HCC hepatocellular carcinoma
- related: GI, Disorders of the Liver
- tags: #GI
Hepatocellular carcinoma is the most common liver tumor arising in patients with cirrhosis, the fifth most common cause of cancer worldwide, and the second most common cause of cancer-related deaths worldwide. Approximately 85% of patients with hepatocellular carcinoma have cirrhosis.
Patients with cirrhosis, regardless of the cause, require surveillance liver ultrasound with or without α-fetoprotein measurement every 6 months, which leads to early diagnosis, increased rate of curative treatment, and improved 3-year survival rates. Patients with HBV infection can develop hepatocellular carcinoma even in the absence of cirrhosis; therefore, surveillance for hepatocellular carcinoma is recommended even in the absence of cirrhosis in individuals at high risk (individuals with HBV who are from sub-Saharan Africa and older than age 20 years, Asian men older than age 40 years, and Asian women older than age 50 years).
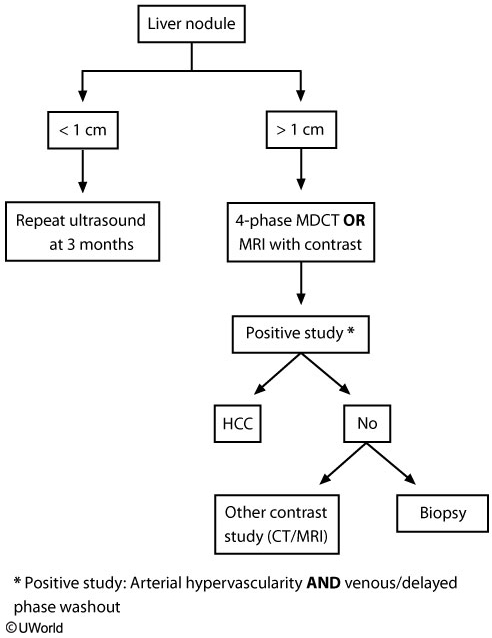
This patient with known cirrhosis has abdominal pain, elevated alpha-fetoprotein (AFP), and a 2-cm mass found on ultrasound. He needs an MRI of the liver as it has better sensitivity and specificity than CT scan or ultrasound in differentiating malignant nodules from the regenerative nodules associated with cirrhosis.
Most cases (80%) of hepatocellular carcinoma (HCC) are due to underlying chronic hepatitis B and C virus infection. Routine surveillance for HCC in high-risk patients (eg, those with chronic hepatitis B infection and/or cirrhosis) is done with abdominal ultrasound every 6 months. AFP is not routinely checked due to high false-positive rates. Early detection of HCC (tumors < 2 cm) offers the advantage of several treatment options for these patients.
Surgical resection of the lesion requires anatomic delineation, which is best achieved with multiphase CT or MRI scanning. Chest CT and bone scan are also frequently used to determine tumor spread. Once imaging studies are available, a decision regarding surgery can be made depending on patient and tumor characteristics.
Bleeding and tumor seeding (via needle track) are risks associated with percutaneous biopsy. Therefore, it is recommended only when initial imaging studies do not provide a clear diagnosis.
The diagnosis of hepatocellular carcinoma can usually be made without biopsy using multiphase contrast-enhanced CT or MRI in patients with cirrhosis and a lesion at least 1 cm in size that enhance in the arterial phase and have washout of contrast in the venous phase.. Biopsy may be needed for lesions that are large, growing, or indeterminant on imaging.
Many specialty societies have issued guidelines for the management of hepatocellular carcinoma. Patients with CTP class A cirrhosis, without significant portal hypertension or jaundice, and a singular lesion 5 cm in size or smaller should be considered for resection. Liver transplantation should be considered in patients with hepatocellular carcinoma within the Milan criteria and with portal hypertension or jaundice. The Milan criteria are as follows: up to three liver lesions 3 cm in size or smaller or one lesion 5 cm in size or smaller, without macrovascular invasion, and without extrahepatic spread. Patients who are not surgical or liver transplantation candidates should be considered for locoregional therapy in the absence of macrovascular invasion (tumor thrombus) or extrahepatic spread. Locoregional therapies include radiofrequency ablation, microwave ablation, transarterial chemoembolization, and transarterial radioembolization. Decisions about locoregional therapy are increasingly made through multidisciplinary tumor boards. Sorafenib is used for advanced hepatocellular carcinoma, which includes cases with macrovascular invasion or extrahepatic spread. In 2017, the FDA approved two drugs for second-line therapy: regorafenib, an oral multi-kinase inhibitor, and nivolumab, an intravenous humanized monoclonal antibody against the programmed cell death receptor.