Lupus
Systemic lupus erythematosus (SLE) is a significant risk factor for the development of premature coronary atherosclerosis and coronary artery disease (CAD). SLE is associated with accelerated atherosclerosis due to a combination of traditional (eg, hypertension, hyperlipidemia) and disease-related risk factors (eg, chronic inflammation, glucocorticoid use). Compared to other women age 35-44, patients with SLE have an almost 50-fold increase in CAD risk. CAD is a significant contributor to premature death in SLE patients. For this reason, the most likely cause of this patient's death is myocardial infarction (with secondary ventricular arrhythmias) due to premature CAD.
Pericarditis is a common cardiac complication of SLE. These patients typically exhibit positional substernal chest pain with friction rub on auscultation. It is usually associated with other symptoms of serositis (eg, dyspnea due to pleural effusion). However, large pericardial effusions and/or tamponade are rare in patients with SLE.
This patient's high-titer ANA and mild cytopenia further support a diagnosis of systemic lupus erythematosus (SLE). Anti-dsDNA antibodies are helpful to confirm a diagnosis of SLE, but are also useful to follow the course of disease. In some patients, titers of anti-dsDNA antibodies correlate with disease activity. Anti-dsDNA antibody levels have also been associated with the development of lupus nephritis—immune complexes containing these antibodies are actually seen within the glomeruli of patients with lupus nephritis. Rising titer levels of anti-dsDNA antibodies can be helpful in confirming that the underlying lupus is the cause of a clinical problem as opposed to infection, medication toxicity, or unrelated disease.
This patient's presentation – fatigue, night sweats, arthralgia/arthritis, and pleuritis/pleural effusion – is suggestive of drug-induced lupus due to hydralazine. It is seen in approximately 5%–10% of patients receiving hydralazine and occurs due to development of autoantibodies that trigger an autoimmune response and a clinical syndrome similar to systemic lupus erythematosus. Other autoantibodies, with the exception of anti-histone antibodies, are uncommon in this disorder.
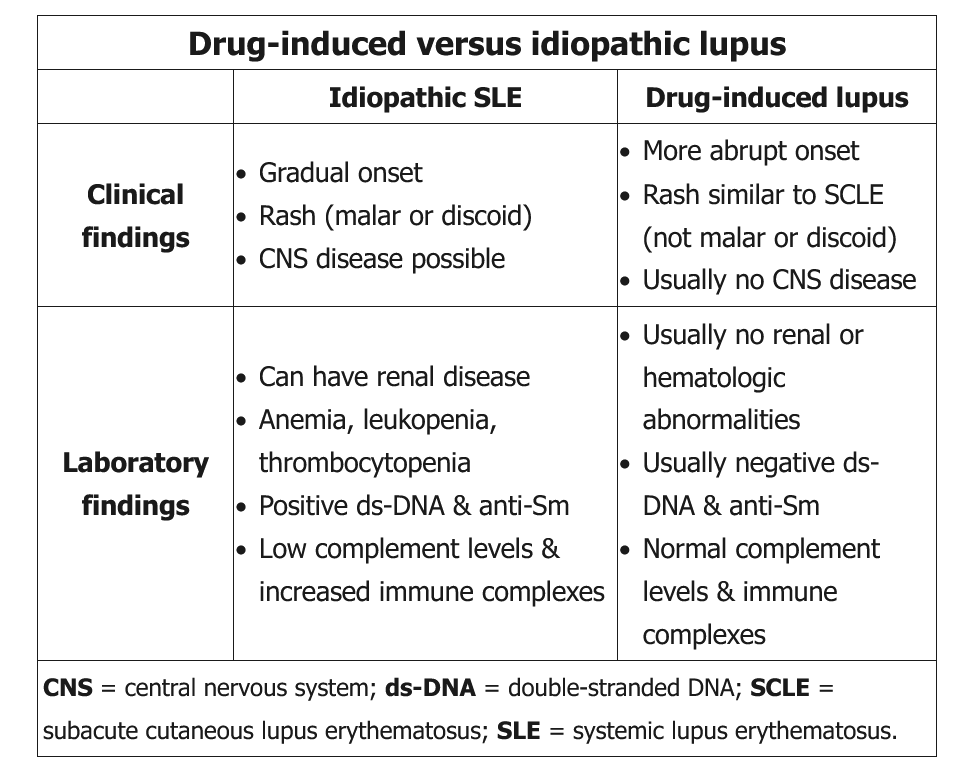
Common symptoms in drug-induced lupus include fever, malaise, myalgias, and arthralgias. Pleuritis is common in procainamide-induced lupus but uncommon with minocycline. Most patients do not develop the typical SLE malar rash, although drug-induced lupus may cause scaly, papulosquamous plaques (typically in a photodistributed pattern but often sparing the face) reminiscent of subacute cutaneous lupus. End-organ (eg, kidney, central nervous system) manifestations are significantly less common in drug-induced lupus than in SLE.
Most patients with drug-induced lupus (95%-100%) have a positive antinuclear antibody assay, particularly histone autoantibodies, but anti–double-stranded DNA and anti-Smith antibodies are rare. Also, drug-induced lupus is less likely to cause cytopenias and complement depletion. Discontinuation of the inciting drug usually leads to gradual resolution of symptoms. Nonsteroidal anti-inflammatory drugs and topical and systemic glucocorticoids can be used to alleviate symptoms if needed.
Drug-induced lupus causes multisystem involvement, and clinical findings can include fever, malaise, myalgia, arthralgia/arthritis, serositis (pleuritis, pericarditis), and/or hepatomegaly/splenomegaly. The diagnosis is made by a history of one or more offending drugs and a positive test for antinuclear antibodies (ANAs). Some common drugs associated with risk of lupus include procainamide, hydralazine, minocycline, INH, and anti-tumor necrosis factor (TNF) alpha therapy (etanercept, infliximab). Treatment is generally symptomatic, and discontinuation of the offending drug typically leads to resolution of symptoms within weeks to months.