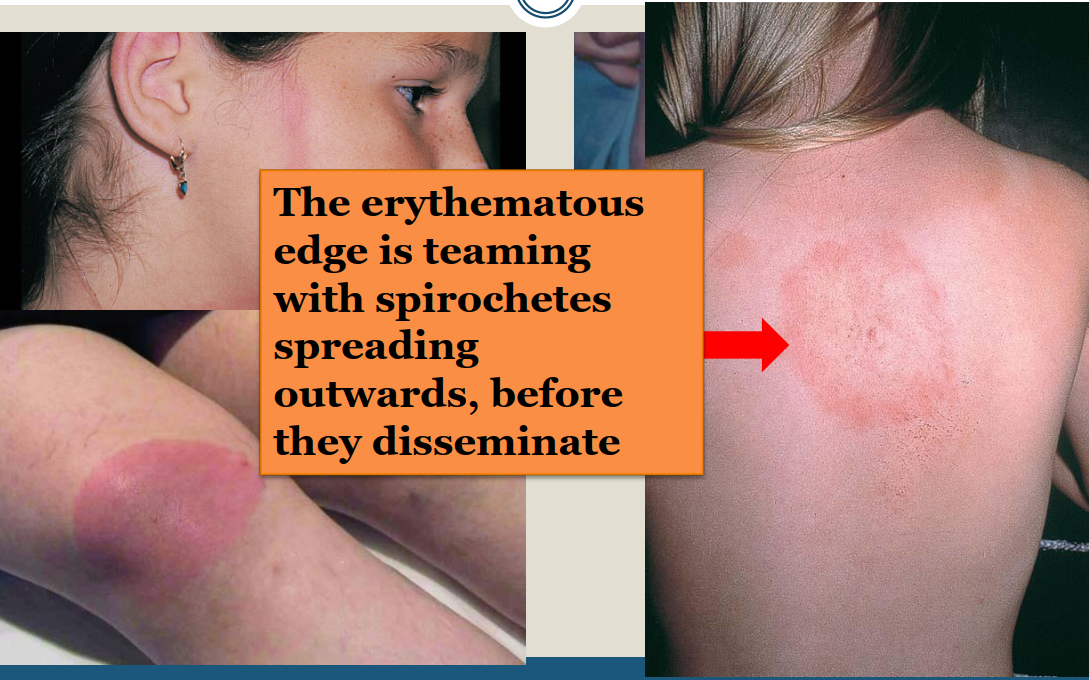
- bull's eye erythema migrans:
- 60-80%
- 1-2 weeks after bite
- 2-3 cm to 2 feet in diameter
- painful, itchy, or asymptomatic
- edge of the target: spirochetes spreading outwards before dissemination

early disseminated
- early disseminated rash
- neurologic finding: weeks to months
- lymphocytic meningitis: mostly with other sx, only 2% by itself.
- Dx with CSF WBC > 5, usually 150s
- positive serology
- elevated CSF lyme index or CSF:serum ab ratio
- CSF PCR insensitive: don't use
- radiculopathy
- CN palsy: usually 7, bilateral bell's palsy
- does not need to be late disease to have CNS sx
- lymphocytic meningitis: mostly with other sx, only 2% by itself.
- carditis: 1st to 3rd degree
- 1-28 weeks after infection
- pacemaker not indicated
- may need temporary pacer
- will improve with treatment

late
- months to years after infection
- arthritis: 1 joint, large joint, usually knee, 60% patients, usually effusion more than pain
- chronic neurologic: encephalitis, peripheral neuropathy
Approximately 60% of patients with untreated Lyme disease develop Lyme arthritis months or years later. A waxing/waning monoarticular arthritis in the knee is the most common manifestations but sometimes a few large joints are affected at once. In contrast to patients with forms of infectious arthritis, those with Lyme arthritis tend to be afebrile and well-appearing and can bear weight on the affected joint. However, arthrocentesis is generally performed because examination findings (eg, tenderness, swelling, decreased range of motion) can overlap with potentially destructive septic arthritis. In Lyme arthritis, the synovial fluid white blood cell (WBC) count is typically 20,000-60,000/mm³. The diagnosis is made by serum enzyme-linked immunosorbent assay and Western blot. B burgdorferi does not grow on standard bacterial joint culture (it requires specialized culture media that is not available in most clinical laboratories).
This patient's knee joint effusion, minimal pain, no fever, and recent tick bite raise strong suspicion for Lyme arthritis. Although most cases eventually resolve after years, patients are at risk for persistent or recurrent arthritis with joint damage. Therefore, treatment with a 28-day course of oral doxycycline or amoxicillin is recommended.
Diagnosis
Diagnosis is confirmed by clinical features and positive ELISA and western blot Lyme serologies.
- 2 tier EIA but very low PPV
- IgM and IgG bands remain positive for years
- IgM does not mean acute infection
- 5% population of NE US has positive baseline test
- Don't test unless there are symptoms
- early localized: clinical diagnosis. Serology neg. Repeat serology in a few weeks
- early disseminated: usually positive 80-90%
- late: negative serology excludes diagnosis
Treatment
- usually 10 days doxycycline
- alternative: amoxicillin, cefuroxime
Current guidelines recommend hospital admission with IV antibiotics (ceftriaxone preferred) to prevent long-term complications in symptomatic patients and those with second- or third-degree AV block or first-degree AV block with PR interval > 300 msec. Oral antibiotics (eg, doxycycline, amoxicillin, and cefuroxime) should be continued at discharge for a 21- to 28-day total course. Complete AV block requires temporary pacing as these blocks are self-limited and usually improve within 1 week. Lesser conduction disturbances may take up to 6 weeks for resolution.
In the past, doxycycline was not generally used to treat Lyme disease in patients age <8 due to the risk of tooth discoloration, but the American Academy of Pediatrics now recommends ≤21-day course of doxycycline as first-line treatment for late Lyme disease. Doxycycline is preferred due to better penetration into the CNS (eradicates organisms lodged there) and excellent efficacy against coinfecting, tick-transmitted pathogens (eg, Anaplasma phagocytophilum). Patients are also advised to rest and avoid high-impact activities until all symptoms resolve to reduce the risk of additional joint damage. More than 90% of patients are cured after oral antibiotic therapy.
Post lyme disease syndrome
- post lyme disease syndrome
- 10% will have ongoing sx
- headache
- fatigue, cognitive
- myalgia
- does not require prolonged abx course
This patient had a tick bite in Pennsylvania 3 months ago and now has left knee swelling and synovial fluid evidence of inflammation, raising strong suspicion for Lyme arthritis, the most common late complication of Lyme disease. Lyme disease is a spirochetal infection caused by Borrelia burgdorferi. It is transmitted by the deer tick Ixodes scapularis during blood feeding. Most cases occur in rural parts of the upper midwestern and northeastern United States, where the tick is endemic. Initial transmission is often (~80%) marked by a spreading, annular rash (erythema migrans) and systemic symptoms; however, asymptomatic or unrecognized cases often go untreated, leading to persistent infection.