Celiac Disease
- related: GI
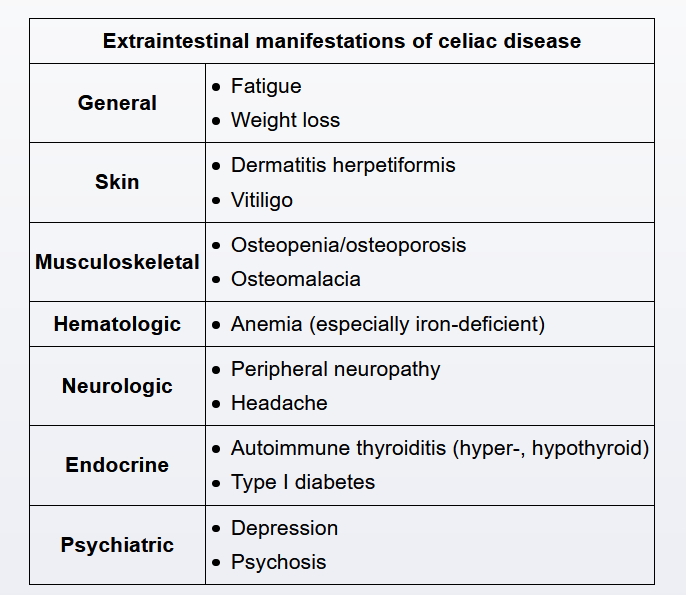
This patient has iron and vitamin D deficiencies despite consuming a nutritious diet, suggesting a malabsorption disorder. In a young patient with multi-nutrient malabsorption, the most likely explanation is celiac disease (gluten-sensitive enteropathy). The likelihood of celiac disease is even higher in this patient with vitiligo and a family history of hypothyroidism (associated autoimmune disorders). Although celiac disease is classically associated with prominent gastrointestinal symptoms such as diarrhea, a substantial subset of patients develops malabsorption with minimal or no gastrointestinal symptoms.
Screening for celiac disease is performed by checking the anti-endomysial antibody and anti-tissue transglutaminase antibody levels. Simultaneously checking both antibody levels increases the sensitivity for diagnosing the disease. The gold standard for diagnosis is small intestinal biopsy.
dermatitis herpetiformis:

Patients with untreated celiac disease are at risk for developing enteropathy-associated T-cell lymphoma (EATL), an aggressive hematologic malignancy that primarily affects the proximal jejunum. Manifestations typically begin with abdominal pain and B symptoms (eg, weight loss, fatigue, fever). Bowel obstruction, bowel perforation, and gastrointestinal bleeding are common as the disease progresses.
Most patients with EATL present late in the disease process when curative options are limited. As such, prognosis tends to be poor with median survival of only 10 months.
Vitamin D deficiency
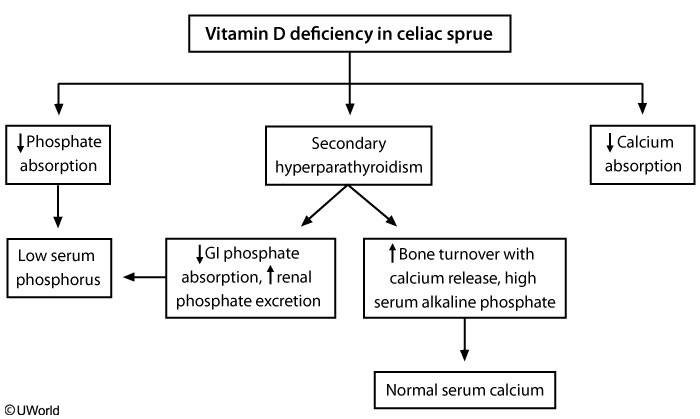
Uncontrolled celiac disease results in decreased gastrointestinal vitamin D absorption and subsequent vitamin D deficiency. This leads to hypocalcemia and secondary hyperparathyroidism with elevated parathyroid hormone (PTH) levels. PTH causes increased bone resorption and turnover, which increases serum alkaline phosphatase. PTH also decreases urinary calcium excretion and increases urinary phosphate excretion, which normalizes serum calcium but lowers serum phosphate.
Prolonged vitamin D deficiency leads to osteomalacia, inaccessible calcium stores in bone (unmineralized osteoid), and eventual hypocalcemia. Patients may develop pseudofractures, bone pain, or deformity. However, many patients can be asymptomatic with just the laboratory abnormalities. Thus, dual-energy x-ray absorptiometry scan is recommended for all patients with celiac disease for evaluation of bone loss. A gluten-free diet can partially reverse bone loss in some patients.
Management
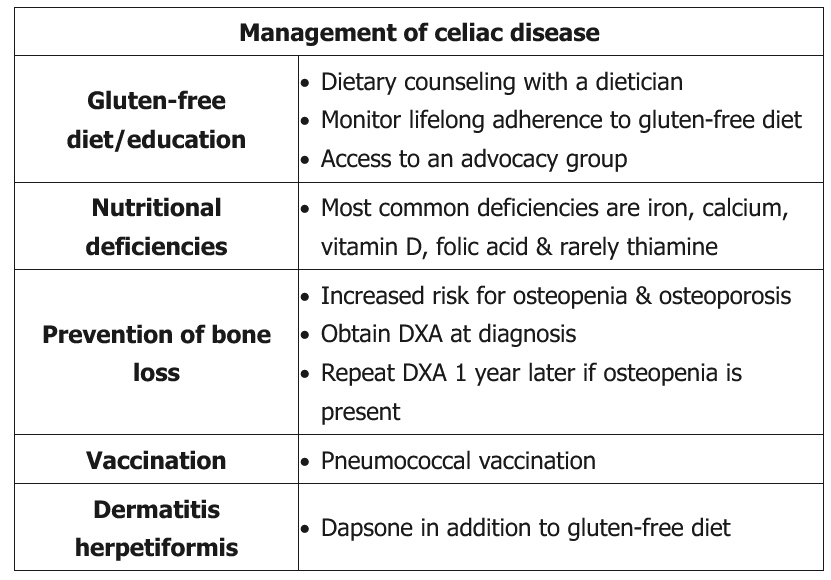
Patients with celiac disease are at risk of developing nutritional deficiencies, neuropsychiatric illness (eg, peripheral neuropathy, headache, depression), and skin disorders (eg, dermatitis herpetiformis). In addition, although the pathogenesis is unknown, hyposplenism has been reported and is believed to be relatively common. Therefore, pneumococcal vaccination is recommended in patients with celiac disease, regardless of age.
Most of the complications of celiac disease can be prevented by strict lifelong adherence to a gluten-free diet; however, nutritional deficiencies and bone loss (primarily due to vitamin D deficiency) should be screened for and treated appropriately.