Abortions
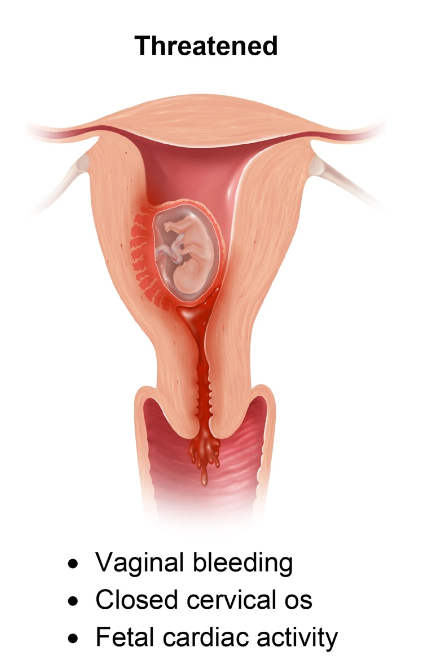
A threatened abortion presents at <20 weeks gestation with vaginal bleeding, a closed cervix, and a normal fetal heartbeat on ultrasound.
Placenta Abruptio
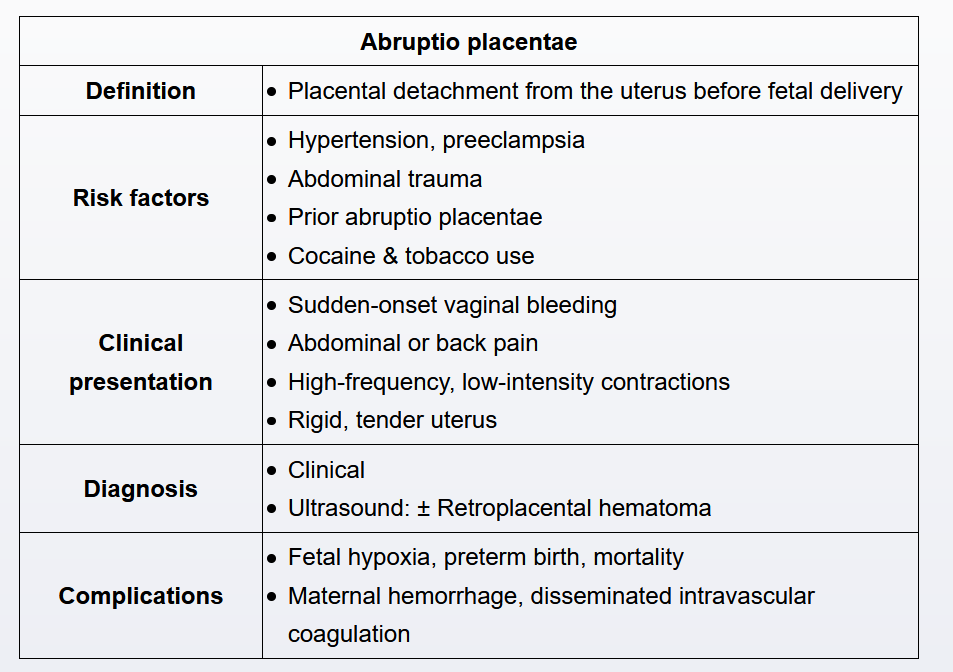
This patient presents in the third trimester with painful vaginal bleeding; a tender, rigid uterus; and a fetal heart rate tracing with late decelerations—a presentation consistent with abruptio placentae. Abruptio placentae, the partial or complete separation of the placenta from the uterus prior to fetal delivery, is associated with maternal trauma, hypertension, tobacco or cocaine use, and a history of prior abruptio placentae.
Abruptio placentae occurs when maternal vessel rupture at the uteroplacental interface causes intrauterine bleeding. This bleeding causes the detachment of the placenta from the uterus, an increase in the intrauterine pressure (eg, tender, distended uterus), and uterine irritability (eg, high-frequency, low-intensity contractions). Some abruptio placentae are self-limiting and contained whereas others progress as the bleeding and placental separation continue. As the degree of placental separation increases, the risk of fetal compromise and mortality from hypoxia (eg, late decelerations in the fetal heart rate tracing) also increases. Maternal complications include hemorrhage and disseminated intravascular coagulation. An acute abruptio placentae with active bleeding is an indication for delivery; the mode of delivery is dependent on both maternal and fetal stability.
Placenta Previa
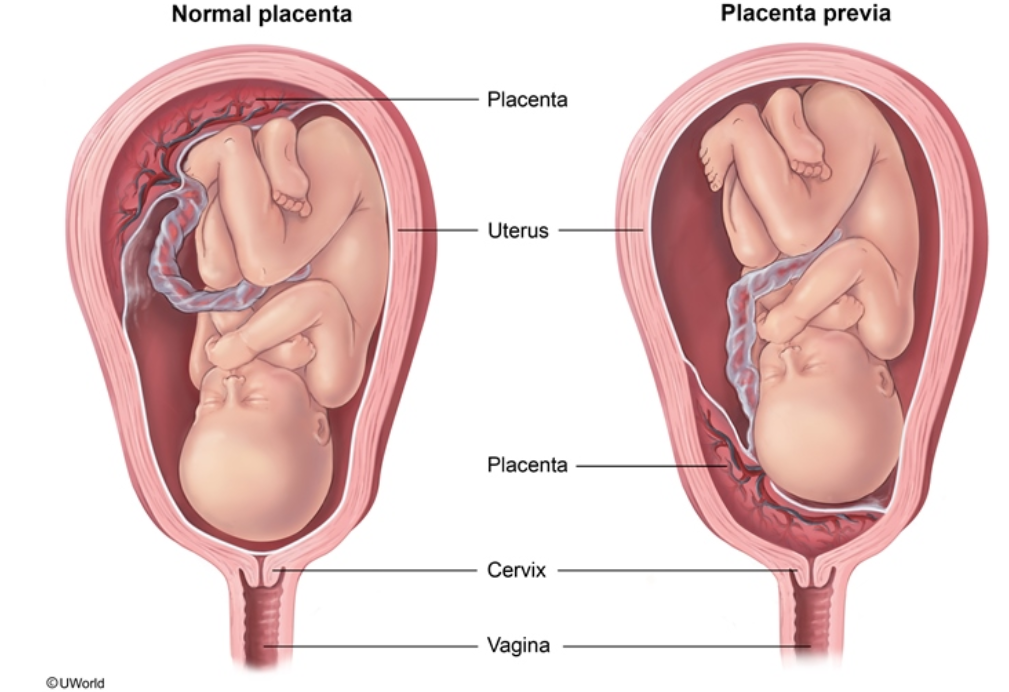
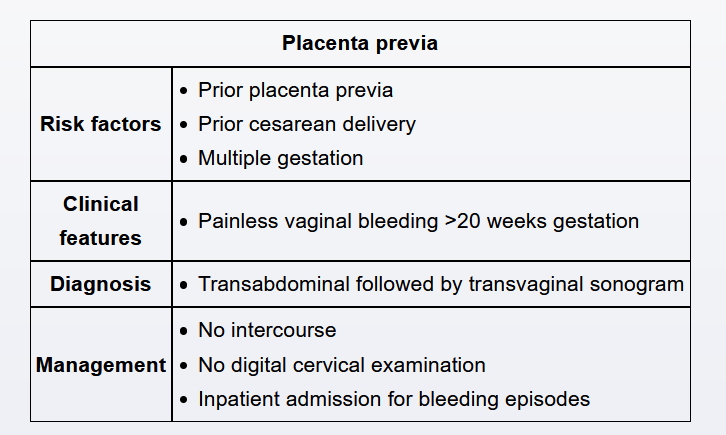
This patient has painless vaginal bleeding at >20 weeks gestation, a presentation consistent with placenta previa. Placenta previa, the extension of the placenta over the internal cervical os, is associated with an increased risk of obstetrical hemorrhage and preterm delivery. Because the bleeding from placenta previa is maternal in origin, the fetal heart rate tracing is typically normal. Risk factors include prior cesarean delivery, multiparity, multiple gestation, and tobacco use.
Placenta previa is typically diagnosed at the 18- to 20-week prenatal anatomy ultrasound, when the placental location is determined. Patients with vaginal bleeding at >20 weeks gestation and no previous anatomy ultrasound require a transvaginal ultrasound to exclude placenta previa. Transvaginal ultrasound and speculum examination are safe in placenta previa as neither the transvaginal probe nor the speculum enters the endocervical canal. However, a digital cervical examination is contraindicated due to entrance into the endocervical canal, which can disturb the placenta and result in hemorrhage (Choice B). Placenta previa is an absolute contraindication to vaginal delivery; patients require cesarean delivery.
Subchorionic hematoma
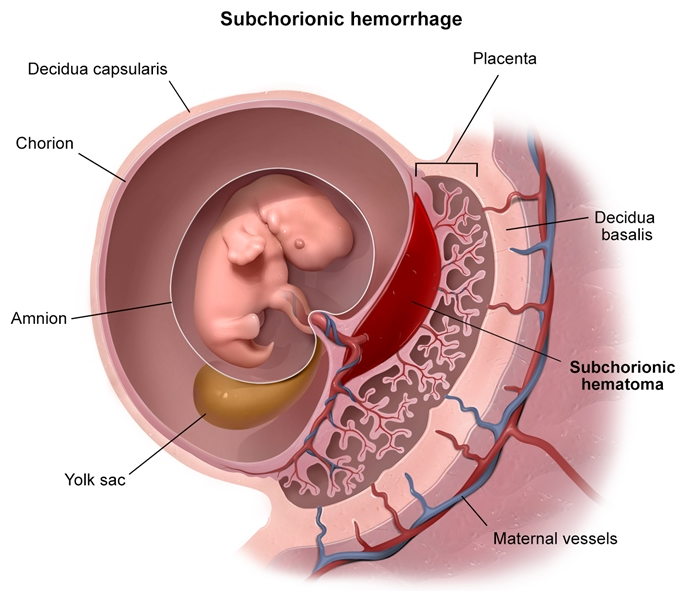
This patient has a subchorionic hematoma, an abnormal collection of blood between the gestational sac and the uterine wall. Subchorionic hematomas are caused by a partial separation of the chorion (outer amniotic membrane) from the uterine wall. Risk factors include the use of anticoagulants, infertility treatment, uterine malformation (eg uterine septum, leiomyoma), and a history of recurrent pregnancy loss. Although subchorionic hematomas can present with vaginal bleeding, they also can be an incidental finding during routine ultrasound. Subchorionic hematomas typically appear on ultrasound as crescent, hypoechoic lesions adjacent to the gestational sac. The majority of patients with subchorionic hematomas have uncomplicated pregnancies, and management is expectant; patients can be followed with serial ultrasounds to help provide reassurance.
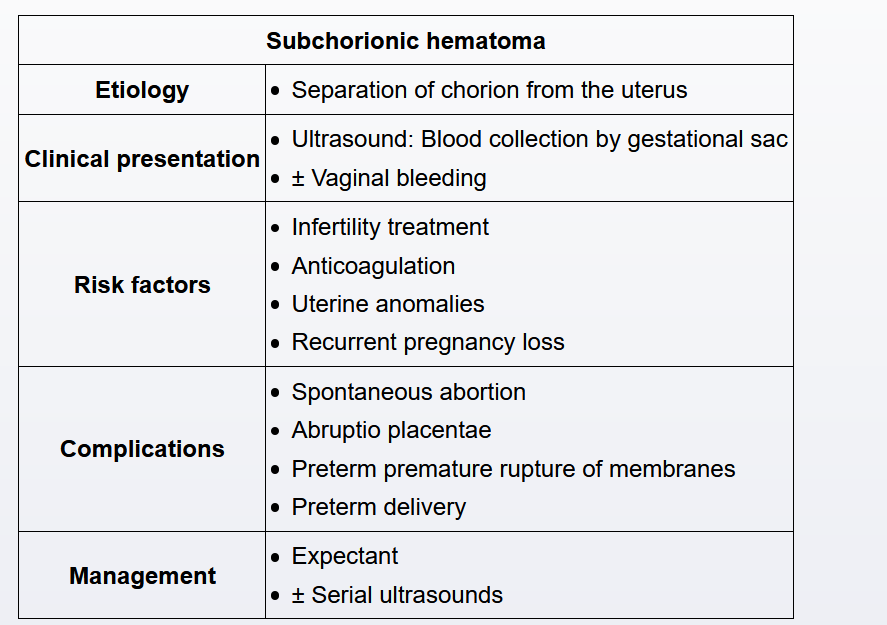
Subchorionic hematomas can result in placental dysfunction, particularly when the blood collection is located centrally on the placenta. Therefore, patients with subchorionic hematomas are at increased risk of spontaneous abortion, pregnancy loss (miscarriage) at <20 weeks gestation. In addition, during the third trimester, patients with subchorionic hematomas are at increased risk for abruptio placentae, preterm premature rupture of membranes, preterm labor, preeclampsia, fetal growth restriction, and intrauterine fetal demise. However, the majority of patients with subchorionic hematomas have uncomplicated pregnancies.
Pre eclampsia
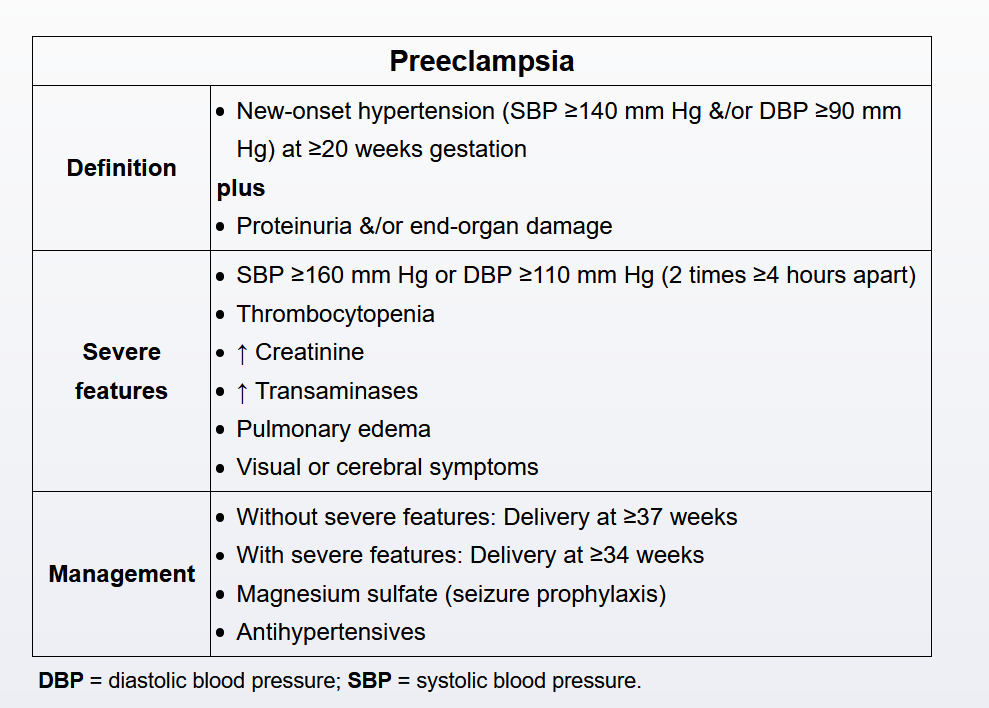
At 37 weeks gestation, this patient has a blood pressure of >160/110 mm Hg, proteinuria, and signs of end-organ damage (eg, headache, visual symptoms), a presentation consistent with preeclampsia with severe features. Severe elevations in blood pressure increase the risk of seizure, stroke, hepatorenal failure, and abruptio placentae.
This patient has preeclampsia based on a new onset of hypertension, pulmonary edema, and hyperreflexia (ie, end-organ damage). Although preeclampsia typically occurs during pregnancy, it can also occur up to 12 weeks postpartum. Preeclampsia is associated with vascular endothelial injury that leads to increased vascular permeability and a decrease in capillary colloid pressure. It is also associated with arterial vasospasm that increases capillary hydrostatic pressure. The result is third-spacing of fluid into surrounding tissues that causes peripheral edema, cerebral edema (eg, headaches, visual changes), and pulmonary edema. Pulmonary edema (eg, dyspnea, hypoxemia, decreased breath sounds) as a complication of preeclampsia is more common in the postpartum period.
Treatment of postpartum preeclampsia includes seizure prophylaxis with magnesium sulfate and blood pressure control. Patients with associated pulmonary edema and fluid overload may require fluid restriction, oxygen support, and diuretics.