HFpEF
- related: Cardiology
- tags: #note
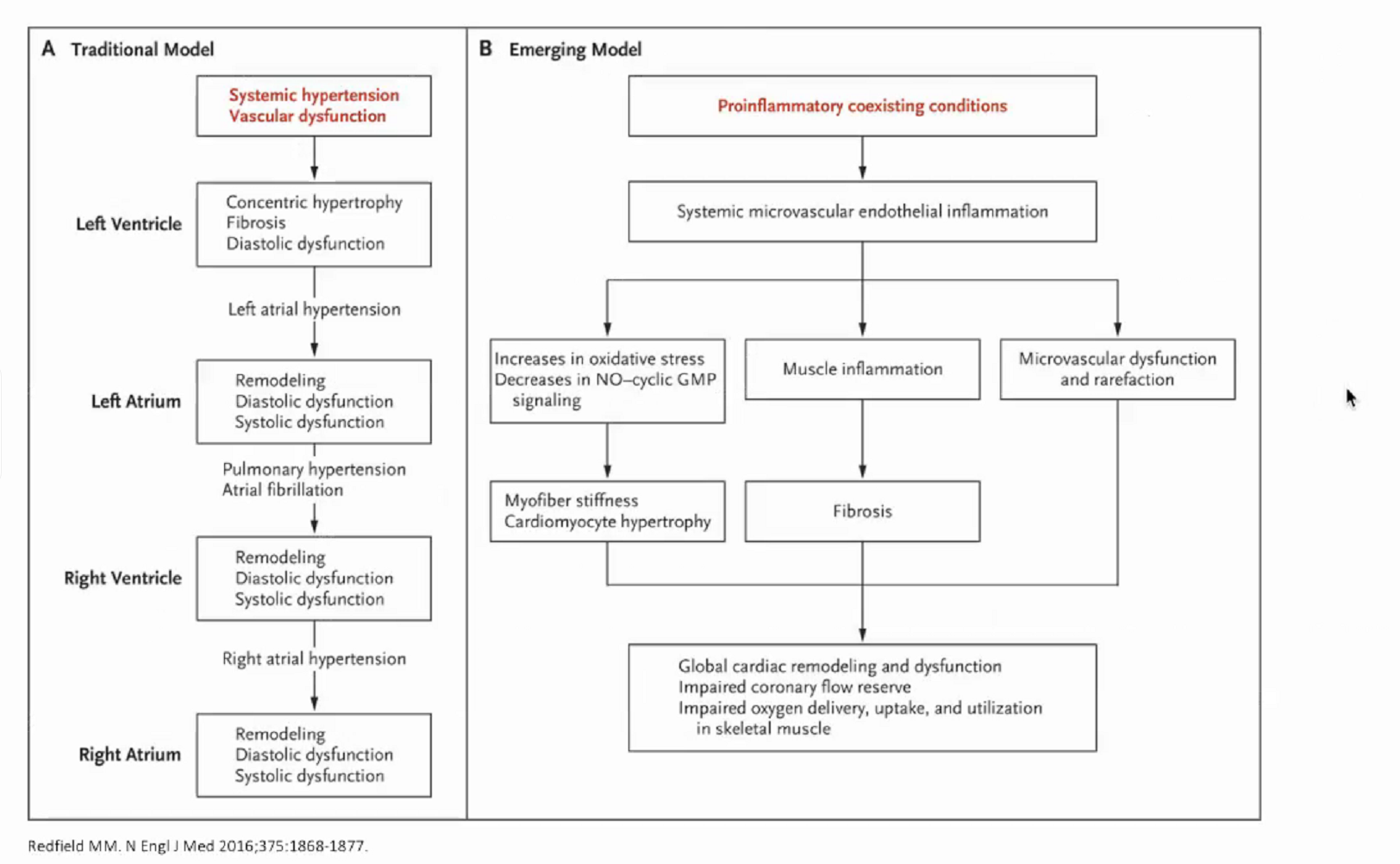
Pathophysiology
normal
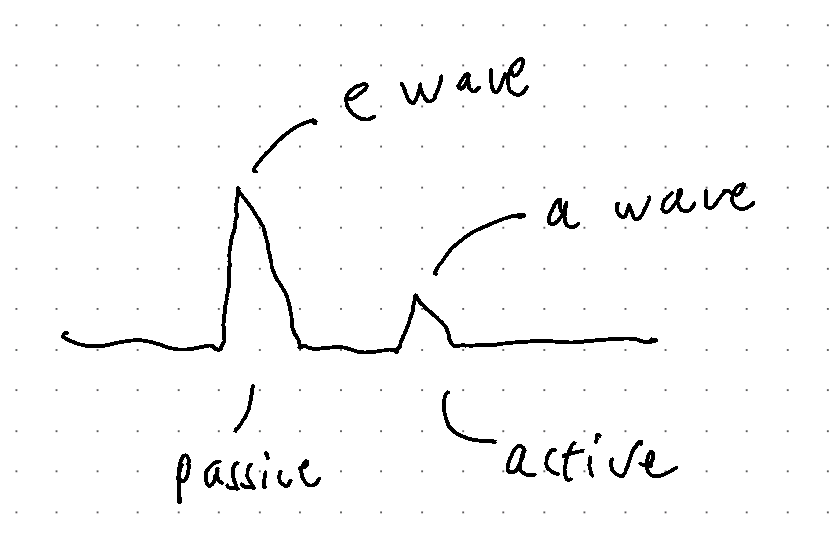
- Passive: LV relaxation
- Active: Atrial kick
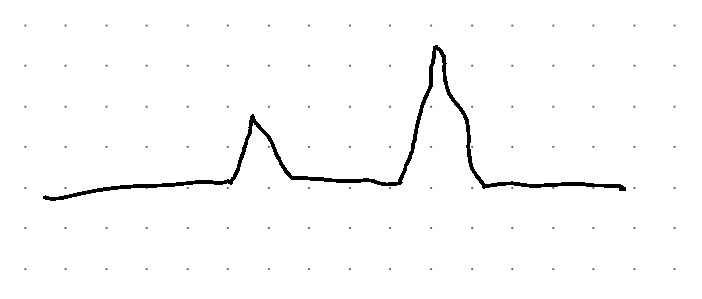
- As we age, LV stiffens up
- Passive filling goes down
- we rely more on atrial kick
- LA pressure is normal however
Pseudonormal LV filling
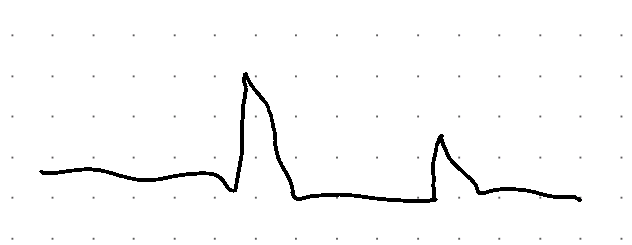
- Mild HFpEF
- LAP very high: high gradient
- atrial kick not as high
- More passive filling due to high gradient
Resistant LV filling
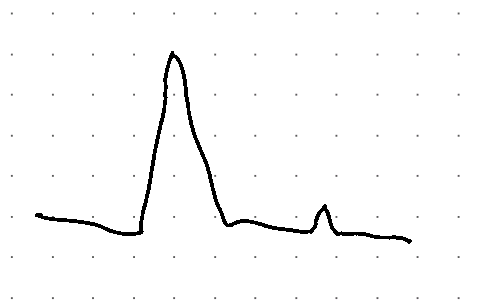
- LAP very very high
- LV can't accommodate
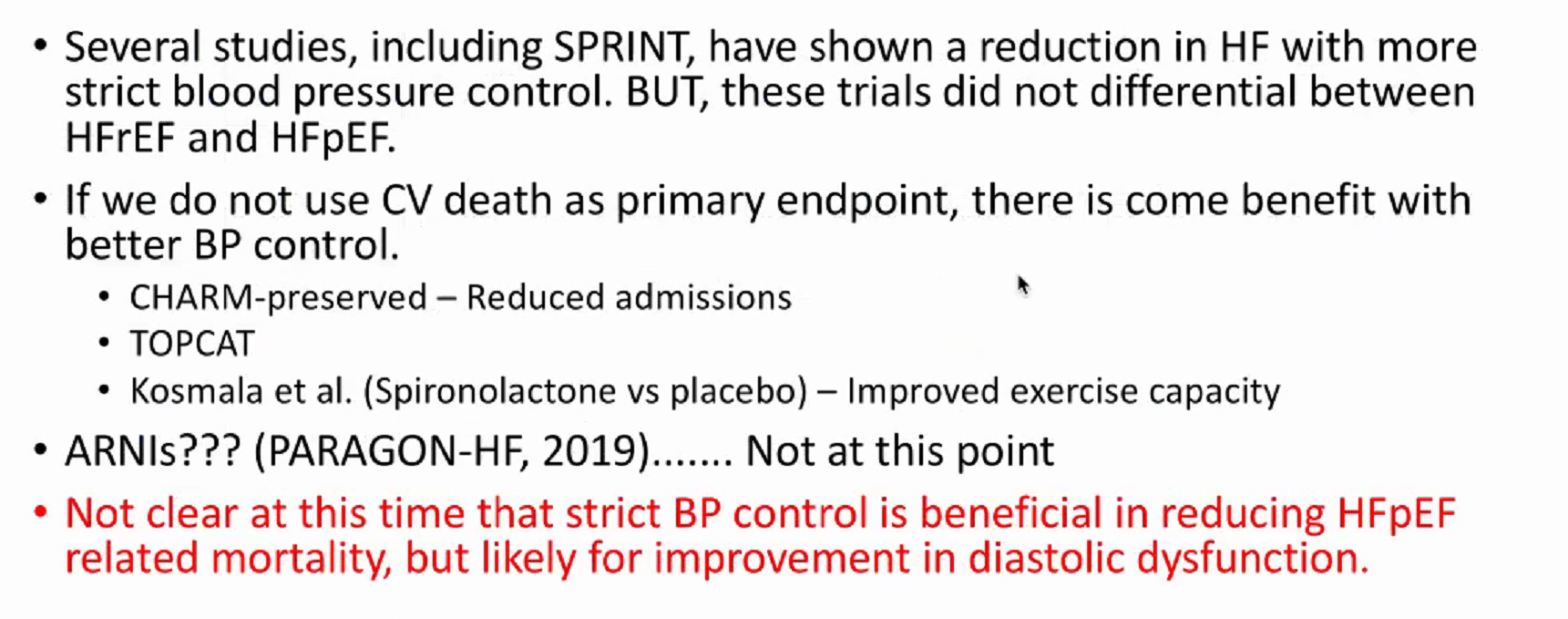
- strict BP maybe not help
Uworld
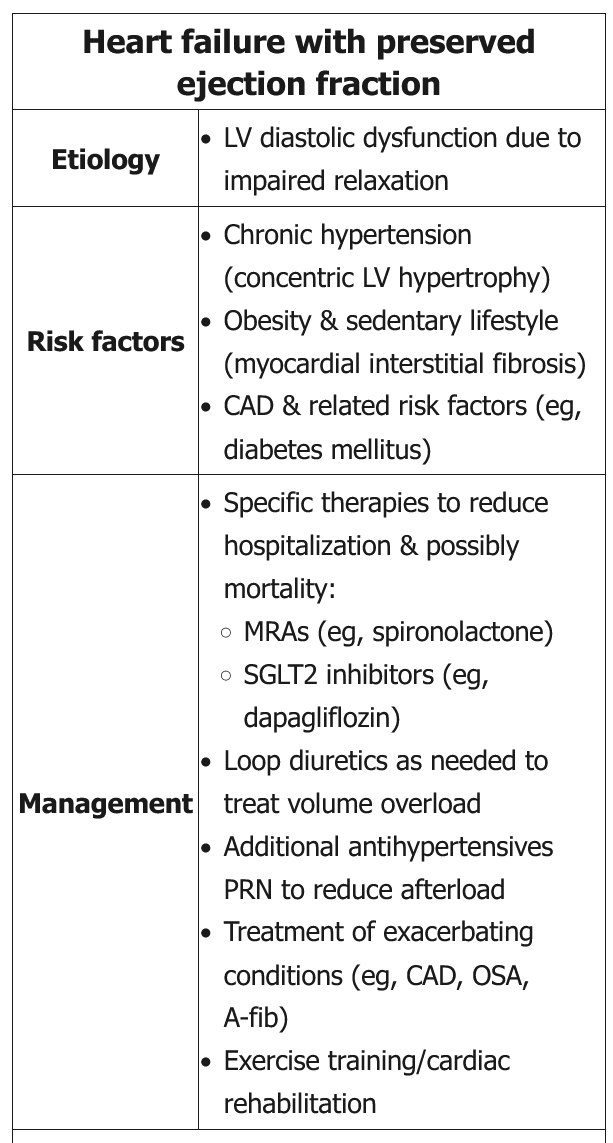
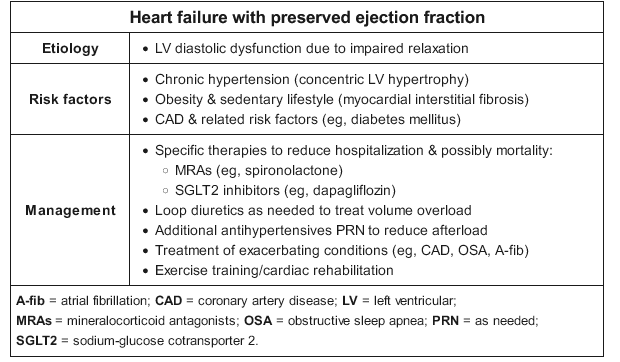 This patient has heart failure with preserved ejection fraction (HFpEF), with signs and symptoms of volume overload, normal left ventricular ejection fraction (LVEF) (>50%), and left ventricular hypertrophy.
This patient has heart failure with preserved ejection fraction (HFpEF), with signs and symptoms of volume overload, normal left ventricular ejection fraction (LVEF) (>50%), and left ventricular hypertrophy.
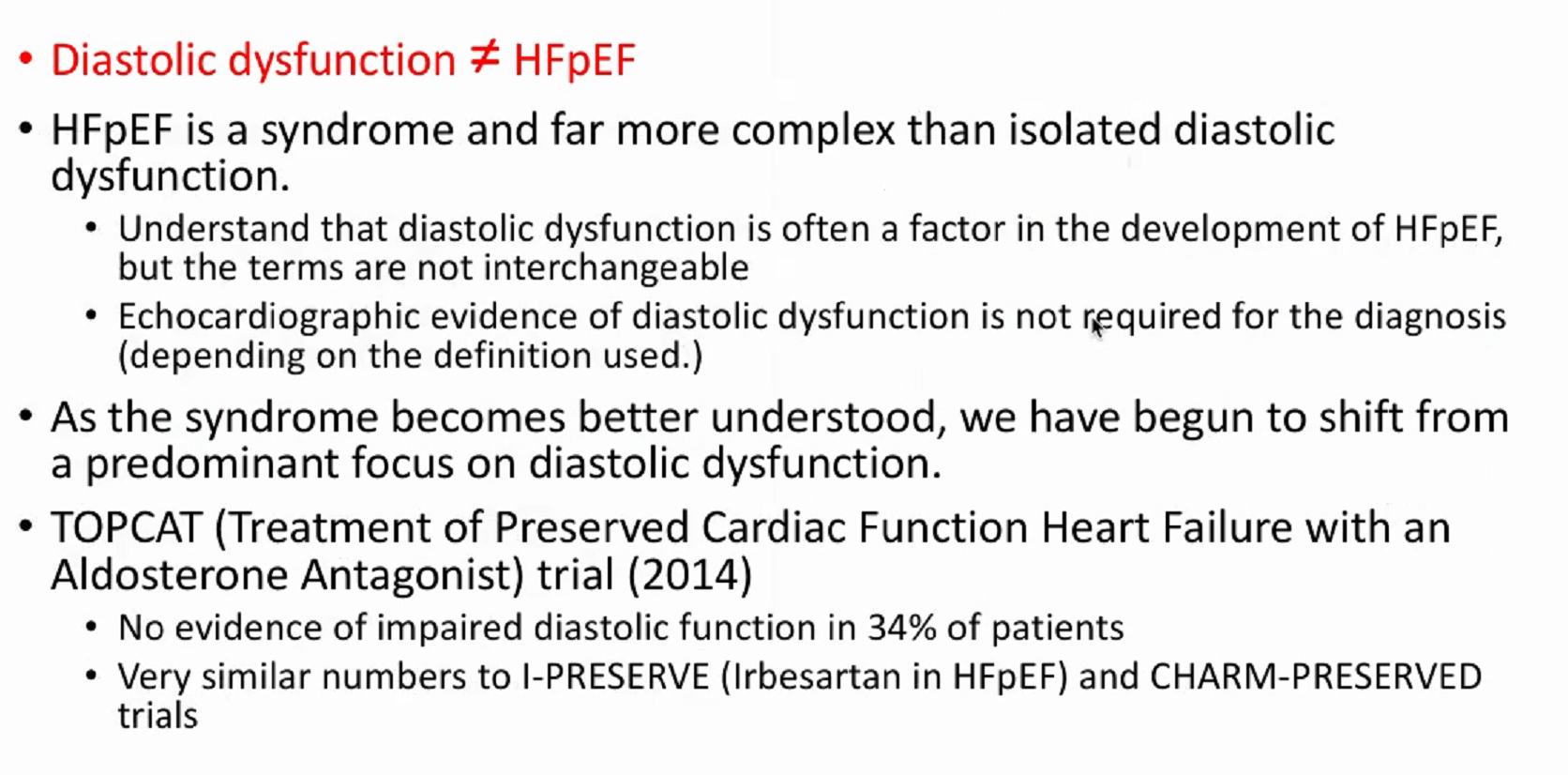
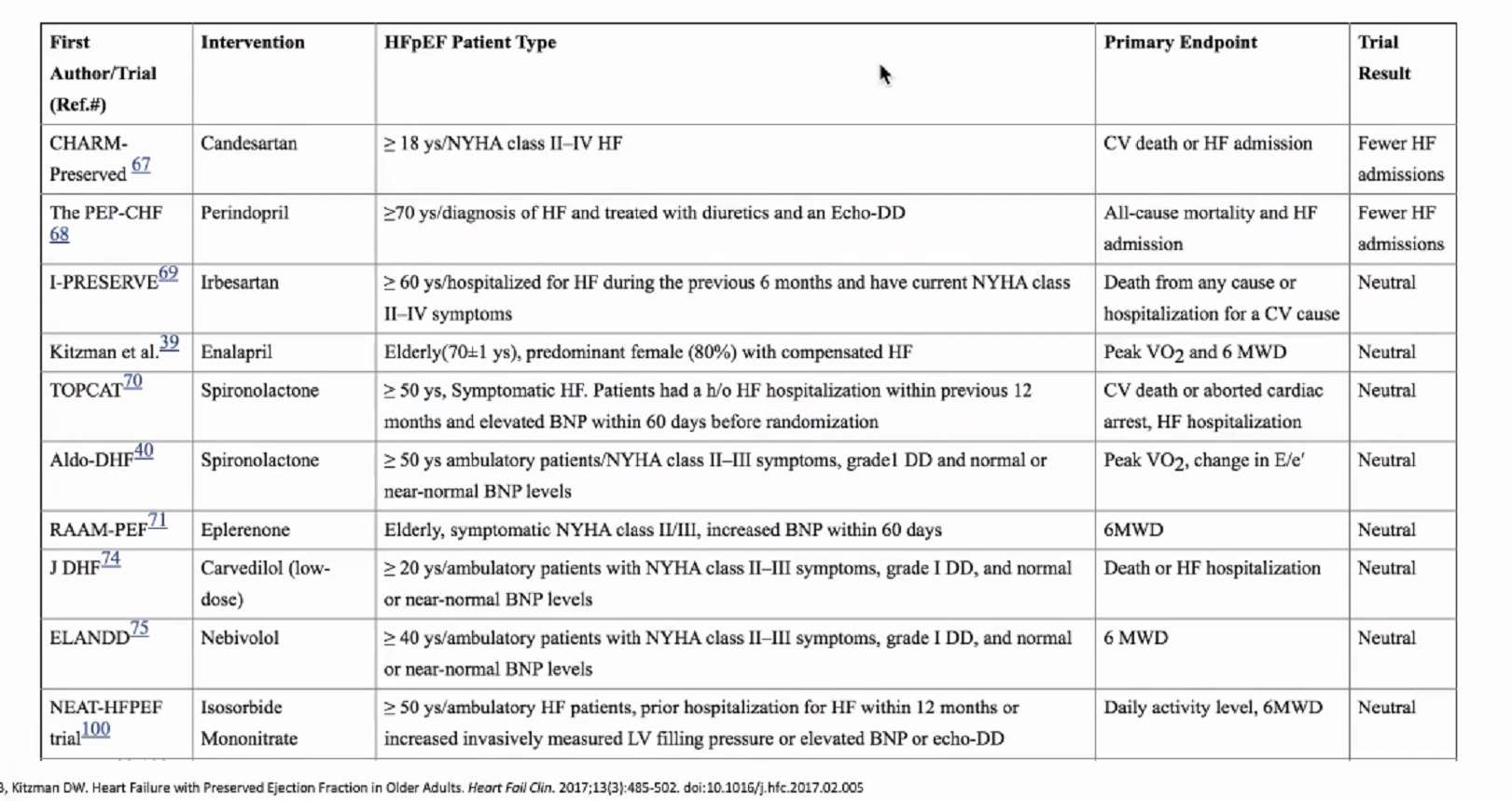
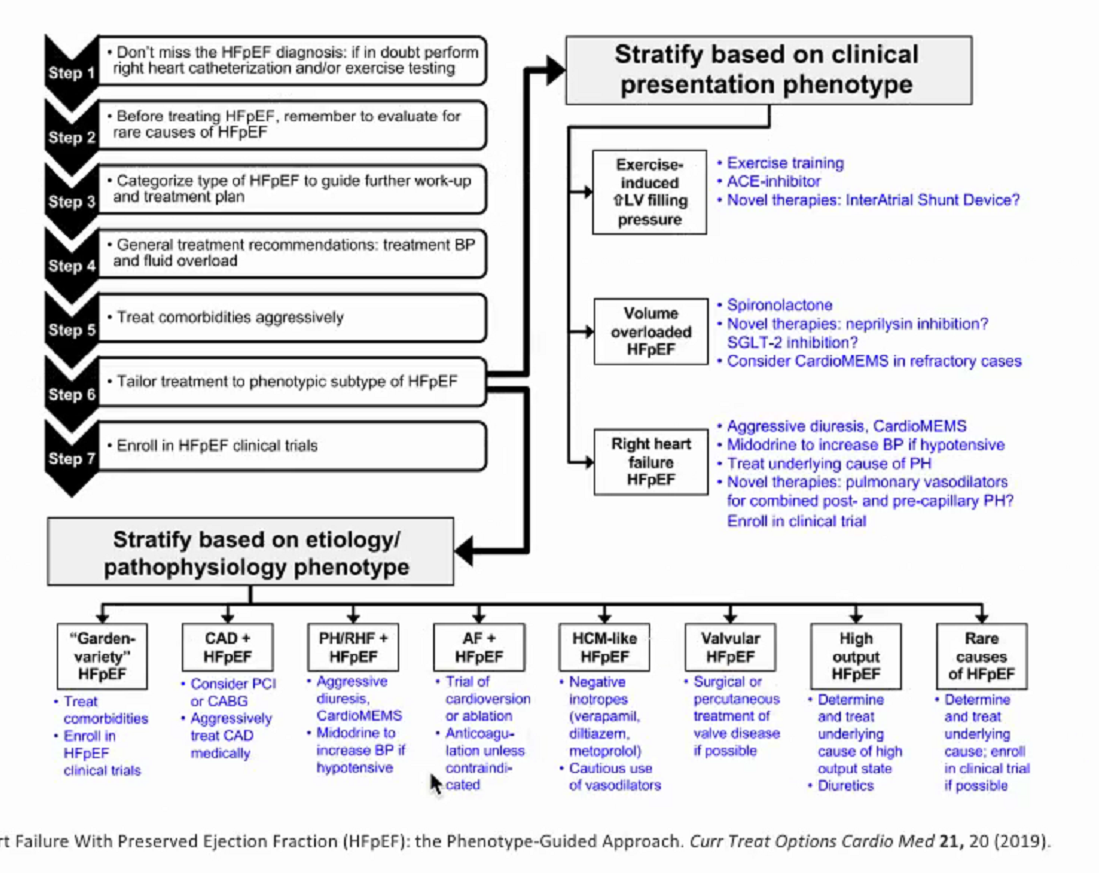
In comparison with heart failure with reduced ejection fraction (HFrEF), HFpEF has overall demonstrated less response to neurohormonal antagonists (eg, angiotensin system blockers, beta blockers); however, aldosterone antagonists (eg, spironolactone) have been shown to reduce hospitalizations and possibly improve survival. Optimal management of HFpEF involves the following:
- Afterload reduction (ie, blood pressure <130/80 mm Hg). Aldosterone antagonists are first-line therapy.
- Treatment of volume overload with diuretics
- Treatment of exacerbating conditions (eg, rate control of atrial fibrillation, coronary revascularization)
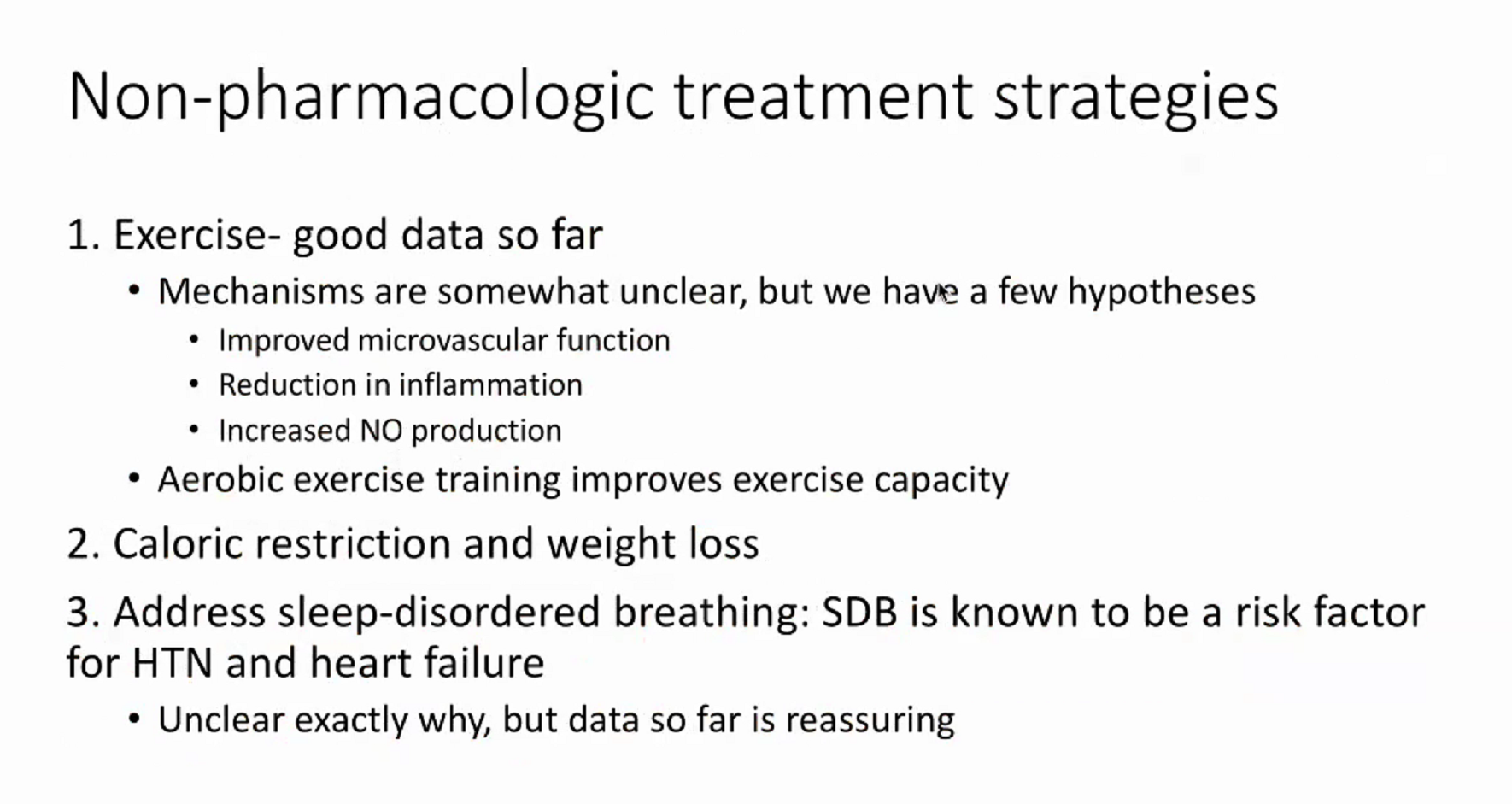
In addition, exercise training in a cardiac rehabilitation program has been shown to improve functional capacity and overall quality of life in patients with HFpEF.
Medications
Several studies show a clear benefit of aldosterone receptor antagonists (eg, spironolactone) and sodium-glucose cotransporter 2 (SGLT2) inhibitors (eg, dapagliflozin) for HFpEF. These agents lower systemic afterload, improve diastolic function, attenuate cardiac hypertrophy, and help achieve euvolemia through their diuretic effects.
Beta blockers improve survival in patients with HFrEF, but they have not shown similar benefit in patients with HFpEF. In the management of HFpEF they are useful for reducing the ischemic burden of coronary artery disease and for rate control of atrial fibrillation, but in the absence of these indications they provide minimal clinical benefit.
This patient's blood pressure is currently under control and long-acting nitrates have not shown any particular benefit in patients with HFpEF. In fact, these drugs are associated with decreased activity levels and occasional hypotension in such patients and should be avoided. Suitable options for blood pressure control in patients with HFpEF include aldosterone antagonists, angiotensin system blockers, dihydropyridine calcium channel blockers, and beta blockers (eg, carvedilol).
Phosphodiesterase-5 inhibitors (eg, sildenafil) are indicated for pulmonary arterial hypertension (ie, group 1 pulmonary hypertension), but they have demonstrated no benefit for pulmonary hypertension resulting from left-sided heart disease (ie, group 2 pulmonary hypertension).