Analgesics

- Utopia: opiates
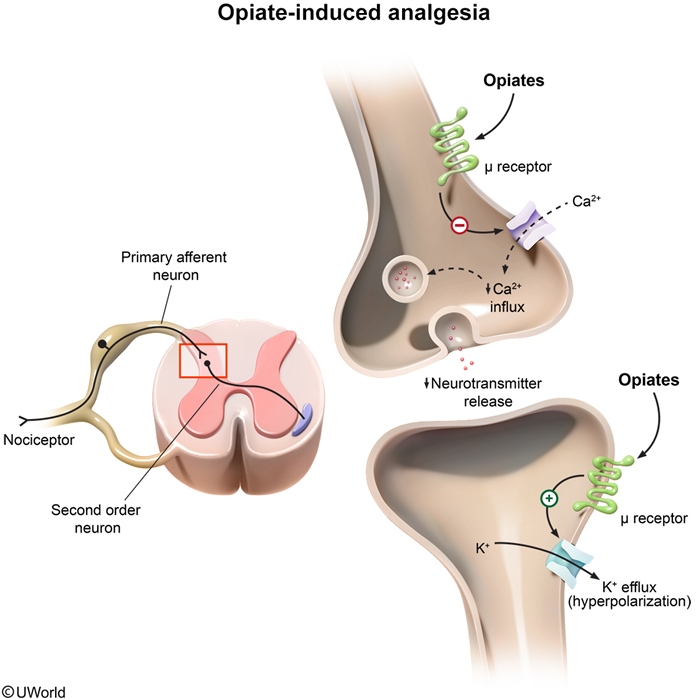
- u-message: opioid receptor (mediates most clinical and adverse effects: e.g. analgesia, sedation, constipation, respiratory depression)
- Open banana barrels: opiate receptors open K+ channels
- Closed Calci-Yum ice cream cooler: opiate receptors close VG Ca2+ channels on presynaptic
- Disconnected presynaptic wire: closure of presynaptic VG Ca2+ channels prevents release of neurotransmitters (e.g. glutamate, acetylcholine, norepinephrine, serotonin, substance P), stopping pain signa
- Pain-relieving acupuncture :u-opioid receptor mediates analgesia

- Fantasy sign:: fentanyl (opioid analgesic), post operative, chronic pain
- More fun: morphine (opioid analgesic)
- Distant tram: tramadol (a weak u-opioid receptor agonist used to manage chronic pain)
- North-South compass: tramadol also inhibits reuptake of norepinephrine and serotonin

- Removed muddy slippers: opioids (e.g. loperamide, diphenoxylate) can be used as antidiarrheals. (loperamide doesn't cross BBB, no central SE)
- Lop-eared rabbit: loperamide (opioid antidiarrheal)
- Loping back and forth: loperamide increases colonic phasic segmentation (increase stool transit time)
- Dolphins hoping back and fourth: diphenoxylate (opioid antidiarrheal)

- Barcode: codeine (opioid antitussive)
- Orphan: dextromethorphan (opioid antitussive)
- Tethered nomadic camel: dextromethorphan antagonizes NMDA receptors

- Cerebral towel: opiates cause CNS depression (e.g. sedation), especially elderly
- Deflated lung vest: opiates can cause respiratory depression, dose dependent
- Colon u-massage table: u-opioid receptors are located in the GI tract (delay stool transit), constipation
- Plunger: opiates can cause constipation
- Constricted hood: opiates cause miosis (constricted pupils)
- Biliary tree: opiates can cause biliary colic (contract biliary smooth muscle)
- "All are welcome": patients may develop tolerance to opiates
- "Out of order": tolerance does not develop for miosis or constipation
- Causing pain: opiate induced hyperalgesia can occur with chronic use
- bradycardia, hypotension from histamine release

- Anxious, hot, and moist: opioid withdrawal (rhinorrhea, lacrimation, yawning, hyperventilation, hyperthermia, muscle aches, vomiting, diarrhea, anxiety)

- DONE timer: methadone (long acting opioid used to attenuate withdrawal symptoms)
- Long tapering flag: methadone and buprenorphine have a long half lives (used in opioid detoxification), less withdrawal
- Blueprint: buprenorphine (long acting partial u-opioid agonist used to attenuate withdrawal symptoms)

- Irritable, moist, tachypneic baby: neonatal abstinence syndrome (diarrhea, sweating, sneezing, crying, tachypnea, irritability)

- Partial ussage: partial u-opioid agonists (e.g. buprenorphine, nalbuphine, butorphanol)
- Bluefin: buphin in names of partial u-opioid agonists (e.g. buprenorphine, nalbuphine, butorphanol)
- Falling into the withdraw spa: partial u-opioid agonists can induce withdrawals

- No lax zone: naloxone (u-opioid antagonist) used to reverse acute opioid toxicity (can precipitate withdrawals)
- No tricks zone: naltrexone (u-opioid antagonist) helps maintain abstinence in heroin addicts
- Tempting alcohol: naltrexone (u-opioid antagonist) helps reduce cravings for alcohol and nicotine
- Getting fit, exercise: naltrexone (u-opioid antagonist) can help with weight loss
Propofol, etomidate, ketamine, IV anesthetics

- Ivy: IV anesthetics (e.g. propofol, etomidate, ketamine)

- "Prospero…fall asleep!": propofol (IV anesthetic for induction and maintenance), lipophilic, rapid induction
- "Introducing": propofol can be used for induction of anesthesia
- "Maintain": propofol can be used for maintenance of anesthesia
- Cab-A: propofol and etomidate potentiate chloride current through the GABAA receptor complex
- Dilated sleeves and pants: propofol causes profound vasodilation (arterial and venous) -> hypotension

- "Intimidator": etomidate (IV anesthetic for induction)
- "Introducing": etomidate can be used for induction of anesthesia
- Cab-A: propofol and etomidate potentiate chloride current through the GABAA receptor complex
- Stabilized patient: etomidate preserves cardiovascular stability, minimum changes to BP, CO, HR

- "snaKE TAMINg": ketamine (IV anesthetic for induction)
- "Introducing": ketamine can be used for induction of anesthesia
- Hitched nomadic camel: ketamine inhibits the NMDA receptor complex
- Dissociative trance: ketamine causes "dissociative anesthesia" (eyes remain open with a slow nystagmic gaze)
- colors, glasses, snake shadows: ketamine can cause unpleasant emergence reactions (e.g. vivid colorful dreams, hallucinations, out of body experiences)
- Stimulated heart cobra: ketamine causes cardiovascular stimulation (e.g. increased blood pressure, heart rate, cardiac output)

- Ben's diner: benzodiazepines (IV anesthetics used perioperatively)
- Bowel water pump: benzodiazepines are used for conscious sedation for minor procedures (e.g. colonoscopy)
- Barber: IV barbiturates (e.g. thiopental)
- "Introducing": IV barbiturates (e.g. thiopental) can be used for induction of anesthesia
- "The ol' quick shave": thiopental is a fast acting barbiturate (highly lipid soluble)
Inhaled Anesthetics, great for kids

- Inhaled anesthetics, great for children
- "laughing" girl: nitrous oxide (N2O - a gaseous anesthetic)
- Air tank in water: volatile anesthetics (e.g. enflurane, isoflurane, halothane) are liquid at room temperature

- Balloon flower: volatile anesthetics (e.g. enflurane, isoflurane, halothane) are fluorinated

Uptake from alveoli into circulation and distribution to tissues:
- Impeded by ball pit: less soluble inhaled anesthetic (e.g. N2O)
- Passed out earlier: less soluble inhaled anesthetics (e.g. N2O) have a faster onset of action, immediate saturation. Poor solubility: amt needed for saturation is small. Brain saturated very quickly
- Immediate rescue: less soluble inhaled anesthetics (e.g. N2O) have a faster recovery
- Moving freely in ball pit: highly soluble inhaled anesthetic (e.g. halothane) in blood
- Passed out later: more soluble inhaled anesthetics (e.g. halothane) have a slower onset of action
- Long tapering flag: more soluble inhaled anesthetics (e.g. halothane) have a longer duration of action

- Partition>>>: higher blood:gas partition coefficient (e.g. halothane) -> higher solubility -> slower onset of action

- Steeper arterial tension curve (e.g. N2O) -> lower blood:gas partition coefficient -> lower solubility -> faster onset of action. Partial pressure of N2O raises rapidly
- Less steep arterial tension curve (e.g. halothane) -> higher blood:gas partition coefficient -> higher solubility -> slower onset of action

- Mac and cheese: minimum alveolar concentration (MAC), percentage of anesthetics in inspired gas mixture that renders 50% pts unresponsible
- 1 out of 2 kids unresponsive: MAC corresponds to the dose of anesthetic that causes 50% of patients to become unresponsive to painful stimuli, corresponds to ED50
- Inverted bowl of potent mac and cheese: 1/MAC corresponds to the potency of an inhaled anesthetic. Lower the MAC, the more potent

- Deflating heart balloon: inhaled anesthetics can cause myocardial depression (leading to decreased cardiac output and hypotension)
- Deflating lung balloons: inhaled anesthetics can cause respiratory depression (leading to decreased minute ventilation and hypercapnia)
- Red brain wig: fluorinated anesthetics increase cerebral blood flow (decrease cerebral vascular resistance), increases ICP

- Cracked liver: halothane can be hepatotoxic (e.g. massive hepatic necrosis)

- Smacked in the flank: enflurane can be nephrotoxic
- Shaking: enflurane can induce seizures

- Magnificent birthday: malignant hyperthermia (skeletal muscle hypersensitivity to volatile anesthetics), not N2O
- "Sucks": succinylcholine (depolarizing muscle relaxant) can also causes malignant hyperthermia
- Defective RYAN: malignant hyperthermia is related to a defect in ryanodine receptors (RyR) in the sarcoplasmic reticulum
- Flame theme: defective RyR release excess Ca2+ ->excessive ATP dependant uptake by the SR -> heat production
- Bite out of muscle: excessive heat production and consumption of ATP induces muscle damage (e.g. rhabdomyolysis), can also present with tachy/hypertension after surgery

- Trampoline: dantrolene (muscle relaxant) treats malignant hyperthermia
- Blocking Ryan: dantrolene blocks ryanodine receptors