Group B strep
Intrapartum antibiotic prophylaxis can prevent transmission of group B Streptococcus (GBS) to the infant and minimize the risk for early-onset sepsis. Indications for prophylaxis include maternal GBS bacteriuria, a positive rectovaginal culture for GBS (obtained at 35-37 weeks gestation), or a previous infant with invasive GBS disease. A positive rectovaginal culture for GBS during a previous pregnancy is not an indication for prophylaxis in subsequent pregnancies.
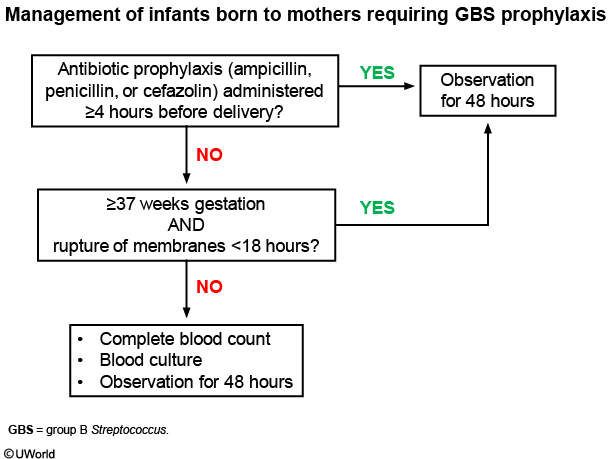
Prophylaxis is considered adequate if ampicillin, penicillin, or cefazolin is administered >4 hours before delivery. Vancomycin, clindamycin, or other antibiotics are not considered adequate prophylaxis due to increasing bacterial resistance and slower distribution across the placenta and into amniotic fluid. Although this mother received ampicillin, the prophylaxis is inadequate as it was given only 90 minutes before delivery.
All infants born to GBS-positive mothers, regardless of prophylaxis, should be observed in the nursery for 48 hours to monitor for signs of infection (eg, lethargy, poor feeding, temperature instability). In infants whose mothers were not treated adequately, a complete blood count and blood culture should be obtained only if the infant is preterm (<37 weeks gestation) or if there was prolonged rupture of membranes (>18 hours). This well-appearing infant is full term and rupture of membranes occurred only 3 hours before delivery; therefore, no workup is indicated.
In addition to a complete blood count and blood culture, antibiotics are indicated if the infant is ill-appearing or born to a mother with chorioamnionitis. Ill-appearing infants should also undergo lumbar puncture for evaluation of meningitis. This infant is well-appearing, and the mother did not have chorioamnionitis.
Strep vs B19
Parvovirus B19 is a common viral infection that typically presents with nonspecific flu-like symptoms (eg, fever, myalgias), followed by variable symptoms, depending on the age of the patient. Young children classically develop a "slapped cheek" malar rash (erythema infectiosum) and, rarely, arthralgias. Adolescents and adults, particularly female patients, may develop acute-onset symmetric joint pain, swelling, and stiffness in the proximal interphalangeal and metacarpophalangeal joints a week after the flu-like symptoms. As seen in this patient, a faint, erythematous, reticular rash may be present. However, most adolescents and adults do not have a rash. Diagnosis is often clinical but can be confirmed by serum serology (parvovirus B19 IgM antibodies); sampling of synovial fluid is rarely required.
Acute rheumatic fever, which presents 2-4 weeks after group A Streptococcus pharyngitis, causes migratory polyarthritis involving the larger joints (eg, knee, elbow). Skin findings include erythema marginatum and subcutaneous nodules.
The treatment of viral arthritis is supportive with nonsteroidal anti-inflammatory drugs for symptomatic relief. The prognosis is favorable; symptoms are self-limited and typically resolve within a few weeks. Parvovirus 19-associated arthritis is nonerosive and causes no long-term sequelae.