Ectopic pregnancy
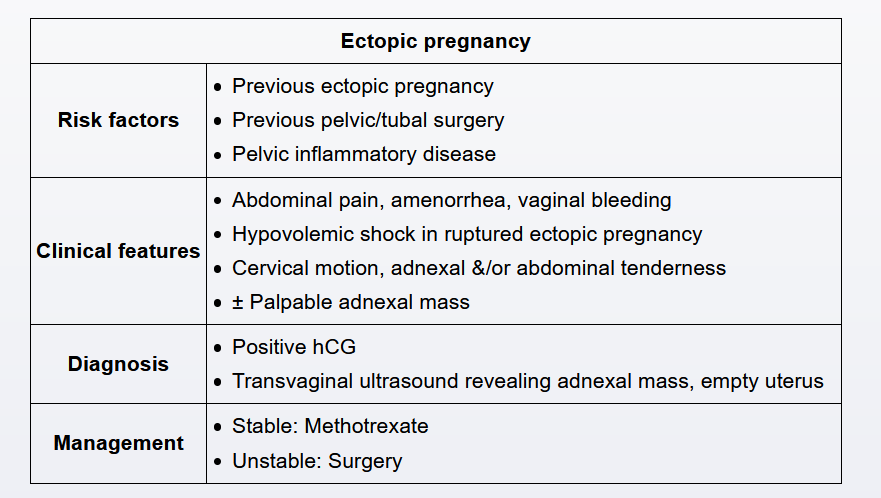
This patient has first-trimester vaginal bleeding and a positive pregnancy test, concerning for an ectopic pregnancy. Patients with a suspected ectopic pregnancy undergo evaluation with pelvic ultrasound and a β-hCG level. An early intrauterine pregnancy can be visualized by ultrasound when the β-hCG level is above the discriminatory zone (>1500 IU/L). This patient has a level above the discriminatory zone and an ultrasound revealing an empty uterus and a complex adnexal mass, which are diagnostic of an ectopic pregnancy.
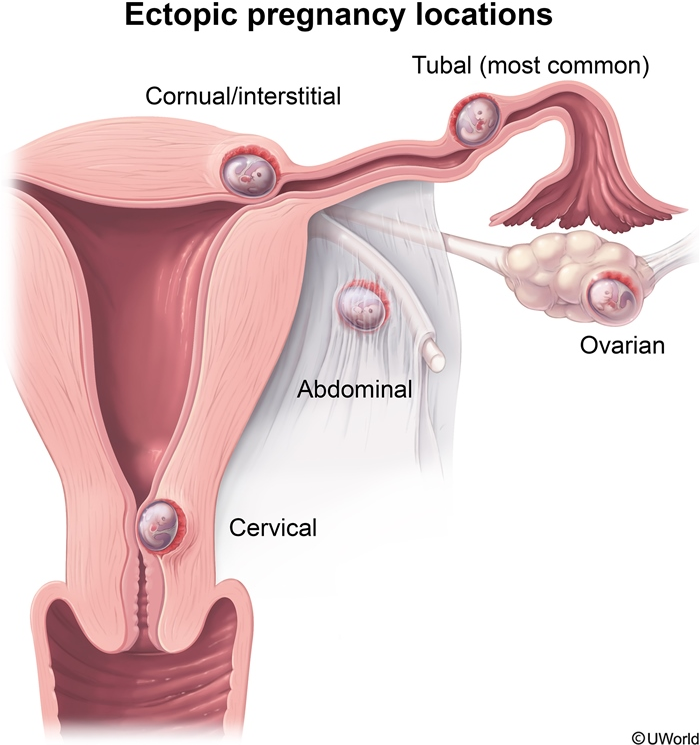
Symptoms of an ectopic pregnancy typically occur 6-8 weeks after the last menstrual period. In addition to vaginal bleeding, lower abdominal pain and amenorrhea may occur. The most common location for ectopic pregnancy is the ampulla of the fallopian tube; other implantation sites include the ovary, abdomen, and cornual region of the uterus. Risk factors include prior ectopic pregnancy, history of pelvic surgery, tobacco use, pelvic inflammatory disease, infertility, and in vitro fertilization. Treatment is with either medical (eg, methotrexate) or surgical management, depending on the patient's hemodynamic status.
The corpus luteum, a physiologic ovarian cyst, develops after ovulation and produces progesterone to maintain the pregnancy until the placenta develops. The cyst appears as an adnexal mass on ultrasound; however, an associated intrauterine pregnancy is also seen on ultrasound.
An early pregnancy of undetermined location occurs when a pregnancy cannot be visualized on ultrasound at a β-hCG level below the discriminatory zone (<1500 IU/L); it can be either ectopic or intrauterine. In stable patients, the β-hCG level is repeated every 48 hours to determine whether the increase is consistent with a normal pregnancy (>35% rise every 48 hours). Ultrasound is repeated when β-hCG is >1500 IU/L and an intrauterine pregnancy should be visualized.
This patient likely has an ectopic pregnancy based on first-trimester vaginal bleeding, lower abdominal pain, and a complex adnexal mass on transvaginal ultrasound. Risk factors for ectopic pregnancy include prior pelvic surgery, pelvic inflammatory disease, infertility, and tobacco use. Common implantation locations for an ectopic pregnancy include the fallopian tubes, ovaries, and cornua of the uterus.
As the ectopic gestation develops, extrauterine implantation sites cannot adapt to the rapid increase in gestational size, and rupture can occur. A ruptured ectopic pregnancy is a life-threatening emergency due to intra-abdominal bleeding (eg, anemia, free fluid in the posterior cul-de-sac) and resultant hemodynamic instability.
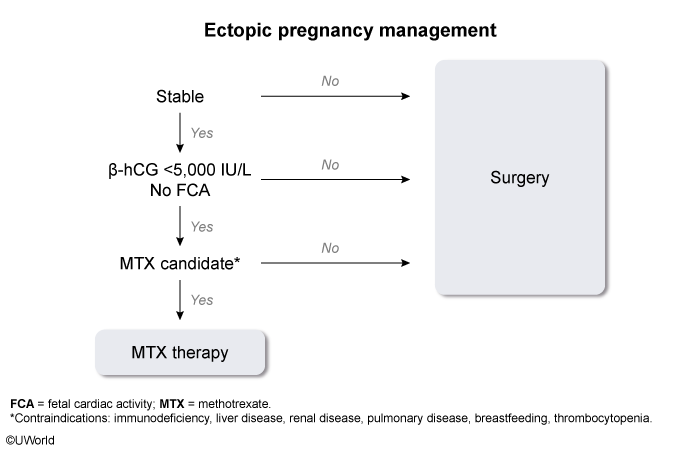
In hemodynamically stable, reliable patients, an ectopic pregnancy can be either expectantly or medically (eg, methotrexate) managed. Expectant management is primarily for patients with no adnexal mass on ultrasound and a β-hCG ≤200 IU/L. Methotrexate can be used in patients with no medical contraindications to therapy (eg, immunodeficiency, renal failure, active pulmonary disease) and a β-hCG ≤5,000 IU/L. In contrast, hemodynamically unstable patients, such as this one, require surgical management (eg, laparoscopy).