Hemochromatosis
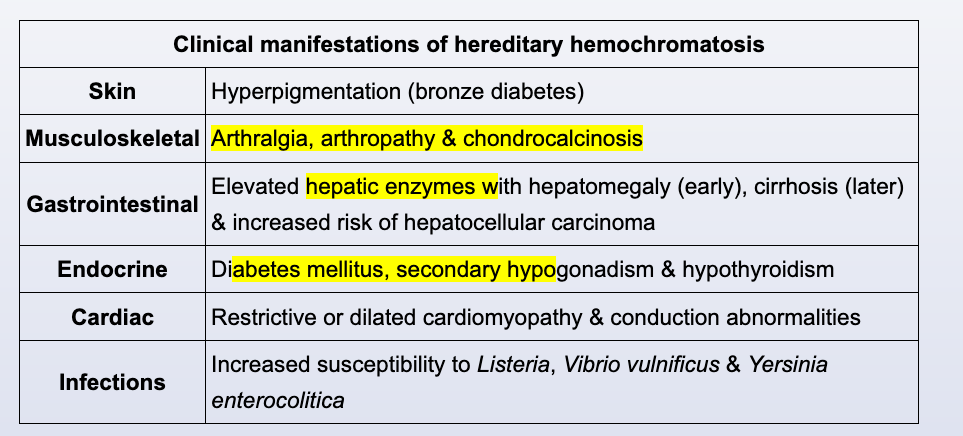
This patient with a family history of cirrhosis has fatigue, poor libido (possibly due to secondary hypogonadism), mild elevations in hepatic transaminases, and an elevated ferritin and transferrin saturation. This presentation is concerning for possible hereditary hemochromatosis (HH). HH is an autosomal recessive disorder characterized by iron deposition in a variety of tissues, leading to multisystem organ damage. Clinical manifestations usually start to appear in the 4th to 6th decade, with women presenting later due to menstrual iron loss.
The initial evaluation of HH includes serum iron studies, which show increased levels of serum iron, ferritin, and transferrin saturation. The diagnosis can be confirmed with genetic testing for hemochromatosis-associated mutations (eg, HFE). Liver biopsy is not required but may be useful to stage the extent of liver involvement (eg, in patients with significant liver function test abnormalities) or to confirm the diagnosis in patients who have evidence of iron overload but negative results on the standard HFE gene markers. Long-term management of hemochromatosis involves serial phlebotomy to deplete excess iron stores.
Autoimmune hepatitis is associated with elevated titers of antinuclear and anti-smooth muscle antibodies. This disorder can also cause extrahepatic manifestations (eg, arthritis, pericarditis), but it is usually associated with more dramatic elevations in transaminases and is much more common in women.
This patient with cardiac conduction abnormalities and secondary hypogonadism likely has hereditary hemochromatosis (HH). The classic presentation of cirrhosis, diabetes, and skin hyperpigmentation (eg, bronze diabetes) occurs in <25% of HH cases and is typically a late manifestation of the disease.
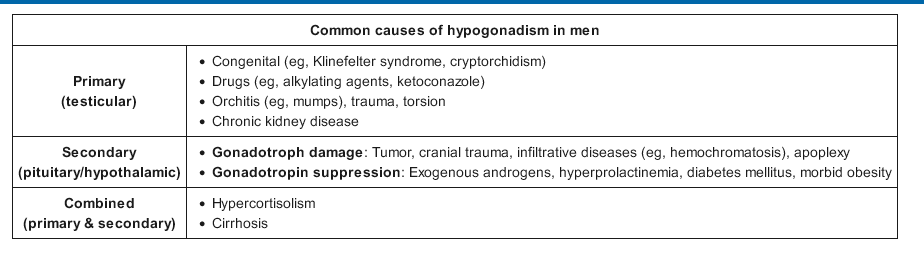
Nonspecific symptoms may occur years before diagnosis and commonly include extreme fatigue, arthralgia, and loss of libido. Cardiac conduction abnormalities occur in about 31% of cases and can manifest as sick sinus syndrome, as seen in this patient. Approximately 45% of patients also develop secondary hypogonadism due to iron accumulation in the pituitary gonadotrophs. Laboratory tests may consequently show low levels of serum testosterone, LH, and FSH. Patients who undergo phlebotomy before age 40 have a higher likelihood of regaining normal gonadal function.
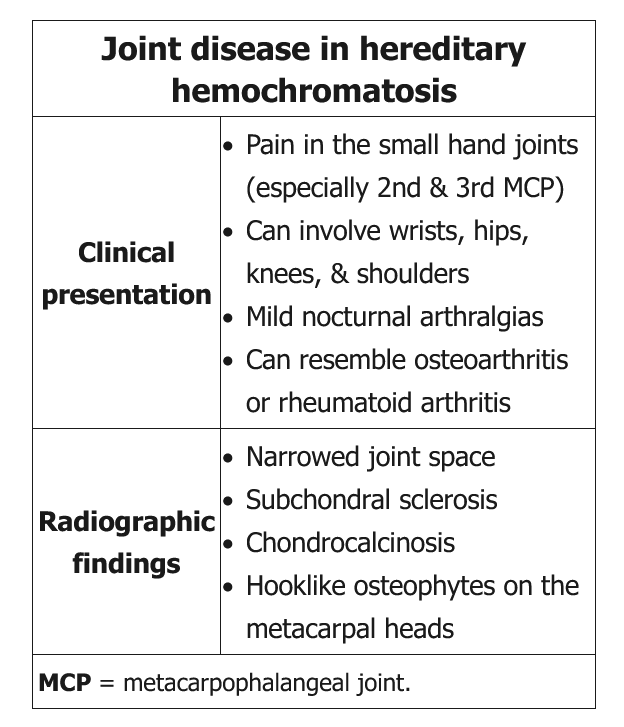
This patient has an acute inflammatory arthritis associated with chondrocalcinosis. Although microscopy results from the synovial fluid are not yet available, they are likely to show rhomboid-shaped calcium pyrophosphate dihydrate crystals consistent with pseudogout.
Pseudogout is most common in the elderly. Occurrence in a young or middle-aged man suggests possible secondary causes, such as hemochromatosis. Hemochromatosis causes reduced clearance of calcium pyrophosphate crystals from the synovial fluid. Therefore, patients can develop any aspect of calcium pyrophosphate deposition disease, ranging from the chondrocalcinosis and the classic polyarthropathy (hook-like osteophytes most prominent in the 2nd and 3rd metacarpophalangeal joints) to acute pseudogout. Given this patient's relatively young age, he should be screened for hemochromatosis with serum iron studies (ie, serum iron, total iron-binding capacity, ferritin).