AKI in transplant patients
- related: Nephrology
- tags: #nephrology
This patient has acute kidney injury and electrolyte abnormalities while on tacrolimus and fluconazole; this should raise suspicion for calcineurin inhibitor nephrotoxicity. Calcineurin inhibitors (eg, tacrolimus, cyclosporine) are common immunosuppressants used in organ transplantation; toxicity may be due to medication-induced vasoconstriction leading to renal ischemia.
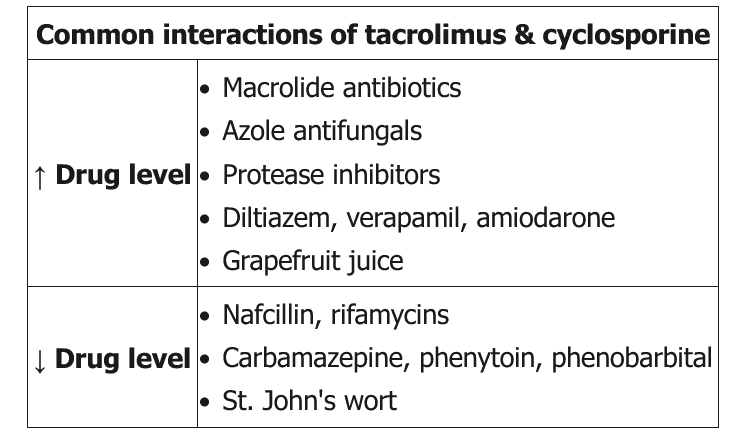
Patients can have declining glomerular filtration rates and a variety of metabolic abnormalities, including hyperkalemia, hyperuricemia, hypophosphatemia, hypomagnesemia, hypercalciuria, and possibly metabolic acidosis. Significant hypertension may also be present. Toxicity is dose-dependent. Calcineurin inhibitors are metabolized by cytochrome P450 3A4; levels are increased by other drugs that are metabolized by this enzyme (eg, azole antifungals, macrolides, non-dihydropyridine calcium channel blockers).
Biopsy is often required to rule out acute rejection; histologic findings are nonspecific, but calcineurin inhibitor nephrotoxicity is suggested by the absence of signs of acute rejection (eg, interstitial inflammation, intimal arteritis, tubulitis). Acute calcineurin inhibitor toxicity is usually reversible with drug cessation, although some patients develop residual chronic renal dysfunction.
Acute graft rejection most commonly occurs within the first 6 months post-transplant, unless the patient is noncompliant with immunosuppression. In addition, significant proteinuria (>1 g) is often present.