Asthma
- related: Pulmonology
Asthma
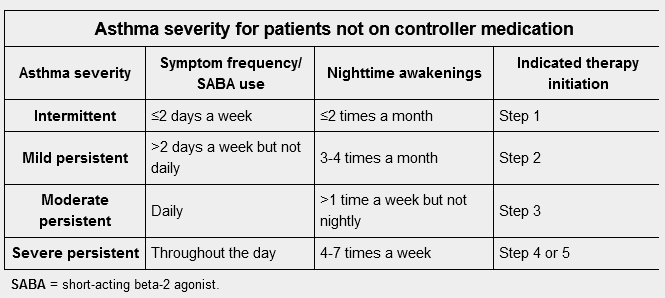
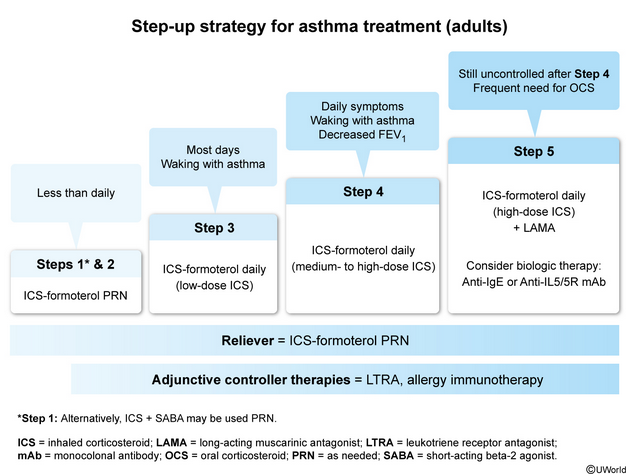
This patient has intermittent asthma symptoms (less than daily, no waking, normal postbronchodilator FEV1). Guidelines recommend treatment with an inhaled corticosteroid (ICS) (eg, budesonide) plus formoterol as needed. This strategy addresses leukocyte-induced bronchoconstriction as the central pathophysiology of asthma:
-
ICSs target leukocytes and should be included at every step of asthma, even for patients with intermittent symptoms.
-
Formoterol targets bronchoconstriction and is the preferred long-acting beta agonist (LABA) because it has fast-onset kinetics (<5 min) and is therefore effective for acute relief.
Short-acting beta agonists (SABAs) (eg, albuterol) are an alternative to formoterol in patients with very infrequent intermittent symptoms, but ICSs should be taken when a SABA is used. SABA monotherapy increases the risk for future exacerbation, probably because the underlying airway inflammation is not addressed. Frequent SABA use also down-regulates airway beta-2 receptors, which dampens bronchodilator responsiveness over time.
Long-acting antimuscarinic agents (LAMA) (eg, tiotropium) are indicated for step-up therapy in patients with uncontrolled asthma despite scheduled high-dose ICS-formoterol. LAMA monotherapy is preferred as initial treatment for most patients with COPD; combined LAMA/LABA therapy (eg, umeclidinium-vilanterol) is used for patients who have a higher symptom score and a history of frequent exacerbations (COPD Group D).