COPD
- related: Pulmonology, Asthma
- tag: #note
MISC
Epidemiology
- 5% of the U.S. population
Pathophysiology
- airflow obstruction that's not reversible
- inflammatory condition
- cigarette smoke/irritants activate macrophage/epithelial cells
- neutrophil chemotactic factors released
- proteases destroys lung parenchyma
- protease inhibitors (a1-antitrypsin) reduced in COPD
- oxidative stress: inflammation, tissue destruction
- ultimately: fibrosis of small airway, reduced elastic recoil, static hyperinflation
- ability to exhale decreases
- inhalation initiated before exhalation => hyperinflation, air trapping
Risk Factors
- smoke exposure
- air pollution: cooking with biomass fuel indoor
- occupational chemical/dust
- a1-antitrypsin deficiency
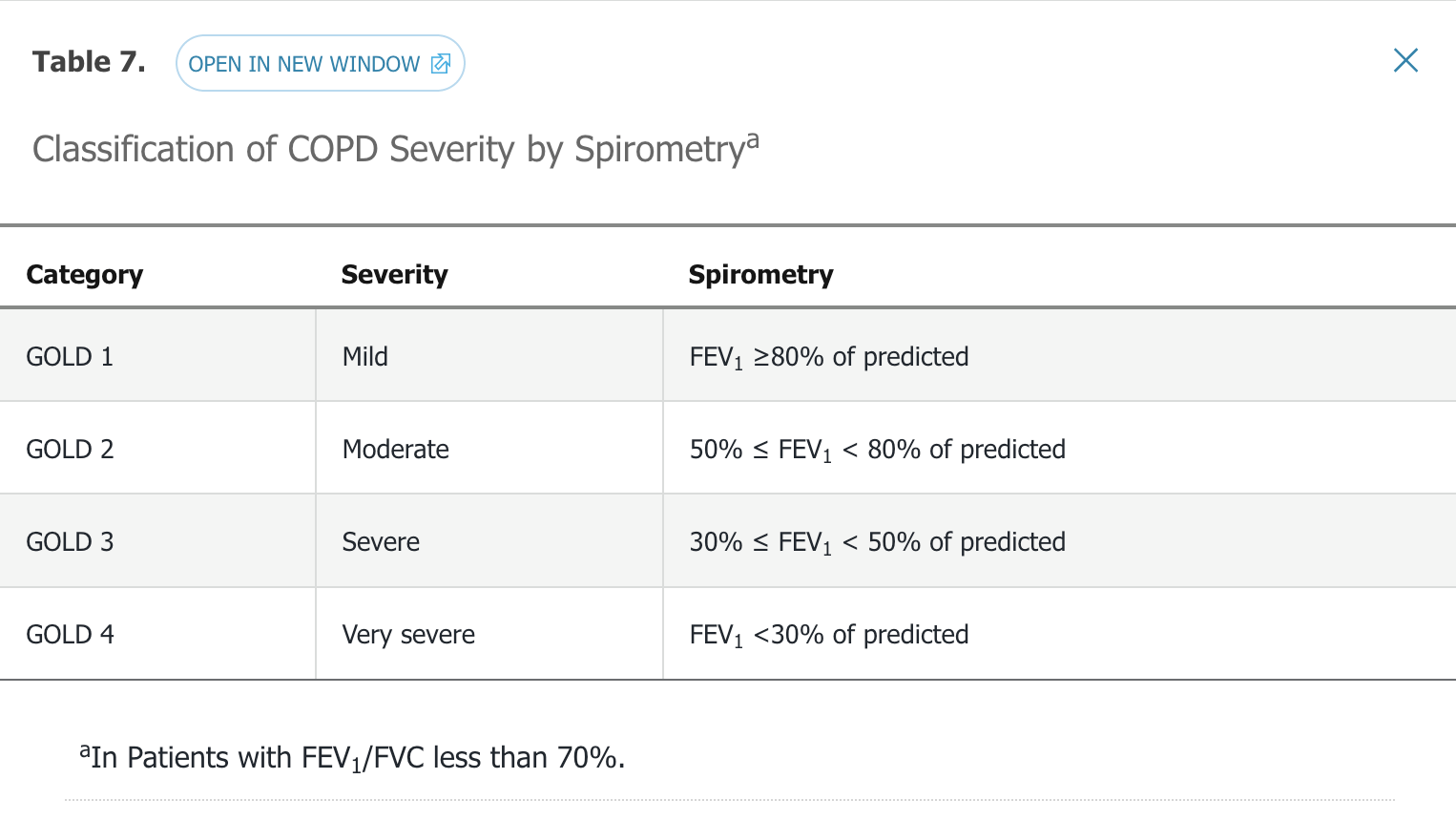
Staging
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)
- degree of airflow obstruction from spirometry
- number of previous exacerbation
- symptoms
- BODE index: predict outcome and response
- BMI
- airflow obstruction: FEV1 percent predicted
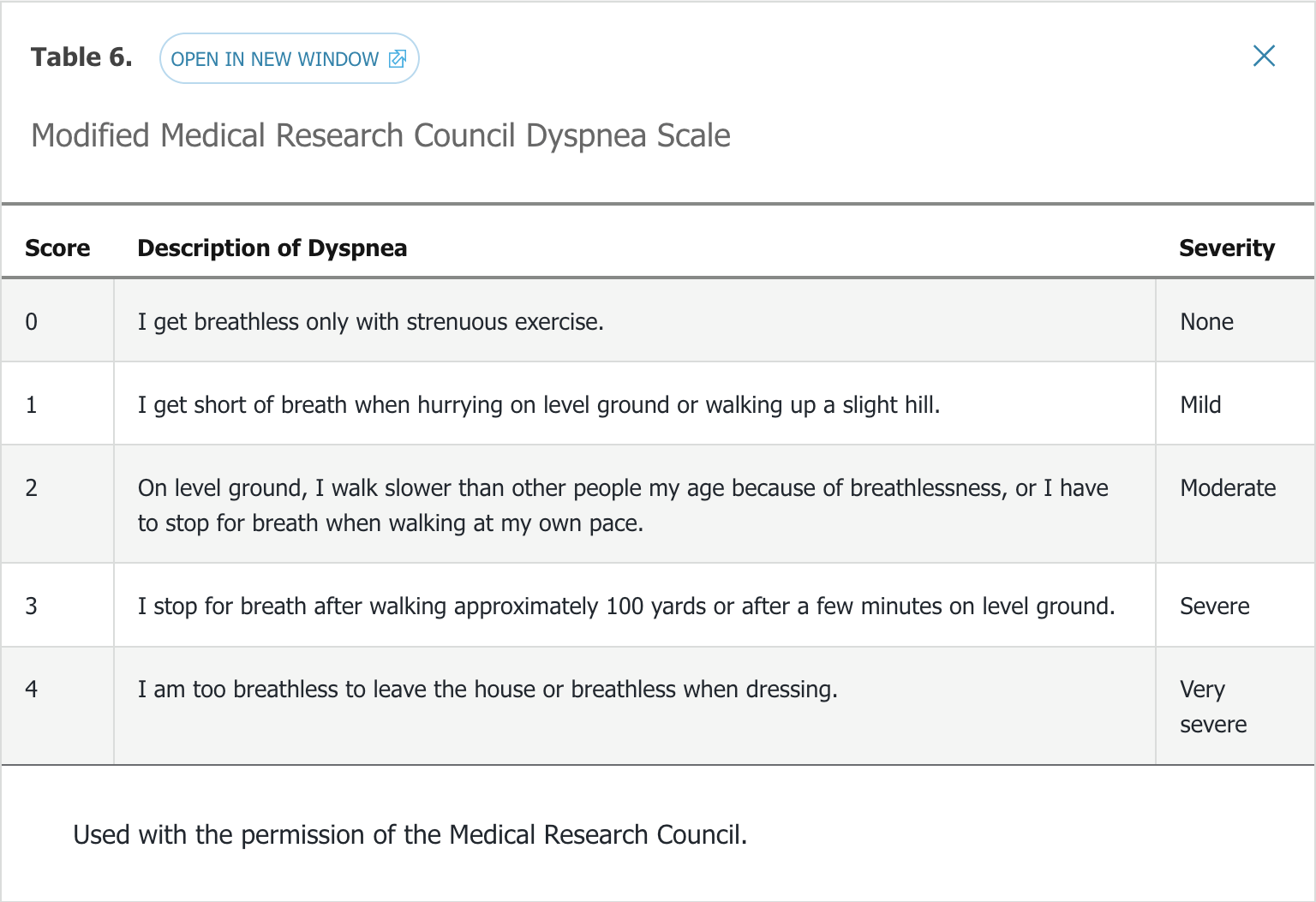
- dyspnea: modified British Medical Research Council (mMRC), perceived dyspnea
- exercise capacity: 6 minute walk test. Used to approximate 4 year survival and risk for hospitalization
Diagnosis
- do not screen for asymptomatic pts
- diagnosis made with post-bronchodilator FEV1/FVC ratio less than 0.7 (asthma has fully reversible airflow obstruction)
- lung volume/DLCO not required for diagnosis but could help with severity determination
Disease Assessment
- determine disease severity by
- COPD Assessment Test (CAT)
- Clinical COPD Questionnaire (CCQ)
- mMRC scale
- GOLD uses CAT or mMRC
- BODE uses mMRC
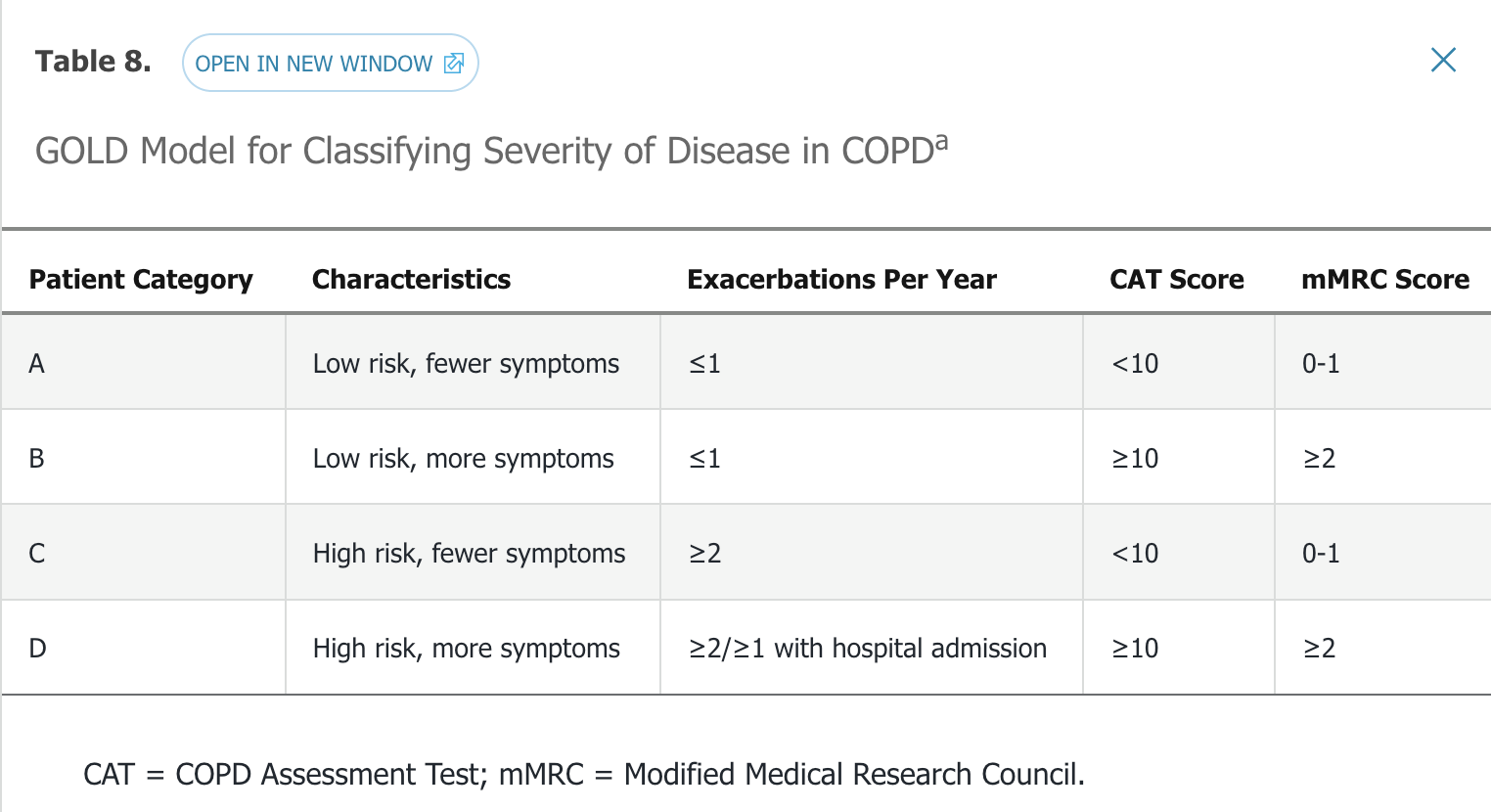
- high risk
- 2 or more exacerbation in 1 year
- FEV1 < 50% predicted
- people hospitalized for acute exacerbation
- a1-antitrypsin level: obtain for pts under 45 with strong family hx, without risk factor, basilar emphysema, associated liver disease, panniculitis
Medications
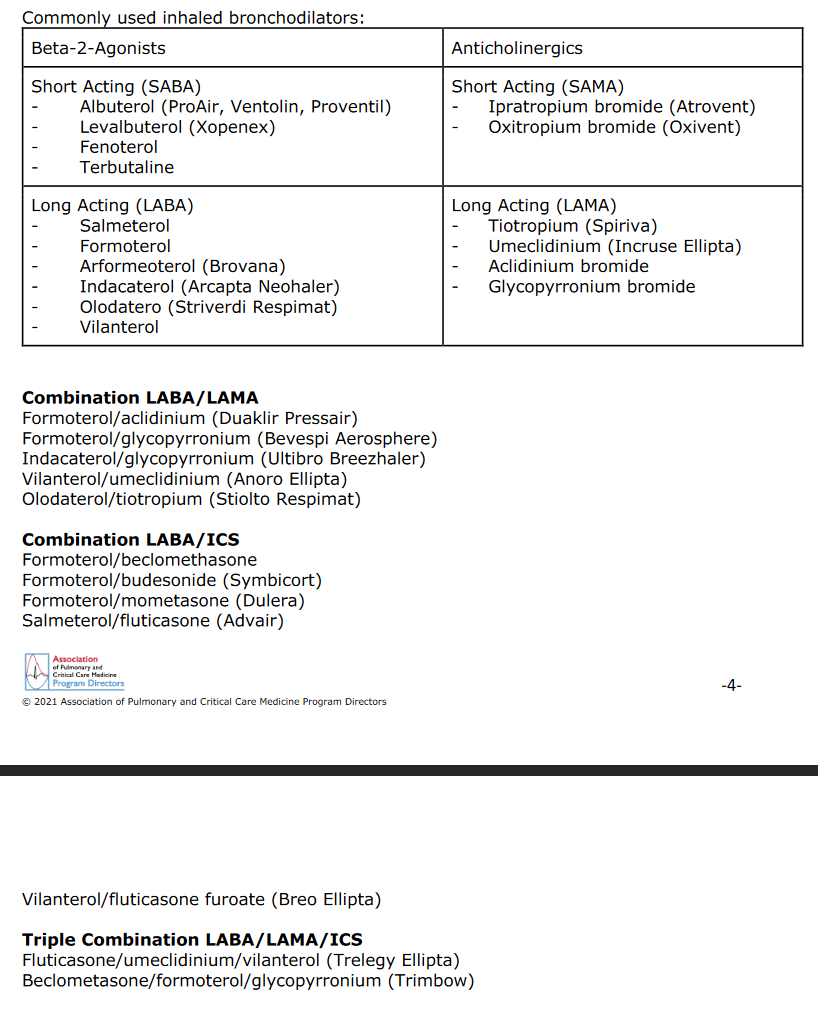
Bronchodilators
- Inhaled SABA
- tachycardia, hypokalemia
- albuterol, fenoterol, levalbuterol, metaproterenol, pirbuterol, terbutaline
- inhaled SAMA
- dry mouth, mydriasis, tachycardia, tremors, rarely glaucoma
- ipratropium
- inhaled LAMA
- not to be used with ipratropium
- use when SABA provide insufficient control for pt with FEV1 < 60%
- tiotropium, aclidinium, umeclidinium, glycopyrronium
- inhaled LABA
- tremors, tachycardia
- maintenance therapy
- do not use for acute exacerbation/bronchospasm
- salmeterol, formoterol, aformoterol, indacaterol, olodaterol
- methylxanthines
- improve functional capacity, reduce exacerbation
- tachycardia, nausea, vomiting, sleep disturbance
- narrow therapeutic index
- overdose: fatal with seizure/arrythmia
- use as maintenance therapy
- add after LABA
- theophylline, aminophylline
- oral beta agonists
- maintenance therapy, rarely used, for people who can't use inhalers
- albuterol, metaproterenol, terbutaline
- oral PDE4 inhibitors
- diarrhea, nausea, bachache, decreased appetite, dizziness
- reduce sx in severe COPD with chronic bronchitis and hx of exacerbation, reduce frequency of exacerbation
- do not use with methylxanthines
- very expensive
- Roflumilast
- Steroids
- increase pna risk
- inhaled:
- best when use in conjunction with LABA
- fluticasone, budesonide, mometasone, ciclesonide, beclomethasone
- oral: prednisone, prednisolone
- LABA + glucocorticoid
- fluticasone/salmeterol: maintenance, prevention
- budesonide/formoterol: maintenance
- SABA + SAMA
- milder disease with fewer sx
- fenoterol/ipratropium
- salbutamol/ipratropium
- ICS + utra LABA
- fluticasone/vilanterol: not used for acute treatment
- LAMA + ultra LABA
- umeclidinium/vilanterol: not used for acute
- macrolide
- long term therapy reduce frequency of exacerbation
Strategies
- Either inhalers or nebulizers
- People who can take deep breaths should use inhalers, otherwise nebulizer
- Combine steroid/beta agonist with muscarinic antagonist:
- Symbicort with Spiriva
- Advair with Spiriva
- Trelegy: symbicort, advair, and spiriva. Less expensive, once a day
- Use nebulizer when can't take deep breaths:
- beta agonist: brovana
- Steroid: pulmicort
- Antimuscarinic agent: ipratropium
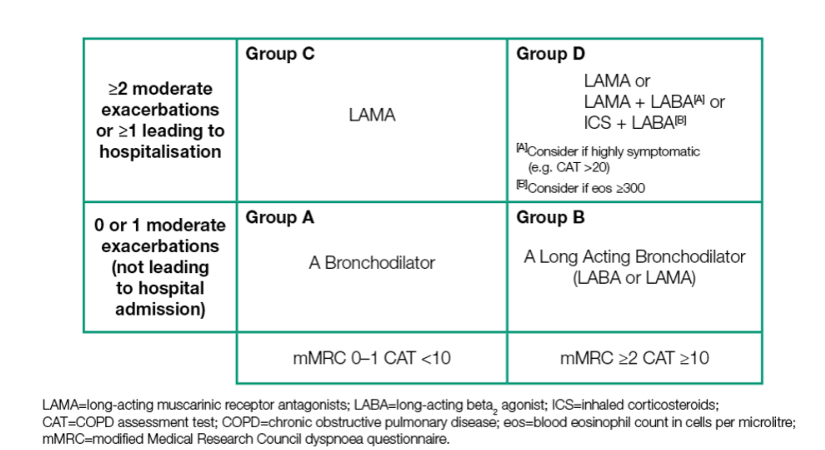
Management by Group
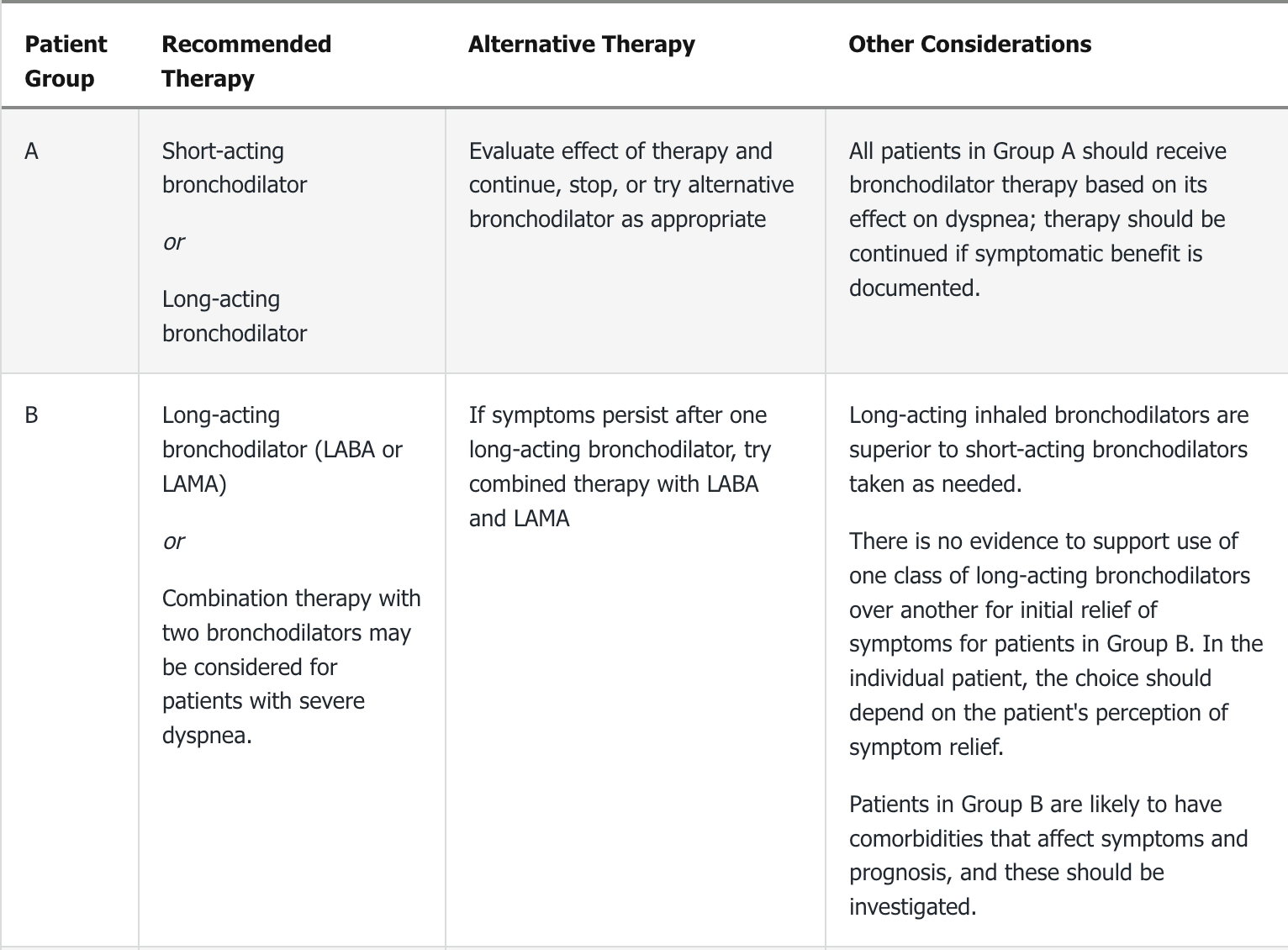
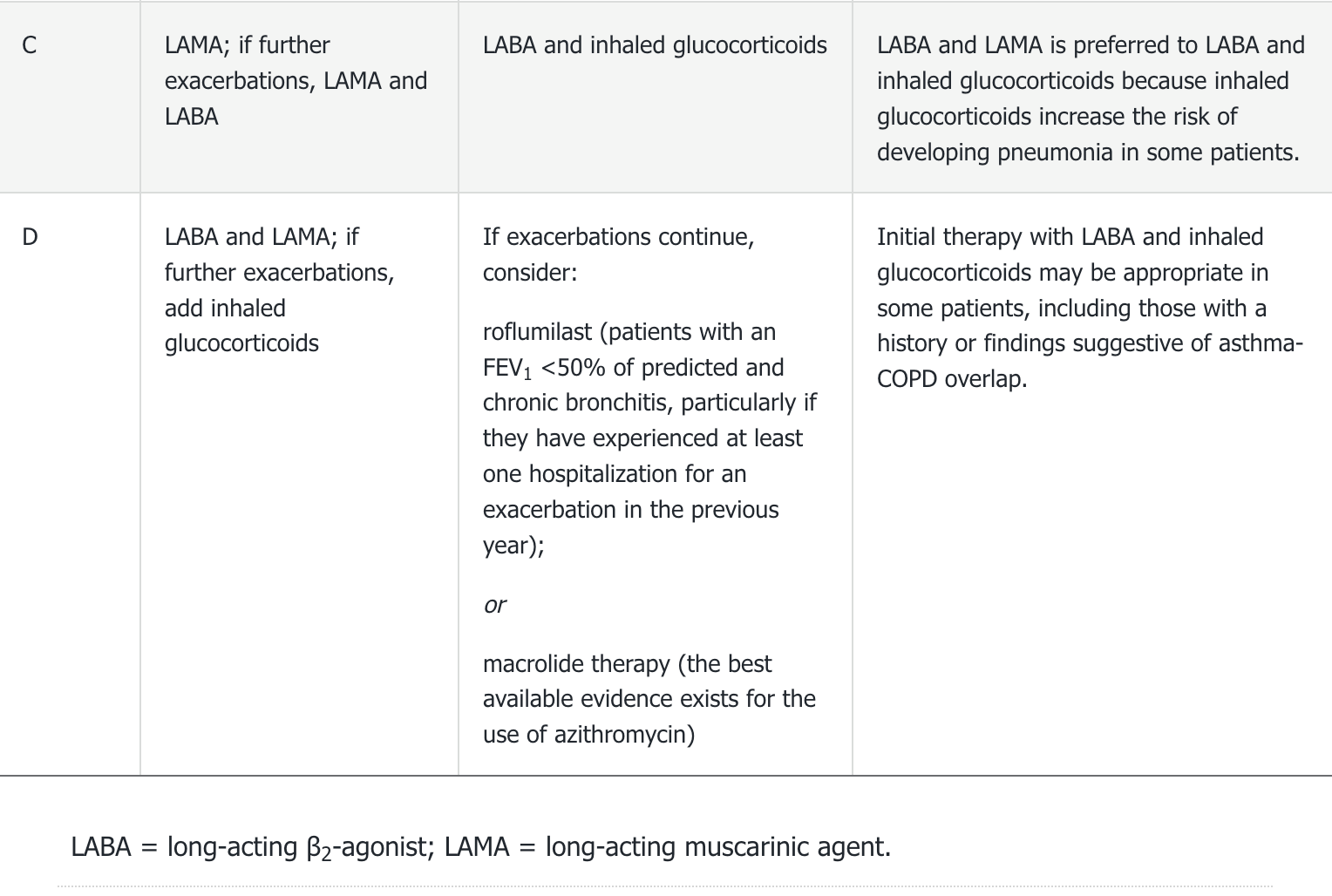
- SABA and SAMA can be used as monotherapy but better combined
- If SABA insufficient to control sx, LABA or LAMA can be added
- Do not use LAMA as monotherapy in pt with asthma-COPD overlap, add ICS due to increased mortality
- ICS used usually only with LABA/LAMA
- Do not use ICS alone unless pt can't use LABA/LAMA
- triple therapy: LABA + LAMA + ICS
Immunization
- annual flu
- PPSV23
-
65: PCV13
Pulmonary Rehabilitation
Pulmonary rehabilitation is a comprehensive program that combines exercise training, nutritional support, education, and social support for patients with chronic lung conditions. It has been shown to relieve symptoms, improve quality of life, and decrease frequency of hospitalizations in patients with COPD. Clinicians should consider adding this to appropriate medical therapy in symptomatic patients with an FEV1 of less than 50% of predicted and to patients recovering from COPD exacerbation; particularly those recently hospitalized or treated with systemic steroids would benefit from pulmonary rehabilitation.
Oxygen Therapy
The use of supplemental oxygen has been shown to improve quality of life and decrease mortality in patients with COPD and resting hypoxemia with an arterial PO2 of 55 mm Hg or less, or oxygen saturation as measured by pulse oximetry of 88% or less. Patients with cor pulmonale, heart failure, or erythrocytosis should be offered the use of supplemental oxygen if the Po2 is 59 mm Hg or less or the oxygen saturation is 89% or less. Some patients may not qualify for oxygen at rest but may desaturate during sleep, exertion, or air travel. Supplemental oxygen is typically prescribed if the oxygen saturation as measured by pulse oximetry falls below 89% in these situations, but the benefits are less defined.
Noninvasive Mechanical Ventilation
Noninvasive mechanical ventilation (NIV), also termed noninvasive positive pressure ventilation (NIPPV), can be used for acute and chronic respiratory failure. For patients with a COPD exacerbation and acute hypercapnic respiratory failure with acidosis, NIV improves symptoms and reduces intubation rates, length of hospital stay, and mortality. It may also be beneficial in COPD patients with pneumonia, to help with discontinuing mechanical ventilation, and for palliative care. It does not replace intubation and mechanical ventilation in critically ill patients, comatose patients, or patients who have sustained a cardiac arrest. NIV is generally well tolerated, and improvement of the pH and PCO2 within 1 to 2 hours predicts success. The benefit of using NIV in the treatment of chronic respiratory failure or in the outpatient setting is less clear. It may, especially if used at night, provide additional symptomatic relief when added to medical therapy in patients with severe COPD.
Prognosis and Goals of Care
The current GOLD initiative recommends combining the degree of airflow limitation using the post-bronchodilator FEV1 with the number of exacerbations and the patient's symptoms to classify the severity of disease. This will allow the clinician to guide escalation or de-escalation of medical therapies as appropriate.
The BODE index can be used as a prognostic indicator for patients with COPD. Using the BMI, the post-bronchodilator FEV1 percent of predicted, dyspnea as defined using the mMRC scale (see Table 6), and the distance walked on a 6-minute walk test, it is possible to approximate the patient's 4-year survival. In patients with severe disease with an overall poor prognosis, referral for hospice and palliative care can provide significant improvements in symptom burden.
Palliative care can significantly aid in symptom management in patients with COPD at any stage of disease. Patients experience not only dyspnea, but also anxiety and depression, which may also be addressed. Opioids are commonly used to treat dyspnea that persists despite medical therapy. Current guidelines suggest a patient with severe COPD — defined by disabling symptoms despite medical therapy, progression of disease as evidenced by increasing emergency department evaluations or hospitalizations, and hypoxemia or hypercapnia — should be considered for hospice care.
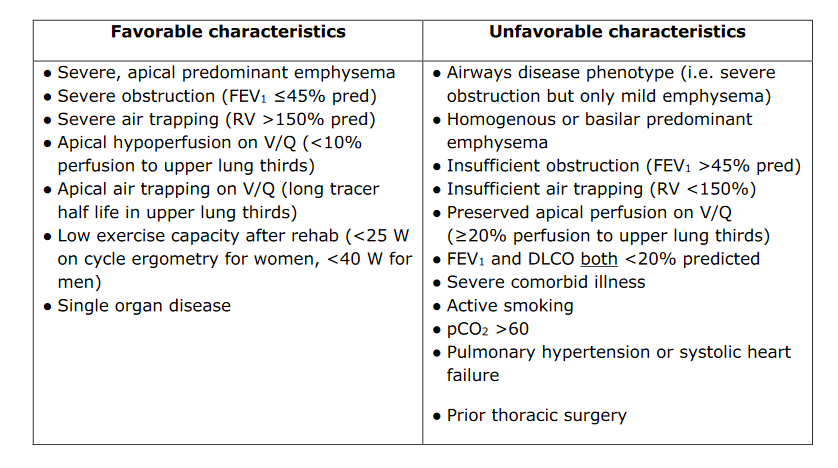
Lung Volume Reduction Therapy
The National Emphysema Treatment Trial (NETT) demonstrated that patients with upper lobe–predominant and significant exercise limitations even after participation in a pulmonary rehabilitation program had improved quality of life, exercise tolerance, pulmonary function, and survival with lung volume reduction surgery. A key finding from NETT was that patient selection was critical to success and that patients with an FEV1 of less than 20% of predicted, a diffusing capacity of less than 20% of predicted, or non–upper lobe predominant disease had a high operative mortality and should not be offered lung volume reduction surgery. The procedure should be considered in patients with upper lobe–predominant who have low exercise tolerance despite maximal medical therapy and completion of a pulmonary rehabilitation program. Nonsurgical lung volume reduction procedures, including bronchoscopic placement of endobronchial one-way valves, plugs, or coils; administration of biologic sealants; and thermal ablation of the airway are being studied for treatment of emphysematous changes in patients with COPD. Early results suggest patients with severe air trapping and hyperinflation may get the most benefit from these new techniques.
Lung Transplantation
Referral for lung transplantation can be considered in patients with severe COPD. The decision to refer should depend on the patient's life expectancy, quality of life, and patient preferences. In general, patients at high risk of dying in less than 2 years who have a high probability of 90-day postoperative survival are candidates. Patients with an elevated BODE index (5 or 6), resting hypoxemia, hypercapnia, an FEV1 of less than 25% of predicted, or significant exercise limitation despite medical therapy, smoking cessation, and participation in a pulmonary rehabilitation program may be referred for evaluation for lung transplantation. Transplantation improves quality of life, and the median life expectancy is 5.7 years.
Acute Exacerbations
- increase in severity or frequency of cough
- worsening dyspnea
- increase or change in character of sputum
- triggers: infection, smoking exposures
- strep pneumo, H flu, moraxella, mycoplasma
management
- sputum clx: not obtained because rarely affects management
- SABA with or without SAMA
- oral glucocorticoids decrease length of stay, 40 mg 5 days
- abx: moderate or severe exacerbation or mild exacerbation with change in sputum
Antibiotics are generally not recommended for management of acute bronchitis in otherwise healthy individuals as most exacerbations are of viral etiology. However, guidelines from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommend antibiotic therapy for patients who have a COPD exacerbation with any two of the following features: increased sputum purulence, increased sputum volume, or increased dyspnea. Antibiotics are also recommended for those requiring mechanical ventilation (noninvasive or invasive).