HPV and pregnancy
Human papillomavirus (HPV) is a common sexually transmitted virus that causes cervical cancer. In immunocompetent women, HPV usually causes a transient infection. Immunosuppressed patients (eg, HIV infection) are unable to clear HPV and are at increased risk for persistent HPV infection that can progress to cervical dysplasia and cancer. Therefore, patients newly diagnosed with HIV are recommended to have a Pap test immediately after diagnosis followed by close interval screening. In patients with HIV, invasive cervical cancer is an AIDS-defining illness.
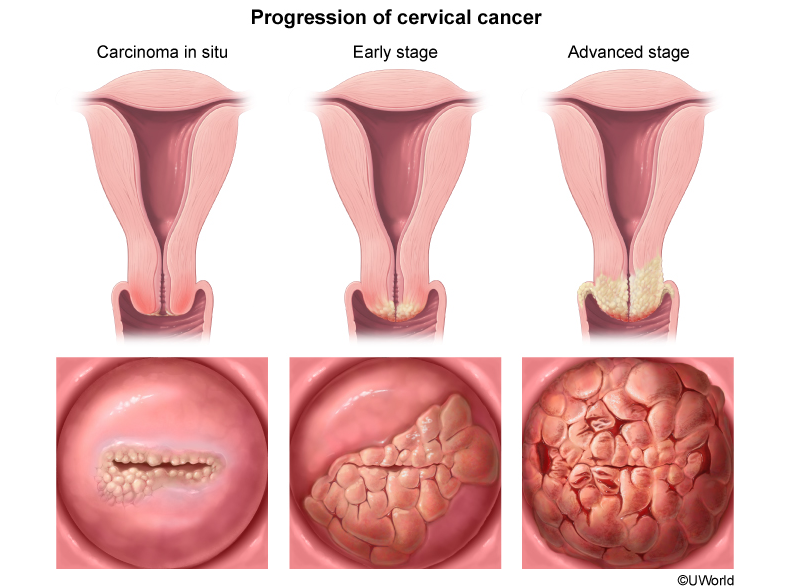
Most patients diagnosed with cervical dysplasia are asymptomatic. Invasive cervical cancer typically presents in patients who have not had routine Pap test screening and can be asymptomatic. However, the most common presenting features of invasive cervical cancer are irregular vaginal bleeding and a friable, exophytic cervical mass. Other features of cervical cancer include postcoital bleeding; watery, mucoid vaginal discharge; and ulcerative cervical lesions. Suspicious cervical lesions require a cervical biopsy to evaluate for cancer. Additional risk factors for cervical cancer include tobacco use, prior sexually transmitted infection, and multiple sexual partners.
HPV can be vertically transmitted. Children with vertically transmitted HPV typically present with lesions in the oropharynx, larynx, or trachea at age 2-5; the most severe manifestation is juvenile-onset respiratory papillomatosis (JRP). There is an association between JRP, childhood HPV disease, and maternal HPV disease. However, cesarean delivery does not prevent vertical transmission or decrease the risk for JRP or childhood HPV disease. Therefore, expectant management for vaginal delivery is the best management for this patient.
A 39-year-old woman, gravida 3 para 2, at 7 weeks gestation comes to the emergency department for vaginal bleeding that began 3 hours ago and has soaked through a pad. Since her arrival, the bleeding has subsided. She reports no abdominal pain or cramping. Her first prenatal visit is in 1 week. The patient has a history of HIV, contracted 3 years ago through unprotected sexual intercourse, but she has declined treatment as she has fel"healthy." She has no previous surgeries. The patient's 2 prior pregnancies ended in uncomplicated term vaginal deliveries; the last delivery was 4 years ago. Her last Pap test, 4 years ago, was normal. She has smoked half a pack of cigarettes a day for 13 years but does not drink alcohol or use illicit drugs. Blood pressure is 130/80 mm Hg and pulse is 82/min. BMI is 24 kg/m2. Abdominal examination shows no tenderness or masses. The external genitalia have no lesions. Speculum examination reveals minimal bright red blood in the vaginal vault. The cervix is closed and there is a 3-cm, firm, white, irregular mass on the anterior cervix that bleeds when touched with a cotton applicator. Laboratory results are as follows:
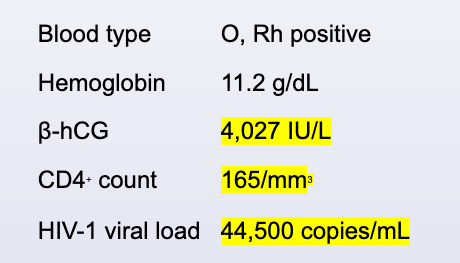
A bedside transvaginal ultrasound reveals an intrauterine gestation with normal fetal cardiac activity. Which of the following is the best next step in management of this patient?