06 Ventilation
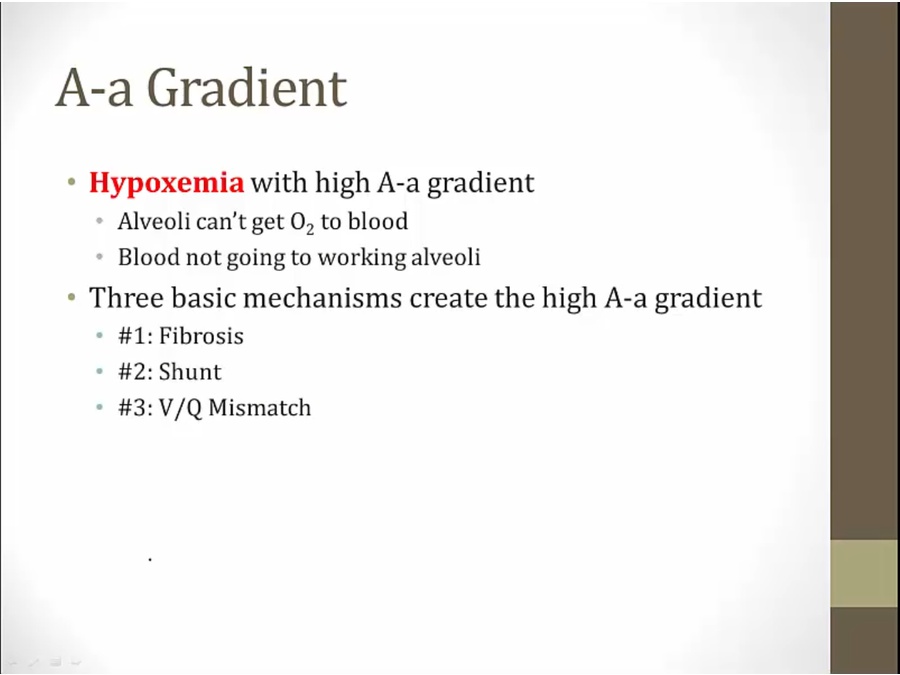
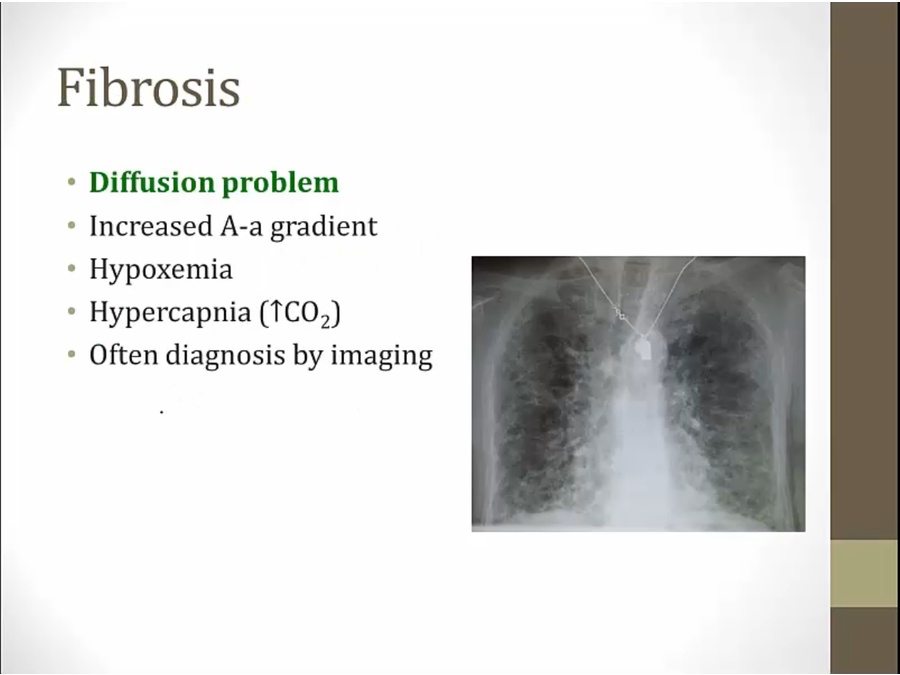
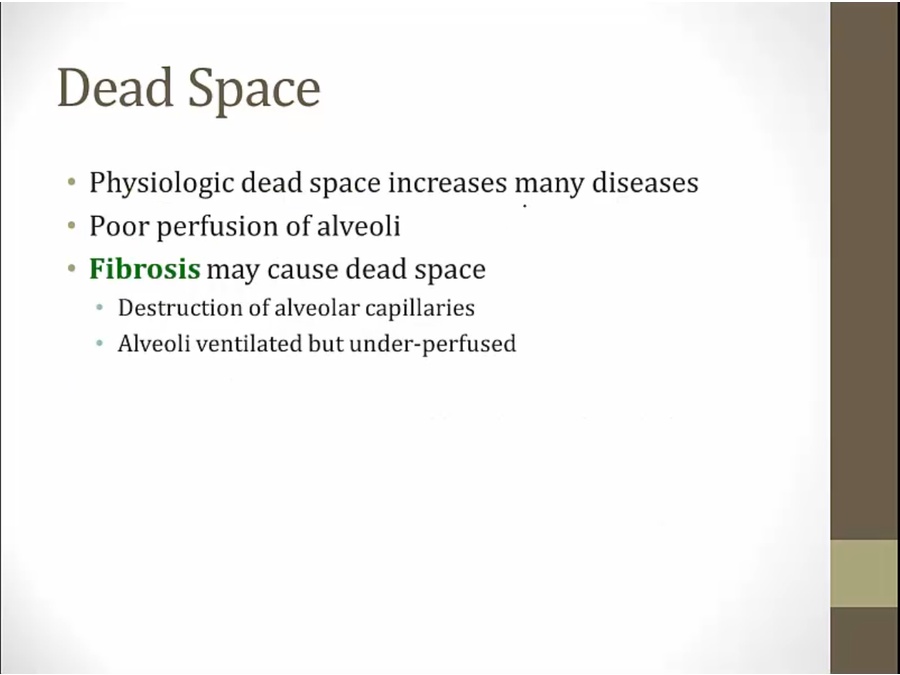
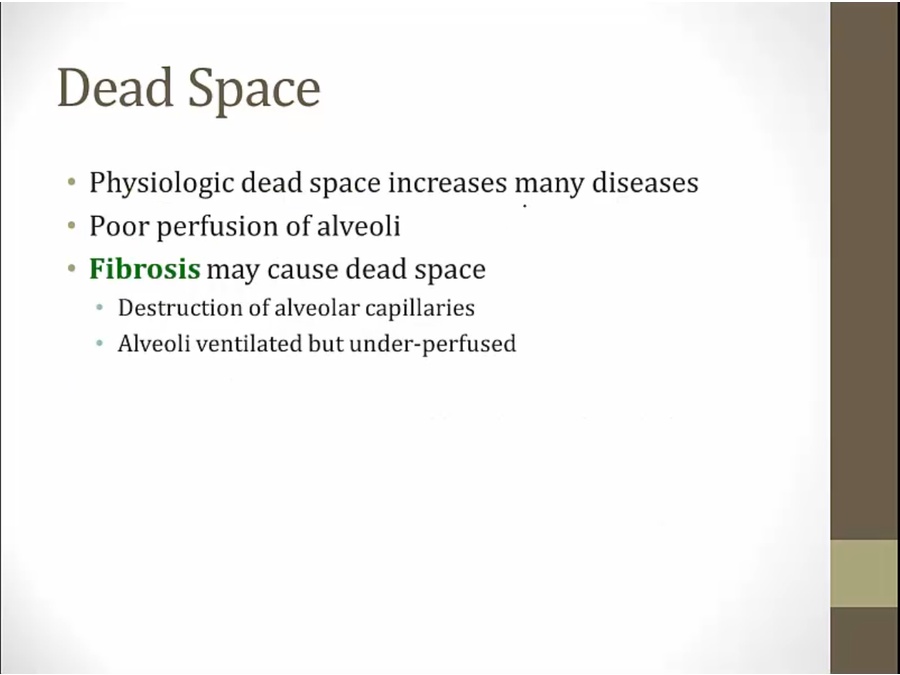
Fibrosis
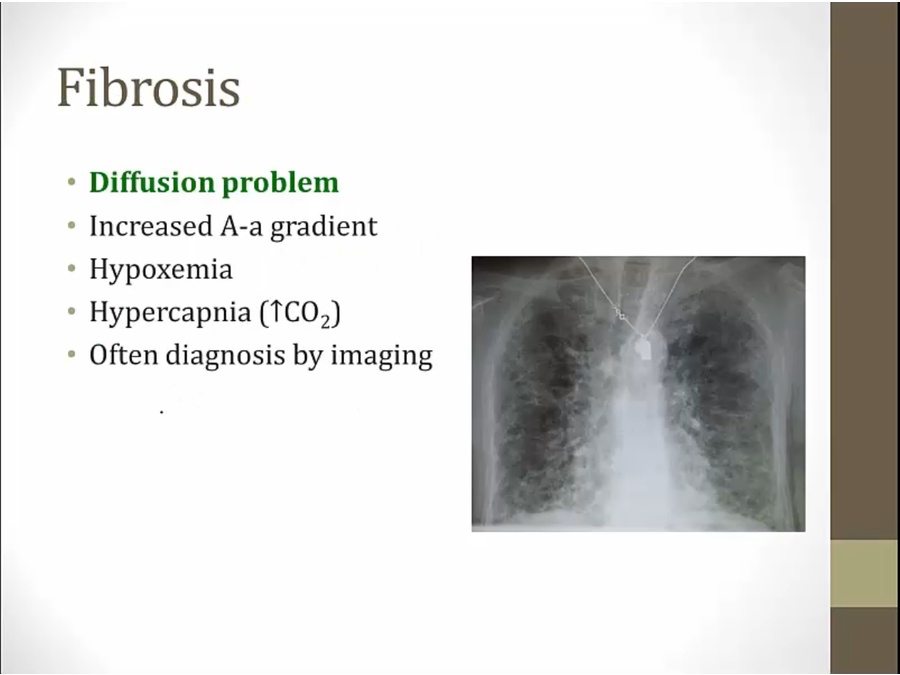
- deposition of fibrous tissues in lungs, destroys alveoli
- barrier created by fibrous tissue
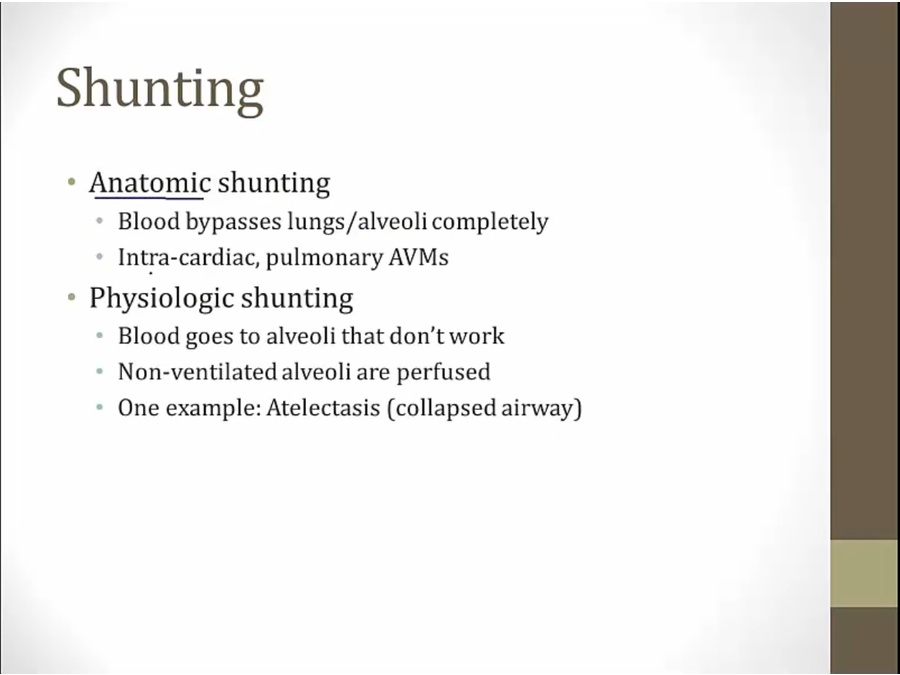
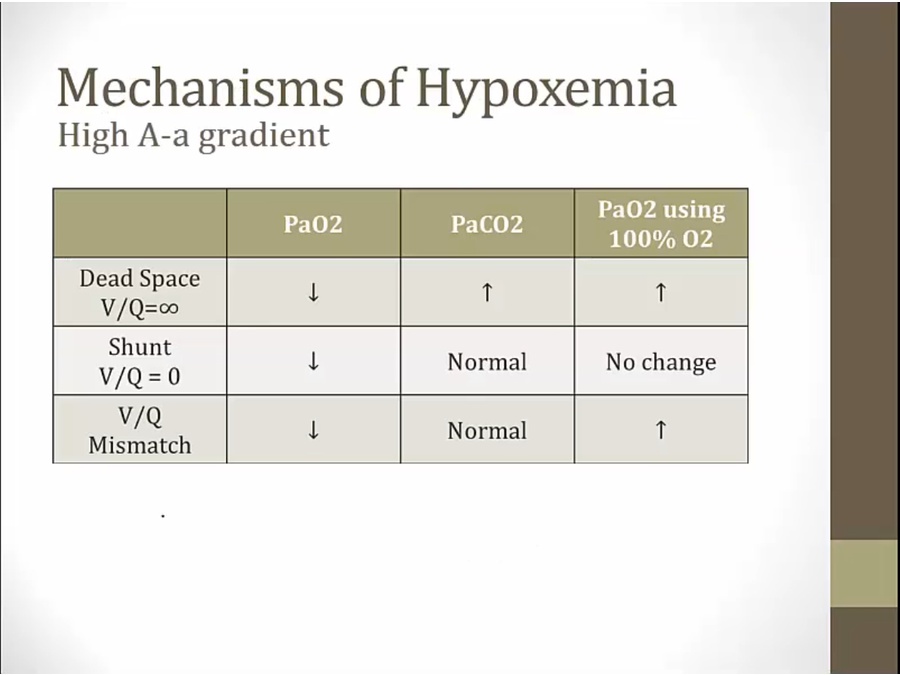
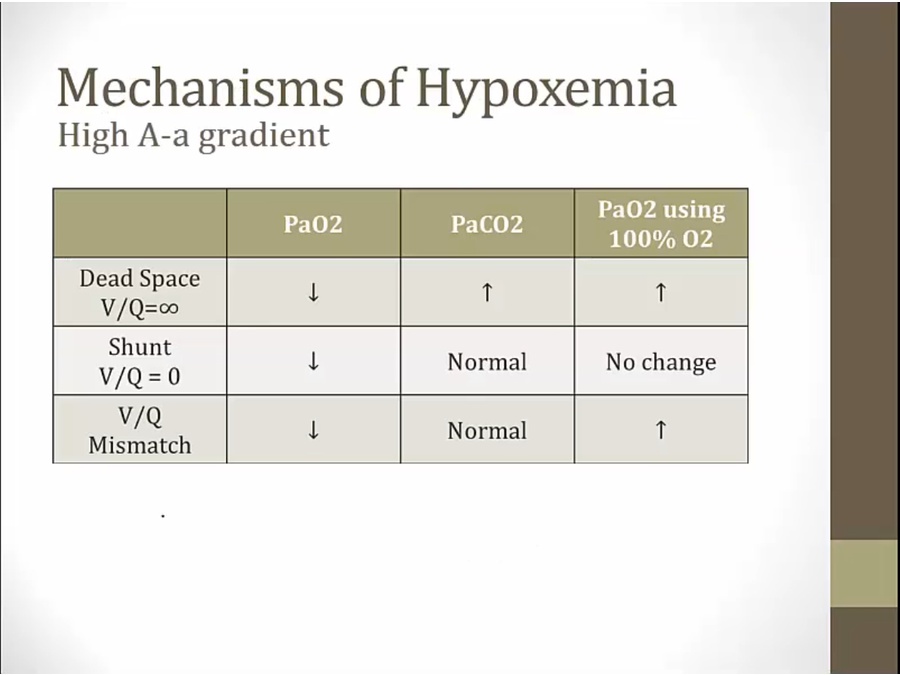
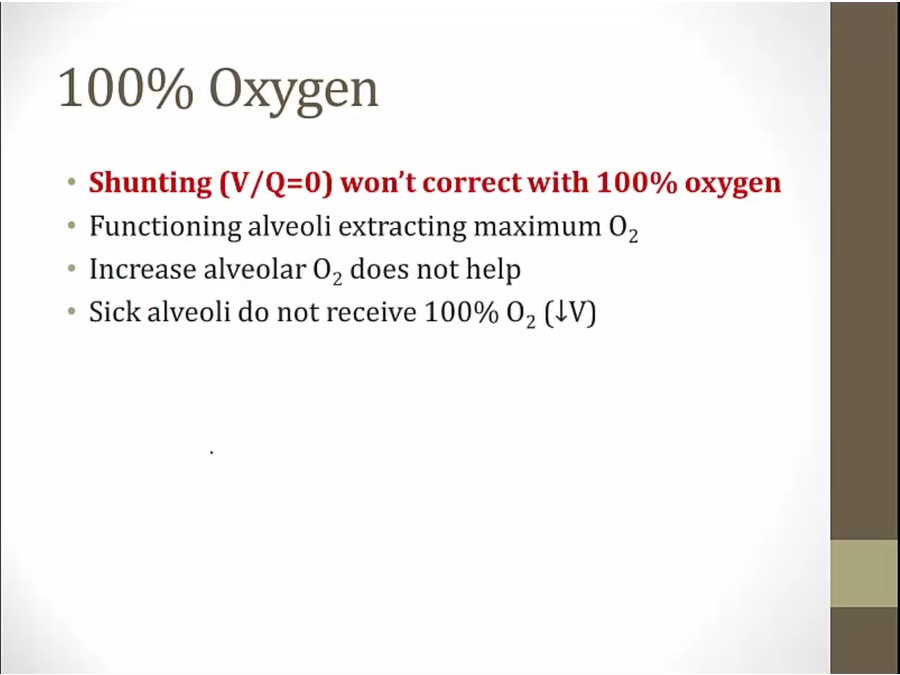
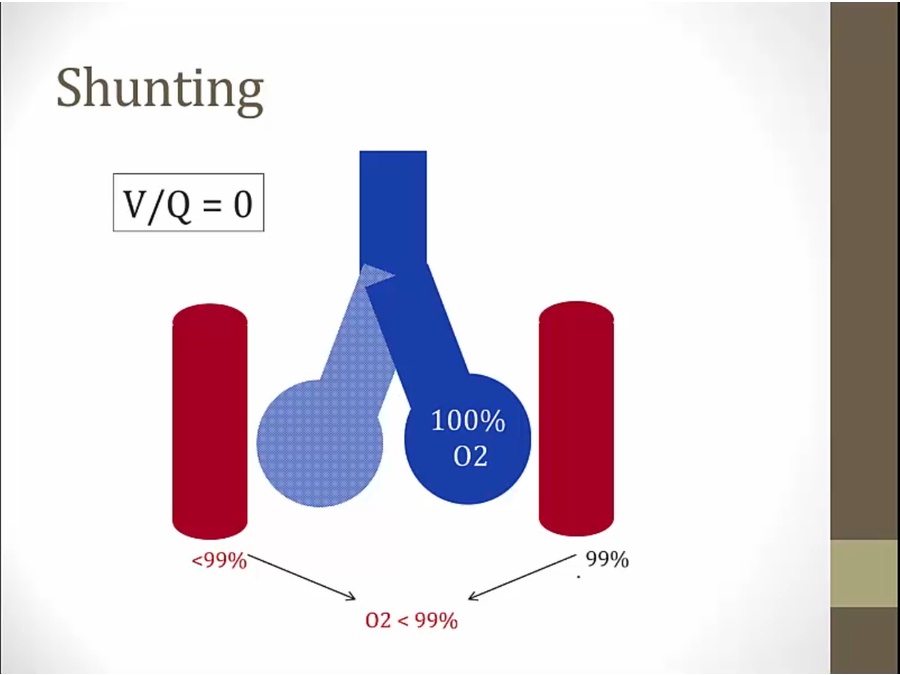
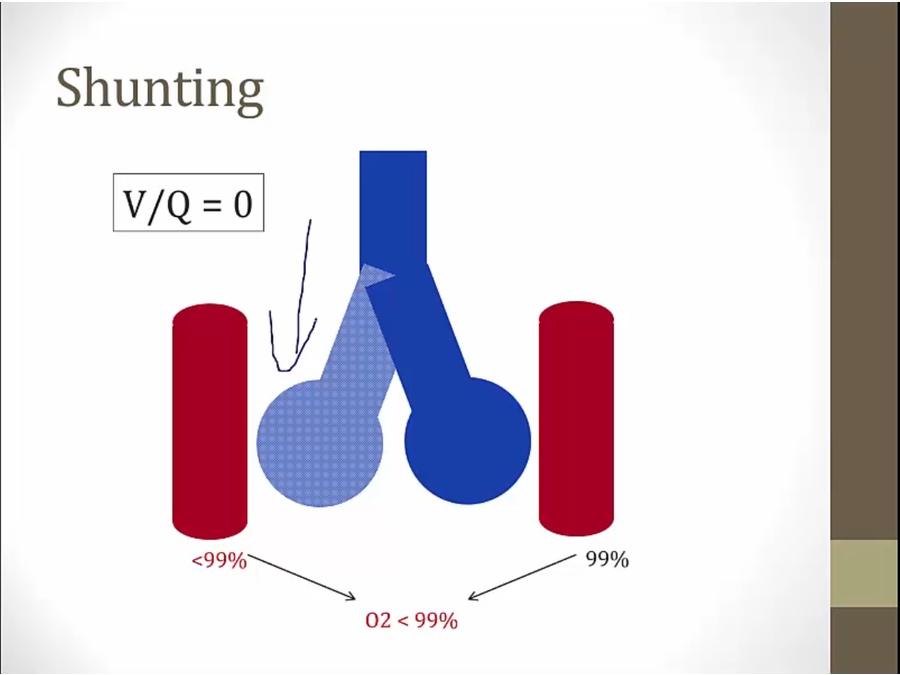
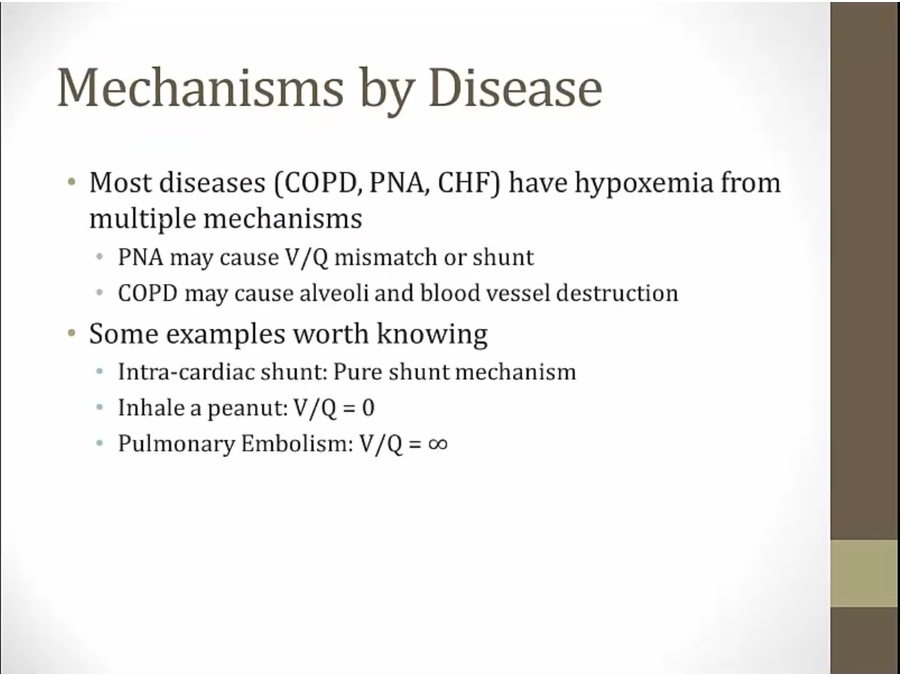
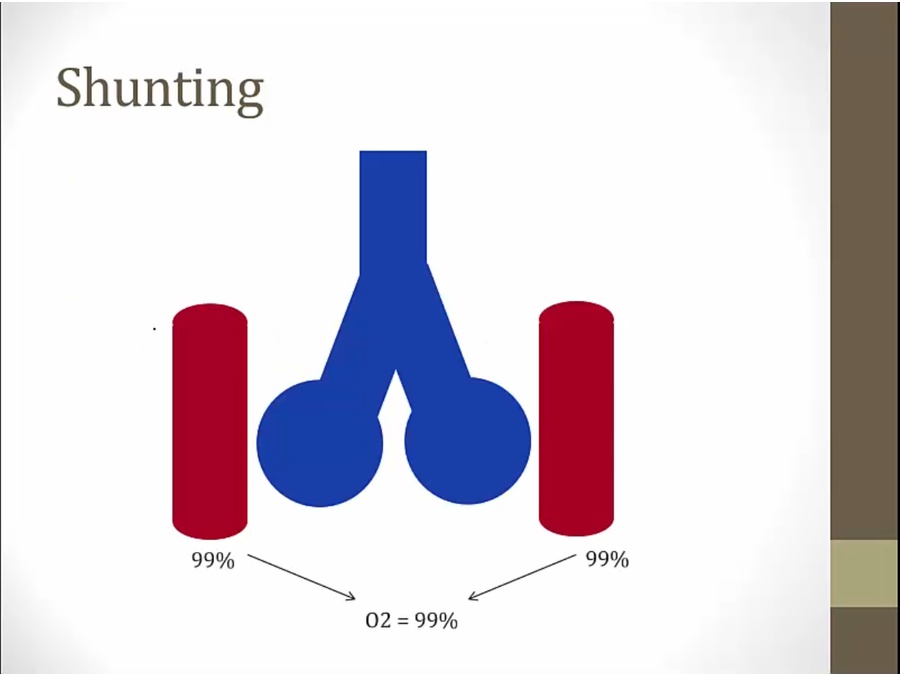
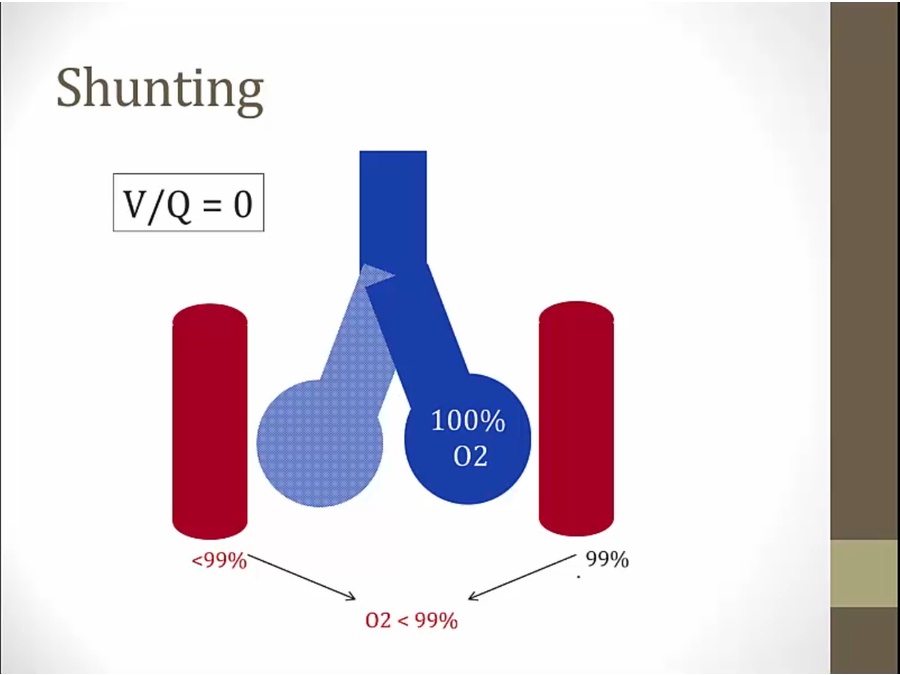
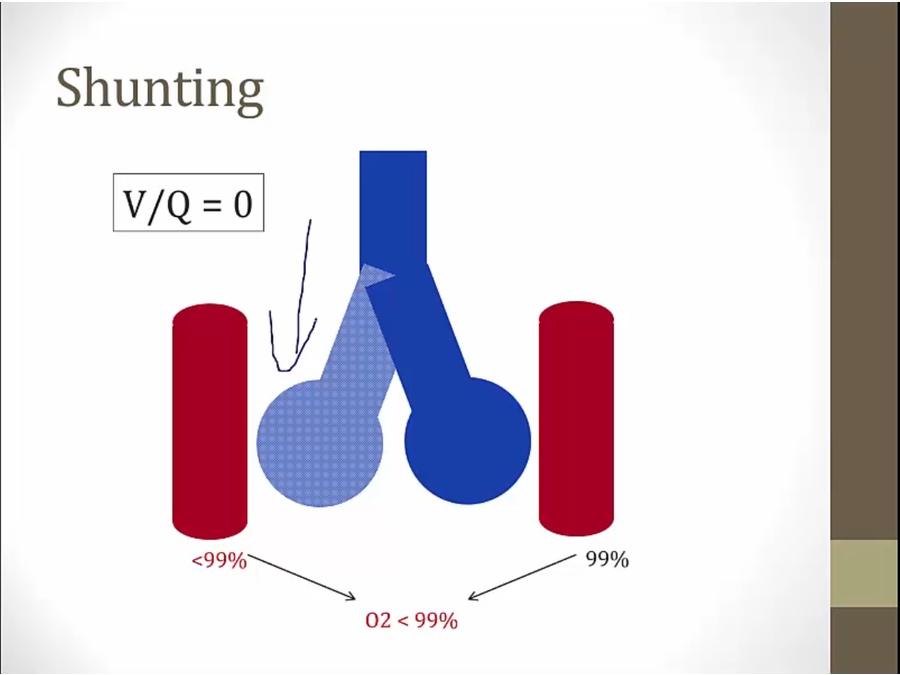
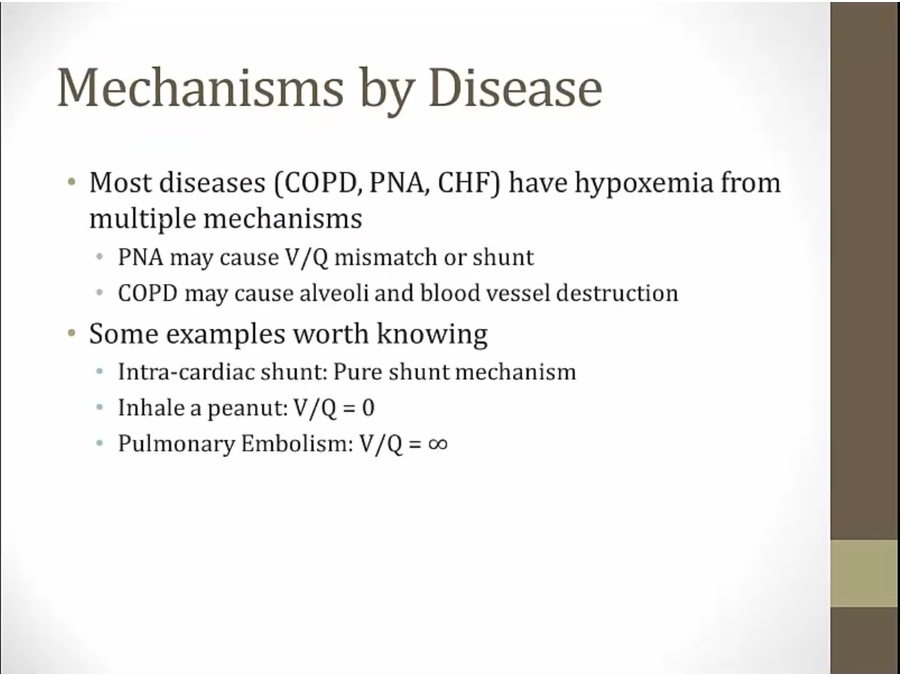
Shunt
V/Q < 1
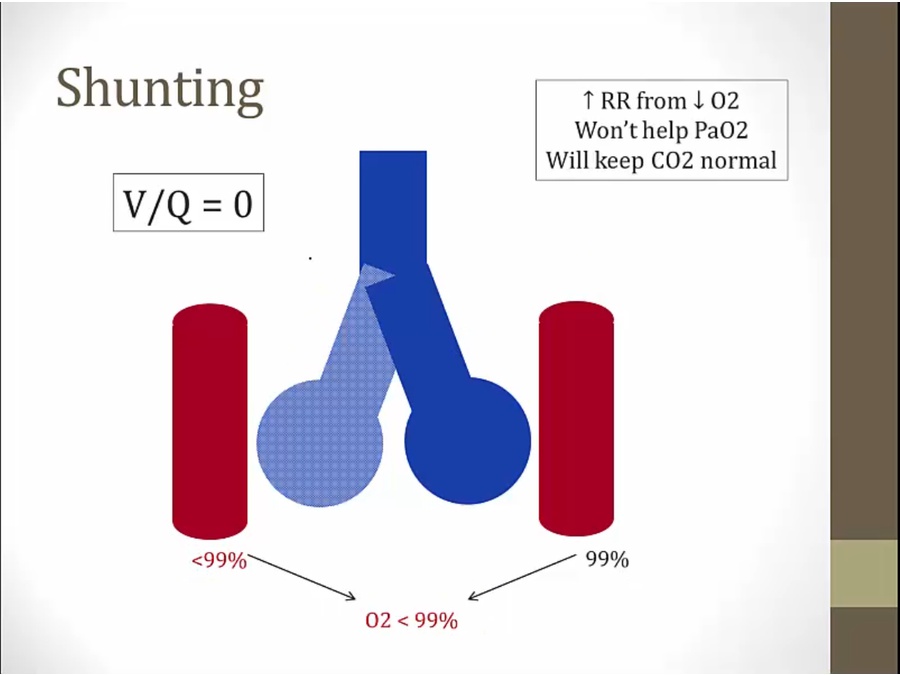
- so extreme V/Q = 0
- shunting as if blood bypassed lung
- anatomic: large congenital defect (VSD)
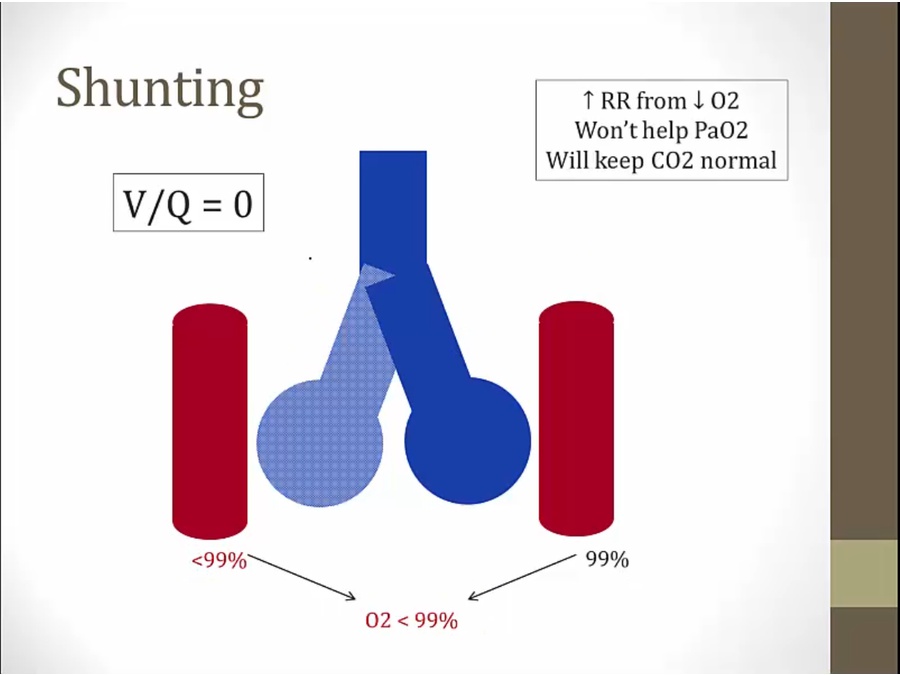
- left alveoli with V/Q of 0
- result hypoxemia when blood mixed
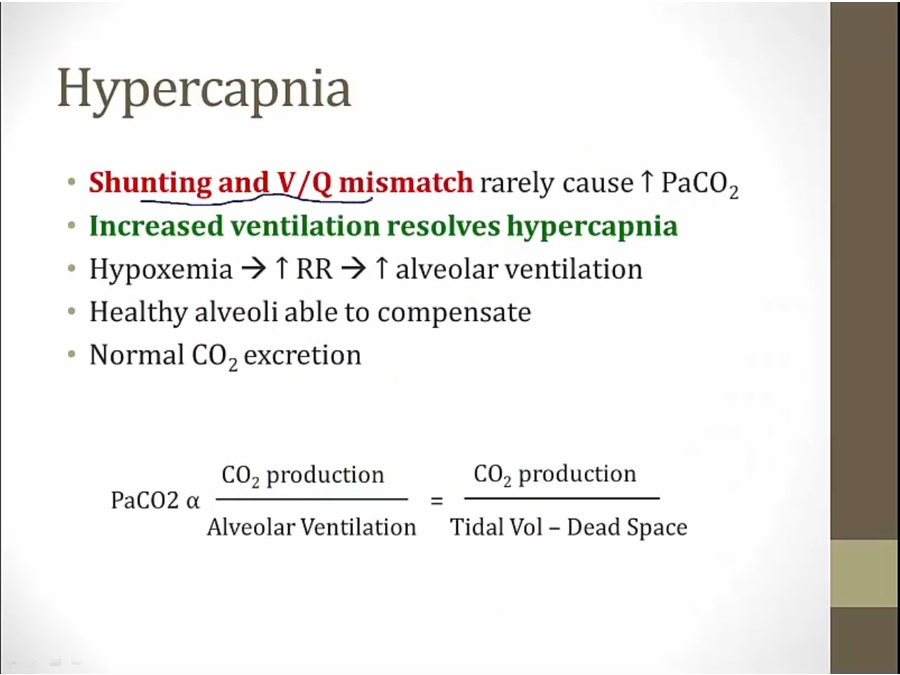
- hyperventilation cannot increase PaO2: blood only goes through healthy alveoli, still mixing at end. Only way to resolve is to resolve shunting (take out mucous plug)
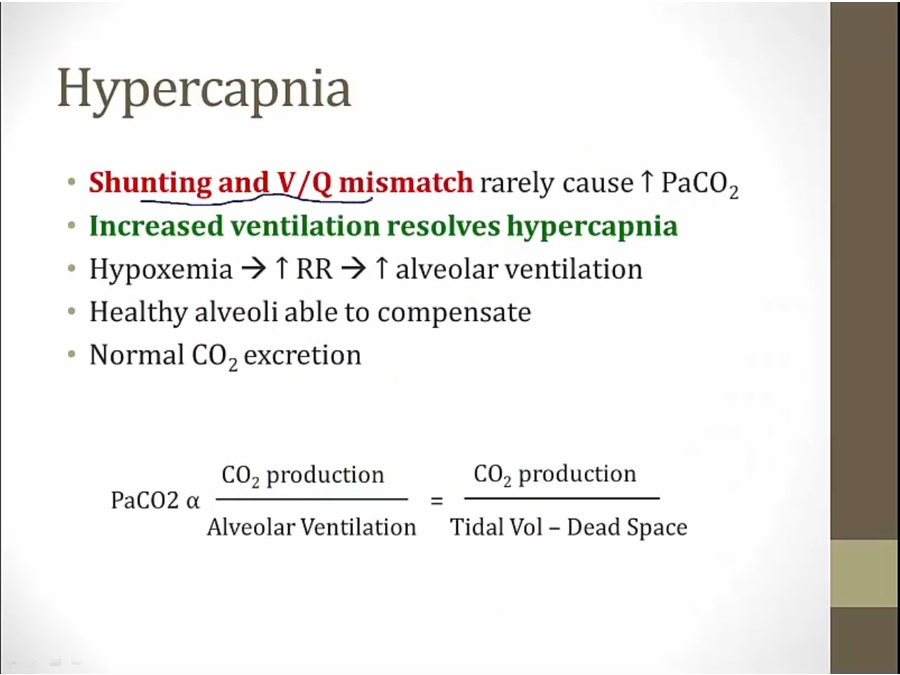
- no hypercapnea: more CO2 is pulled with hyperventilation
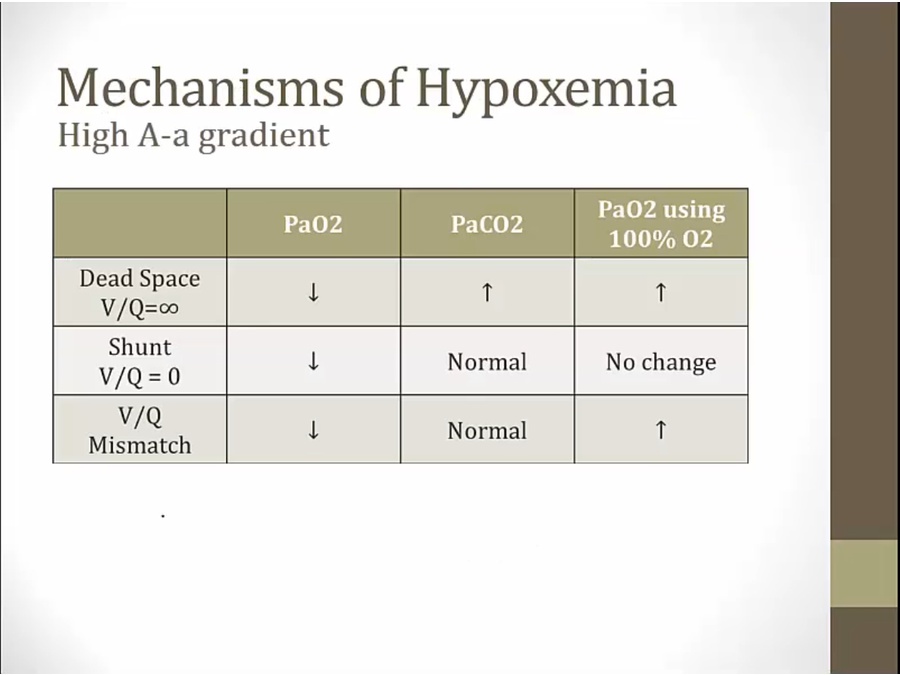
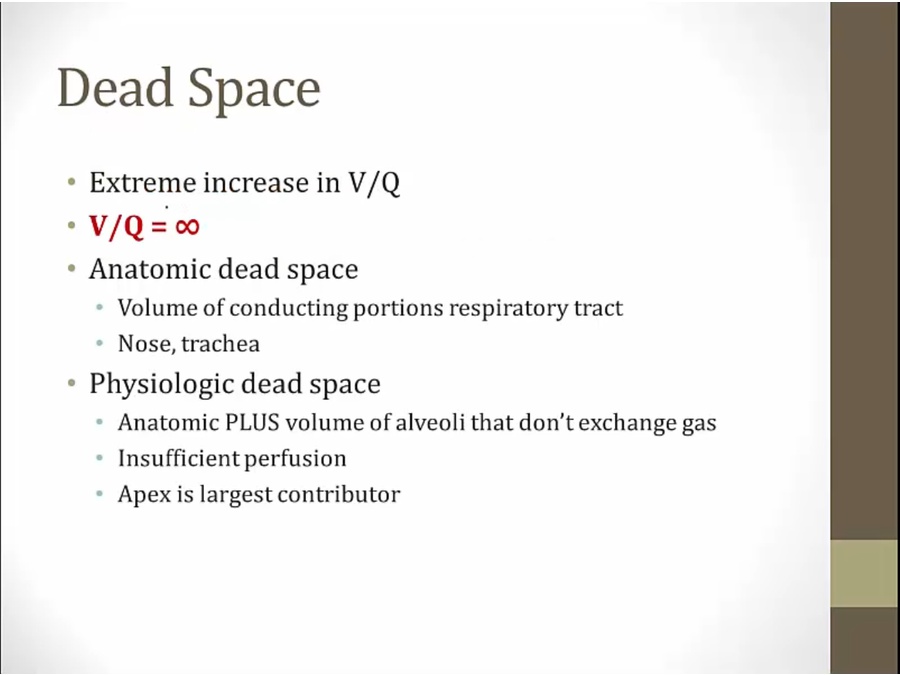
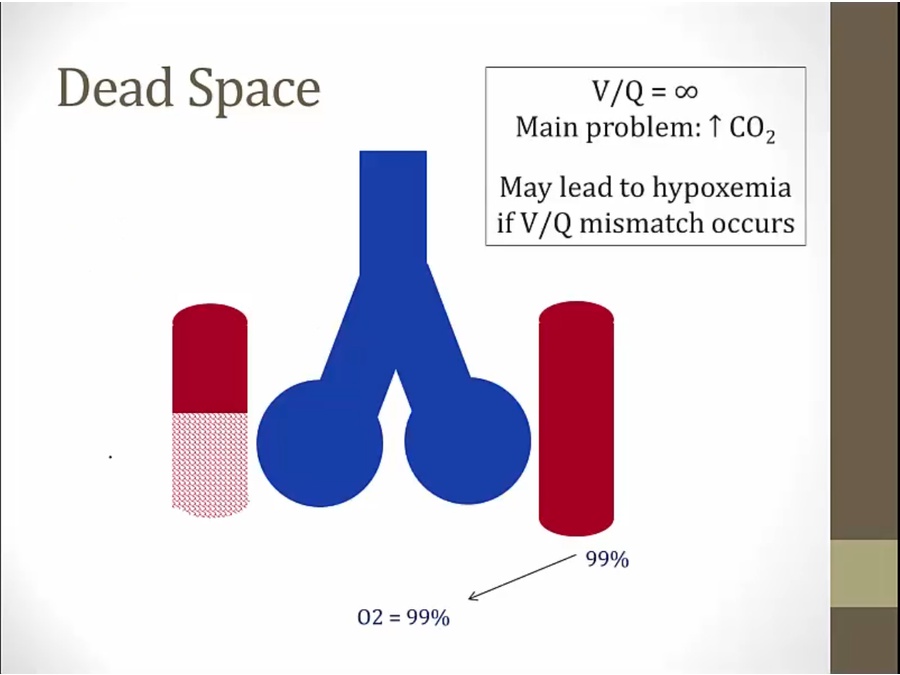
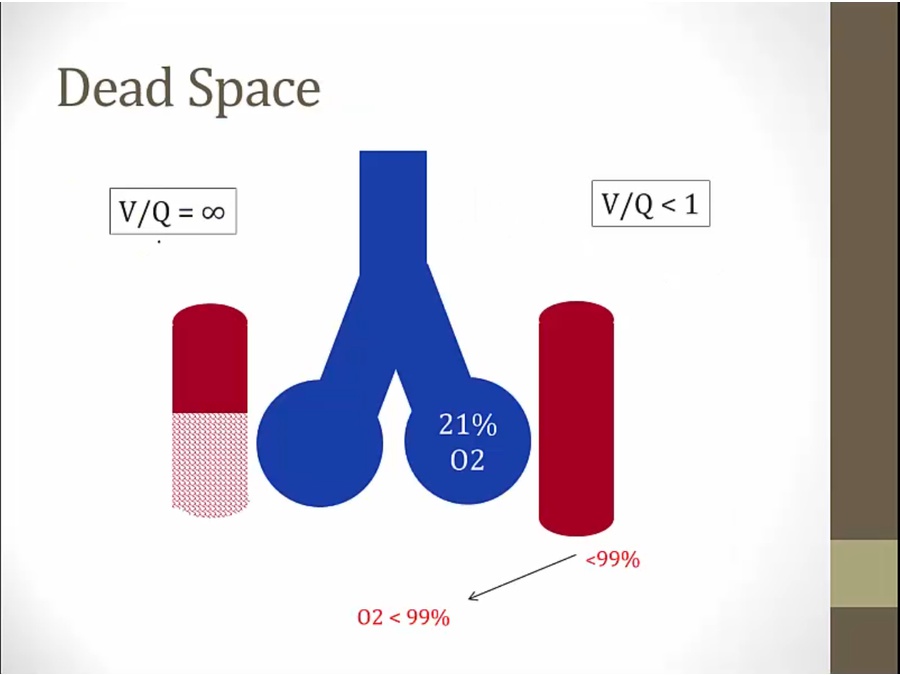
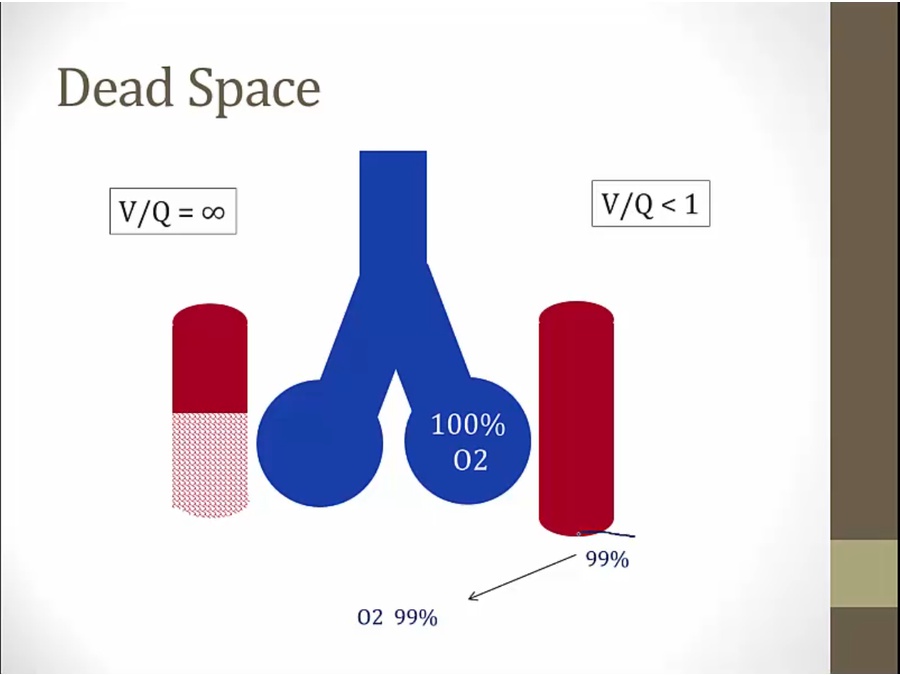
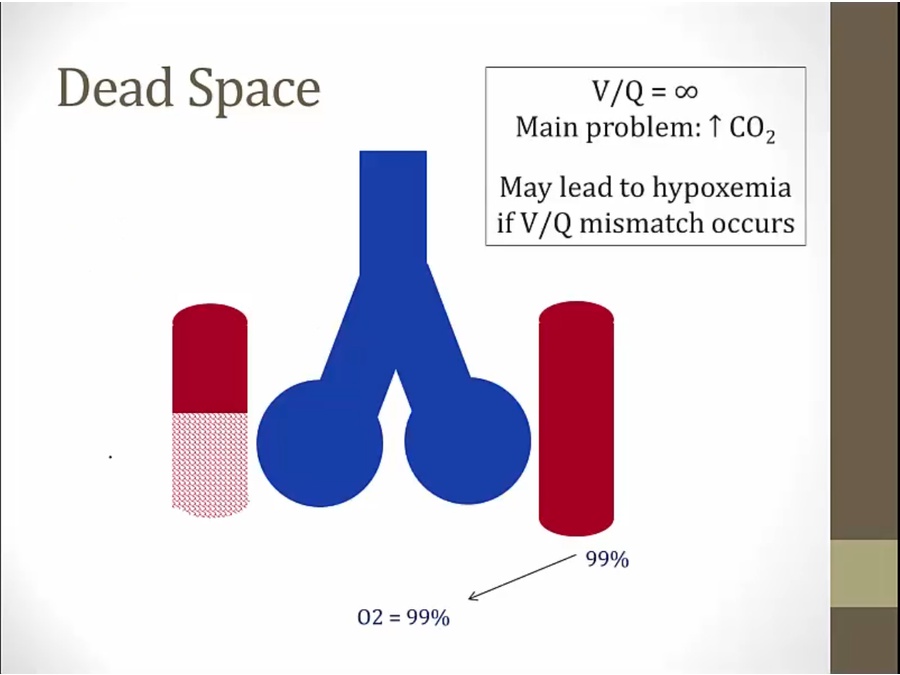
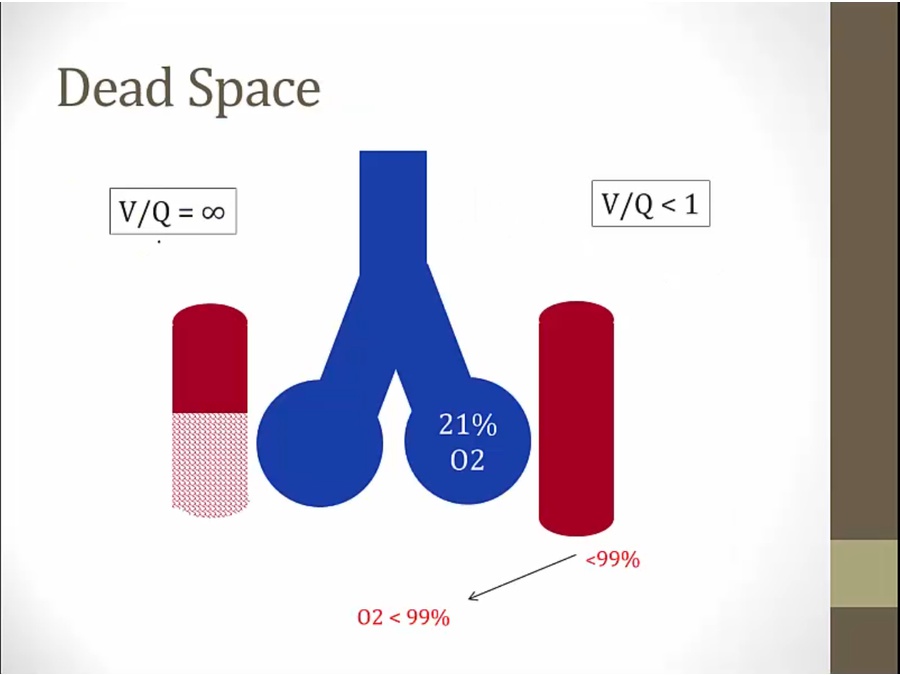
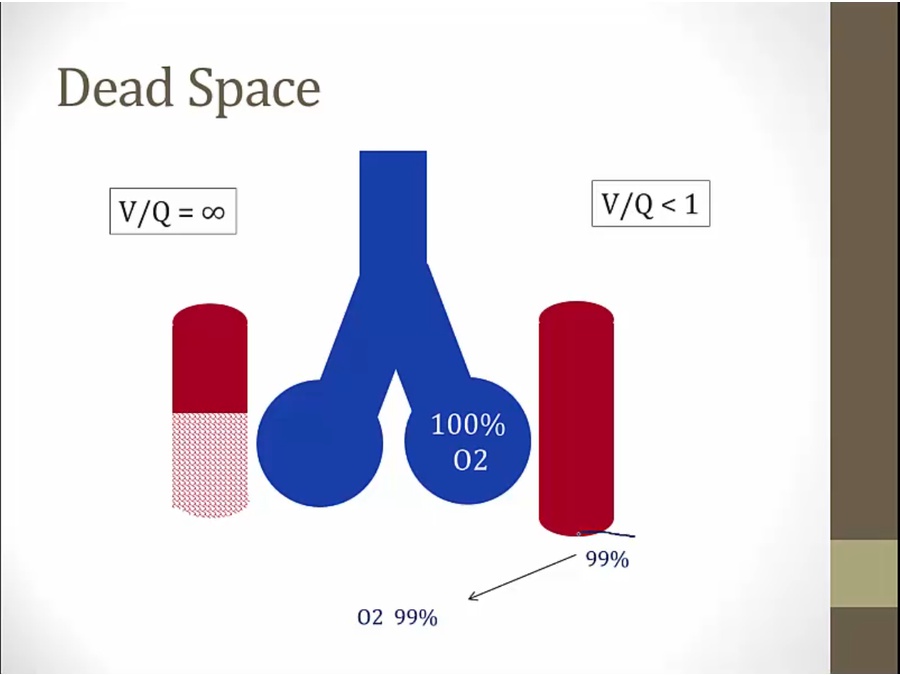
V/Q > 1
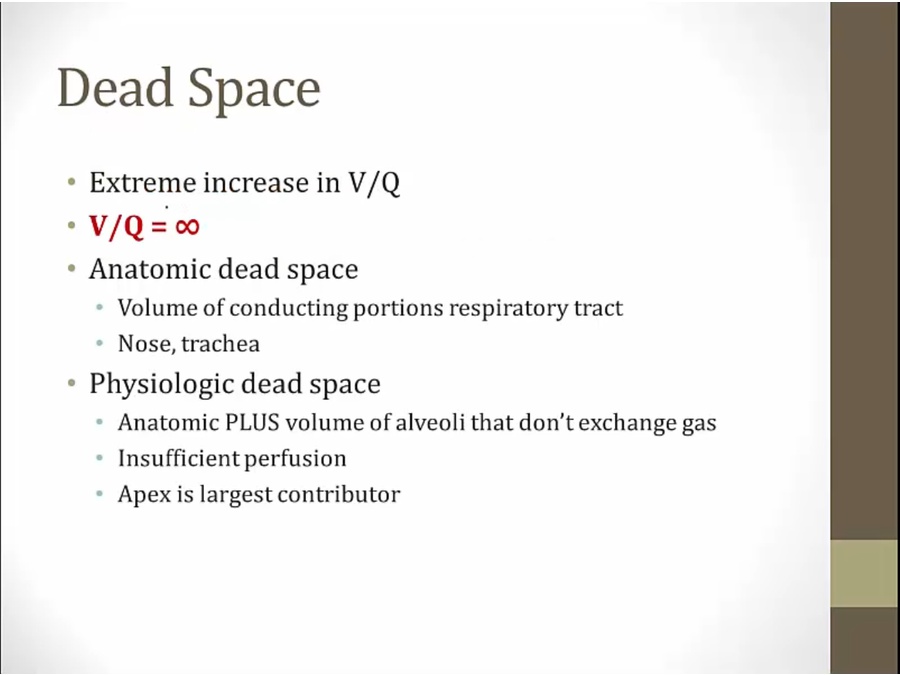
- PE clotting blood
- O2 in arterial will be normal, no hypoxemia if pure dead space
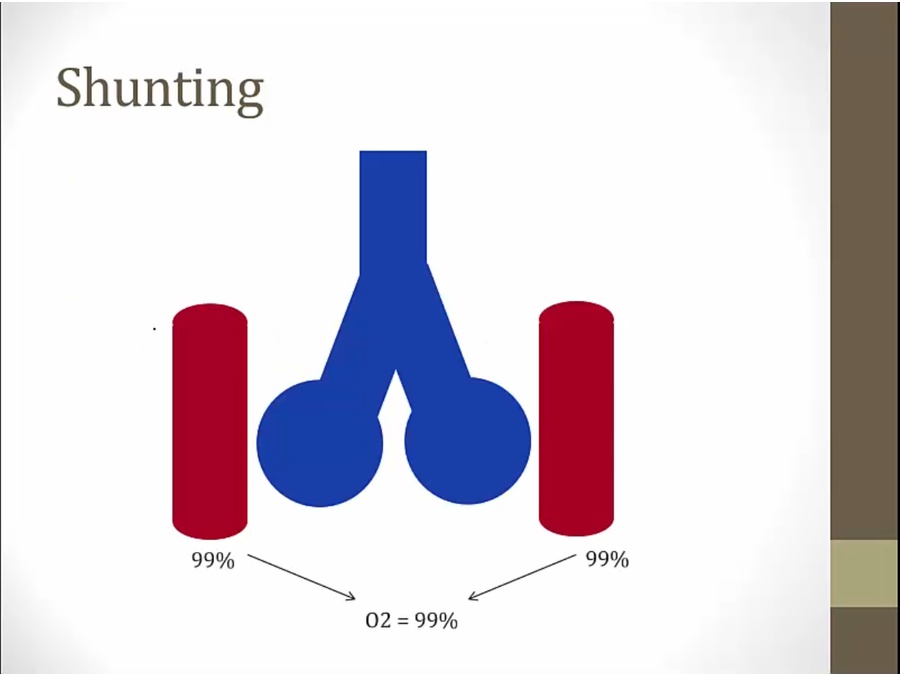
- No blood to left, more blood to right: reduced V/Q, less than 99% O2 sat coming out (V/Q mistmach)
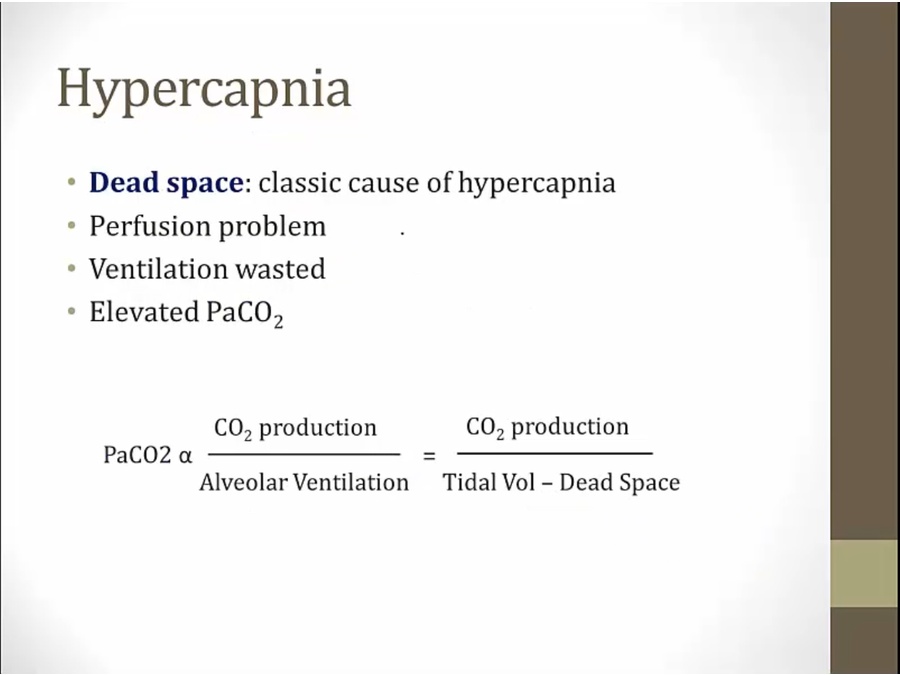
- CO2 up: ventilation wasted because CO2 not exchanged
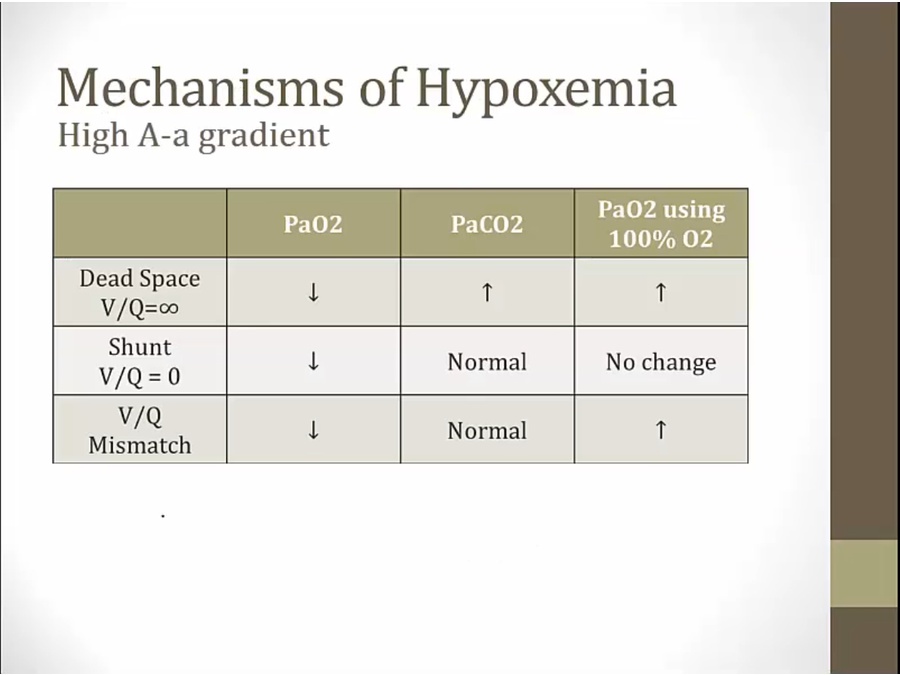
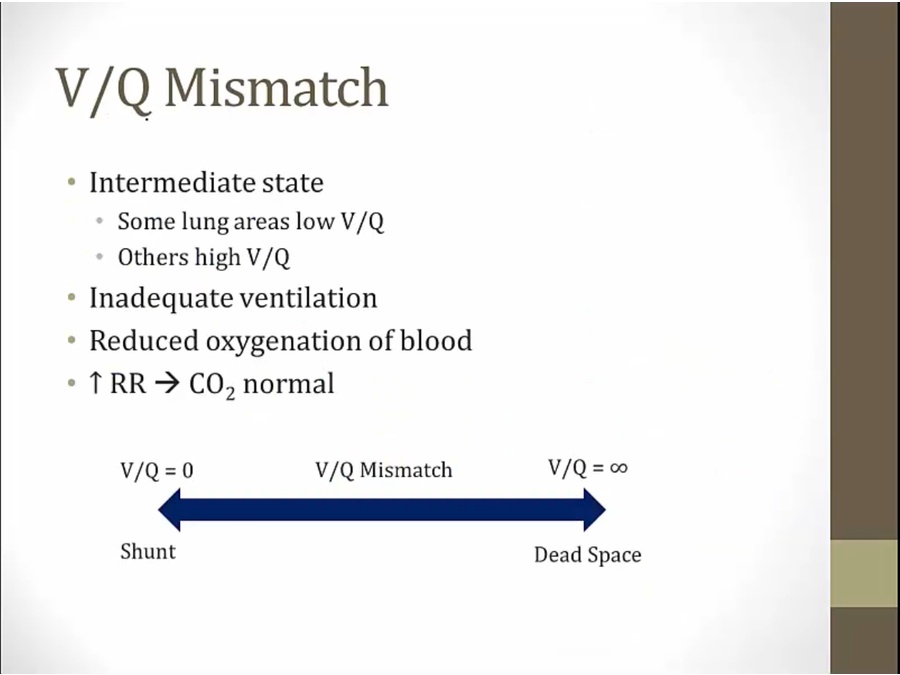
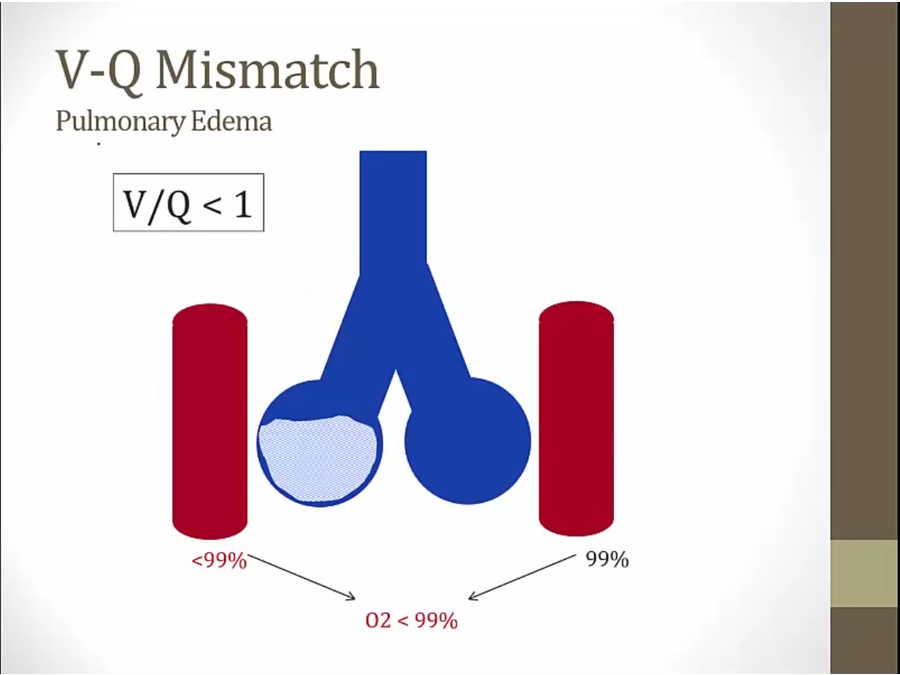
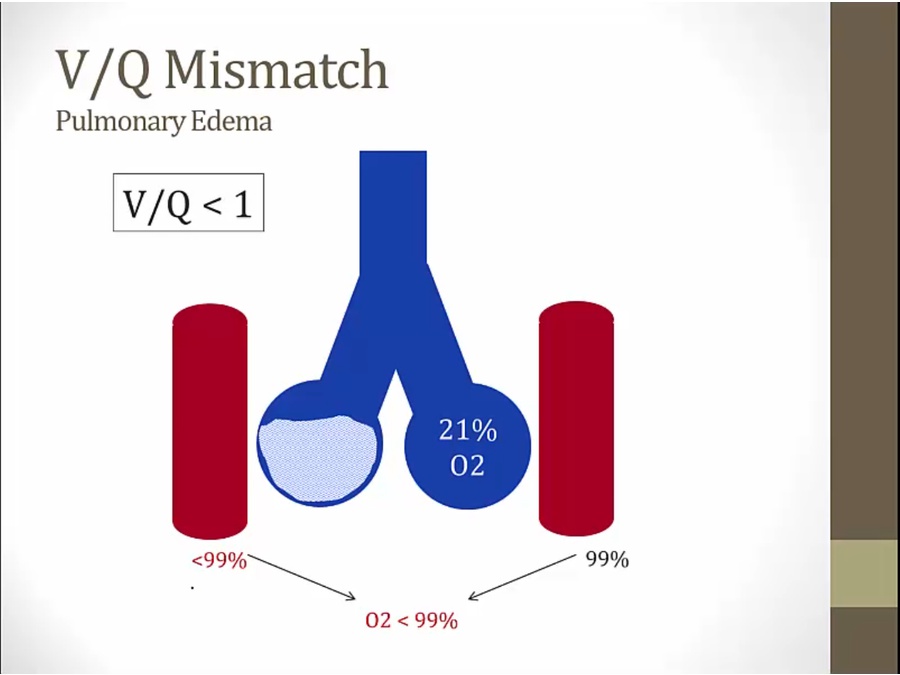
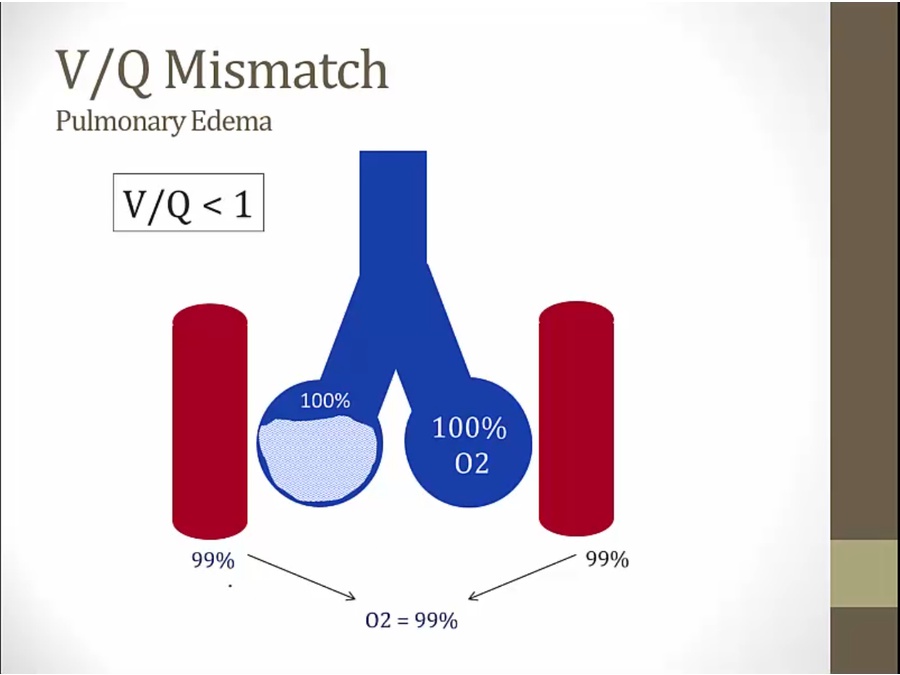
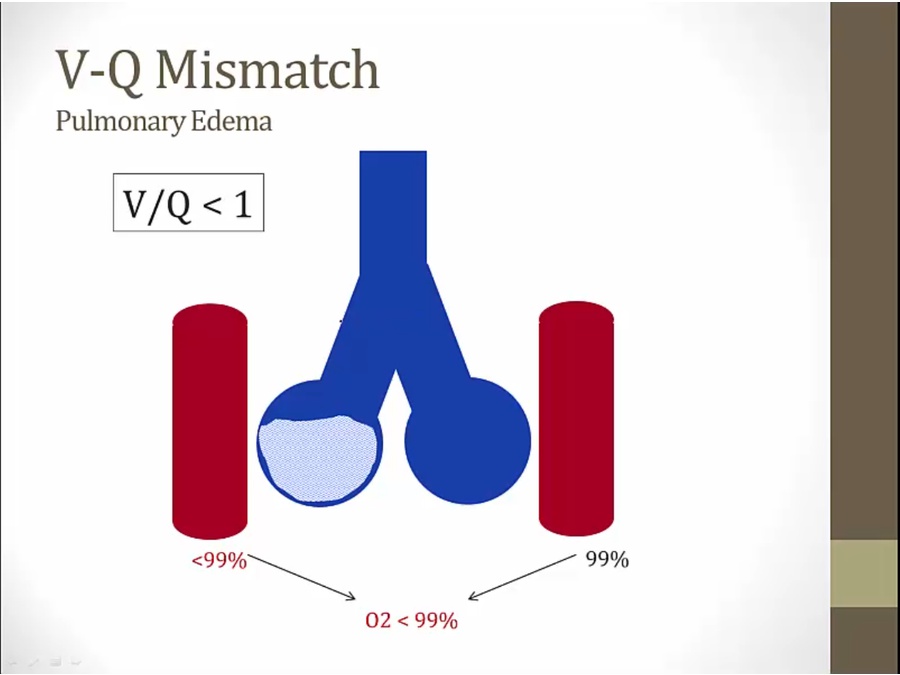
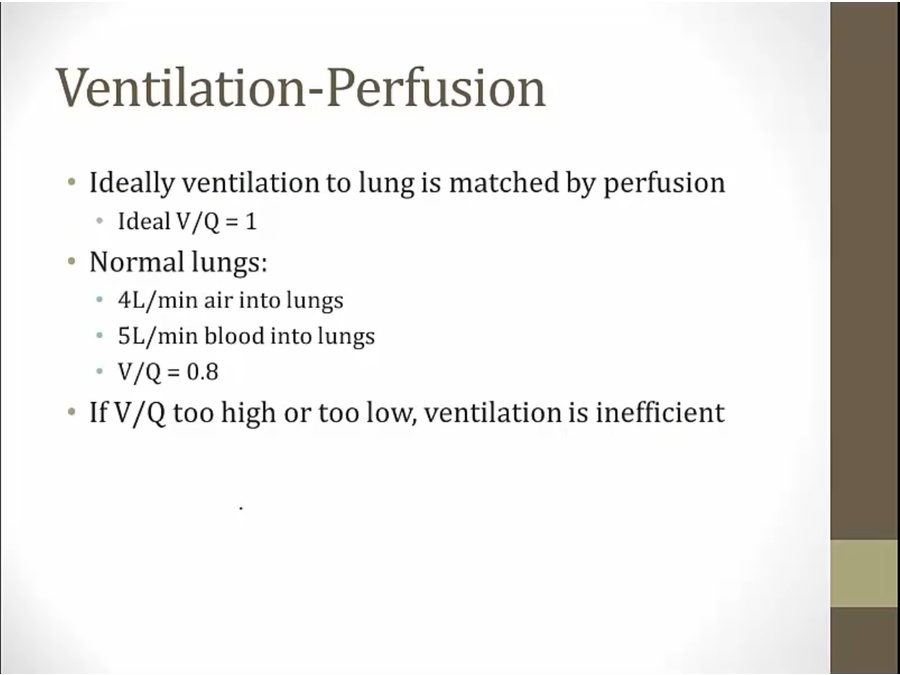
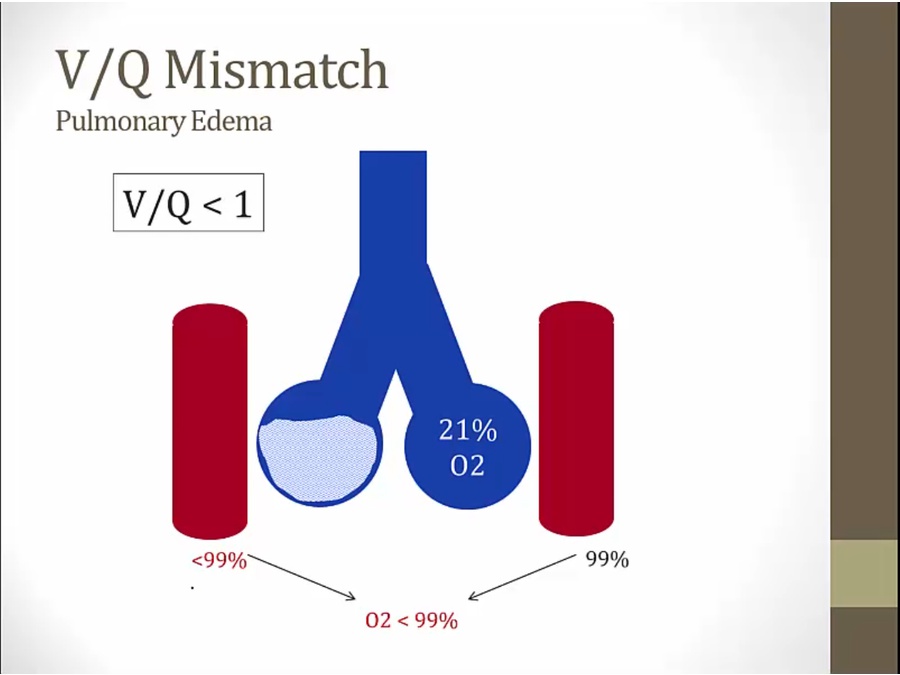
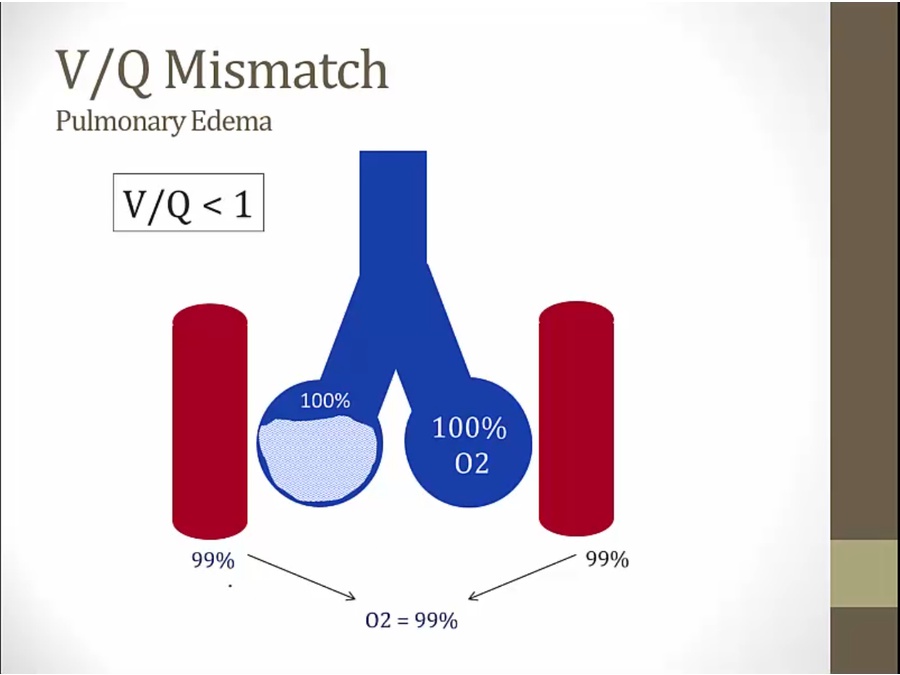
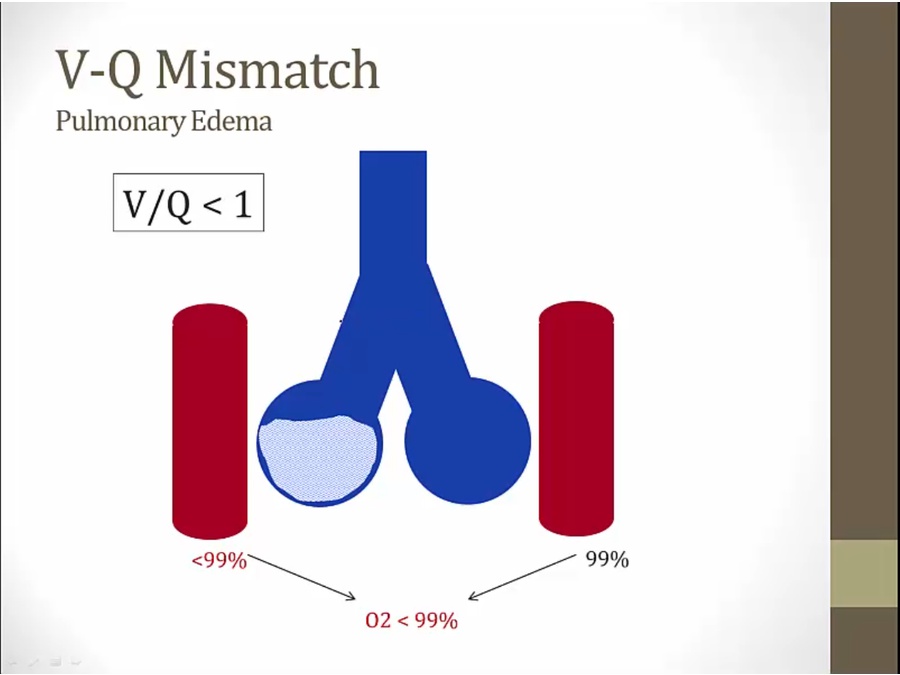
V/Q Mismatch
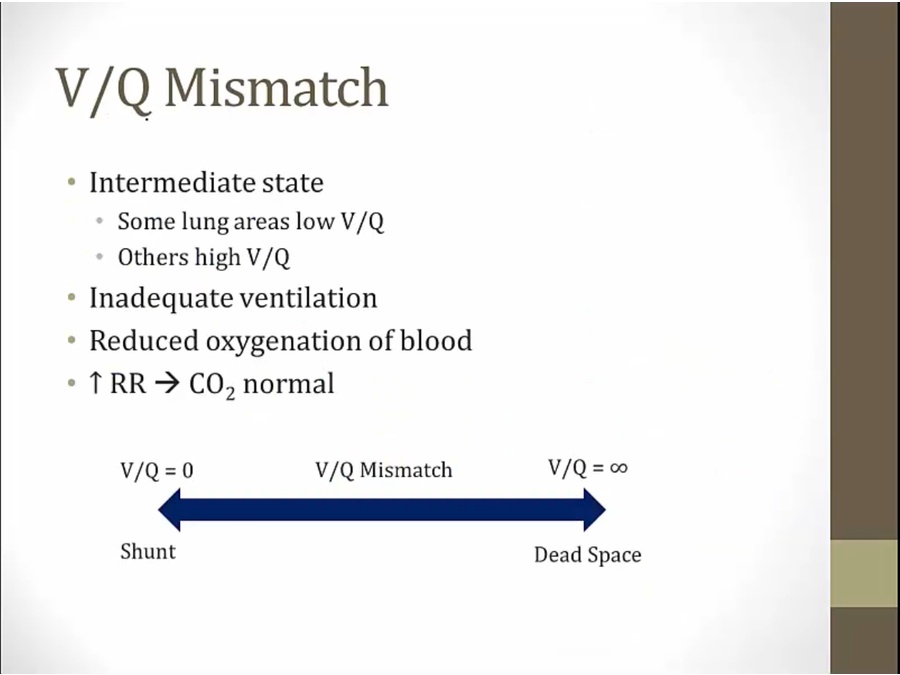
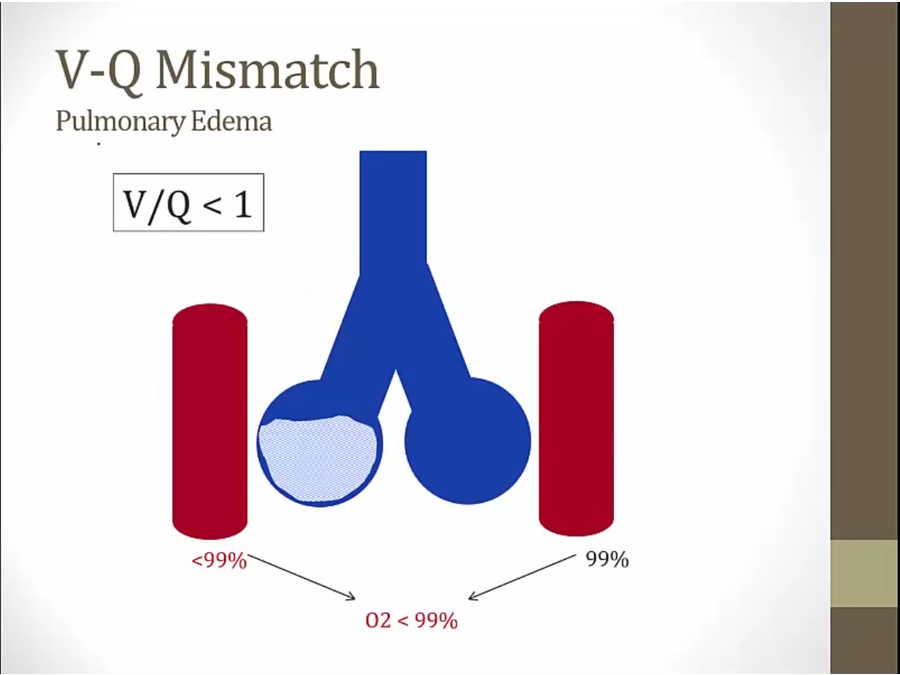
- water resulting in less ventilation V/Q < 1
- distinct from shunt/dead space
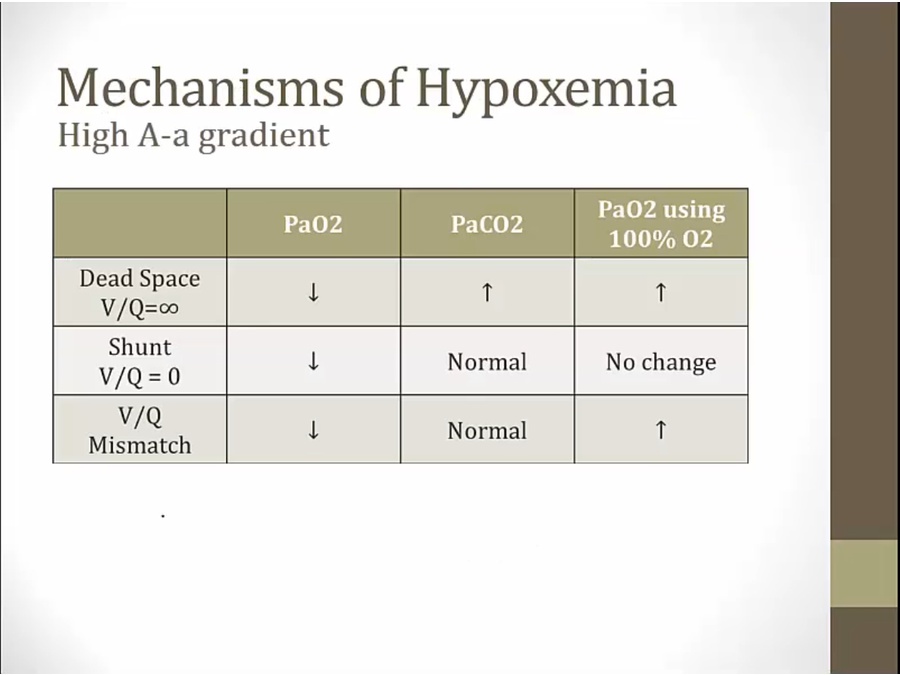
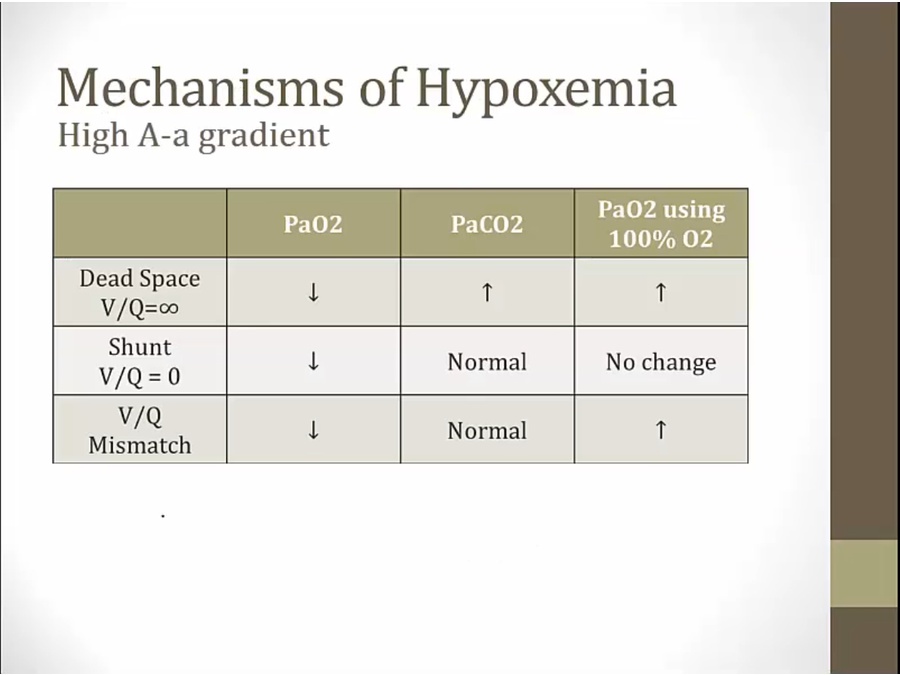
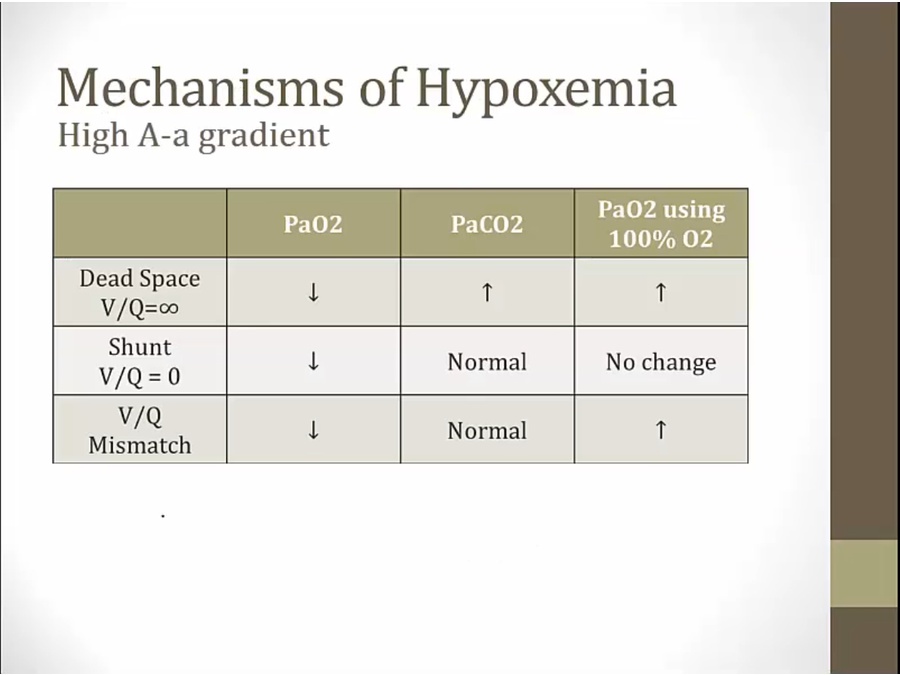
Diagnosis
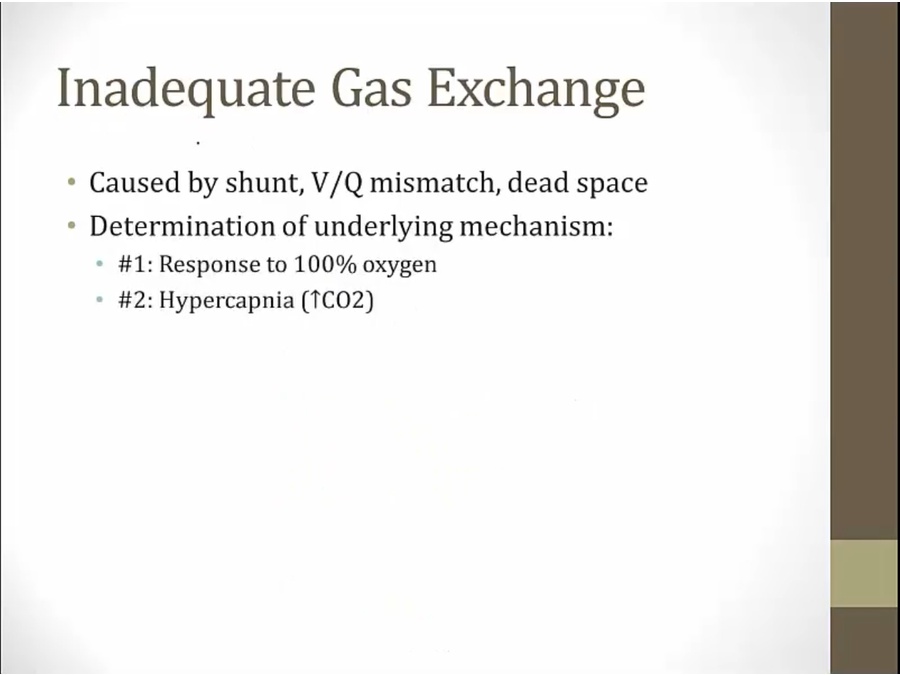
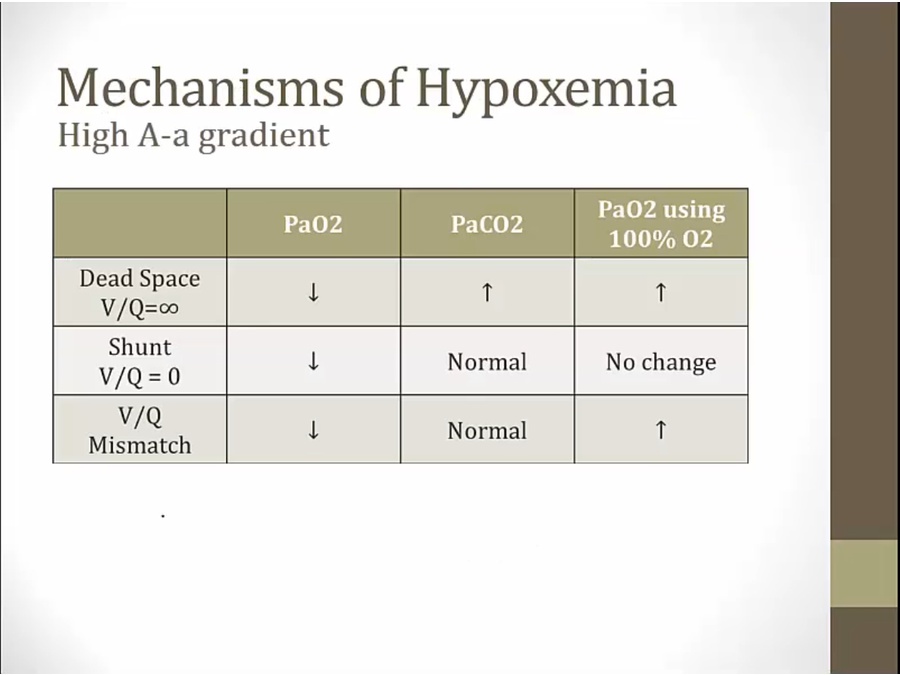
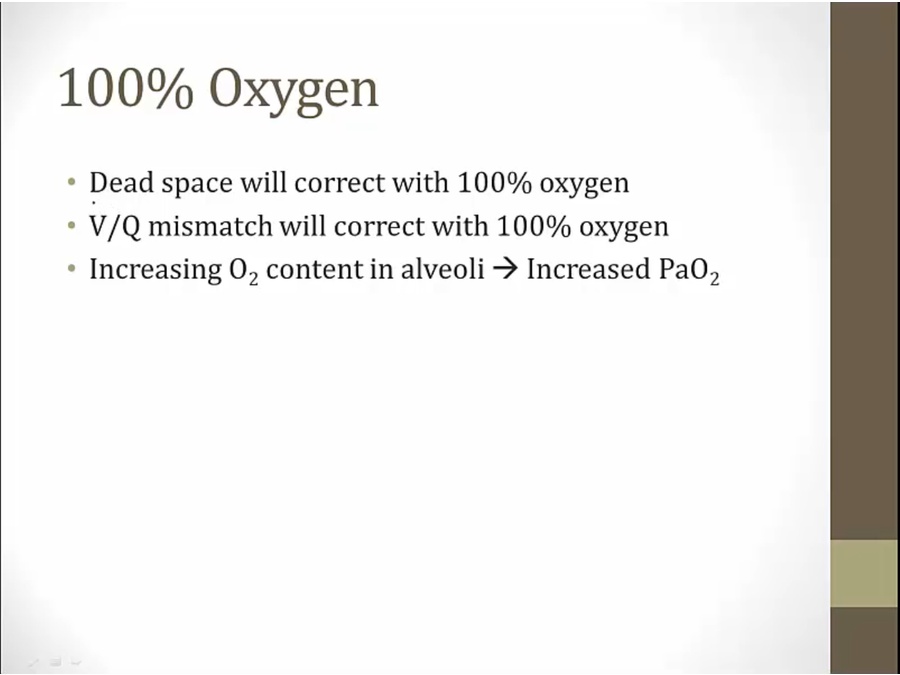
100% O2
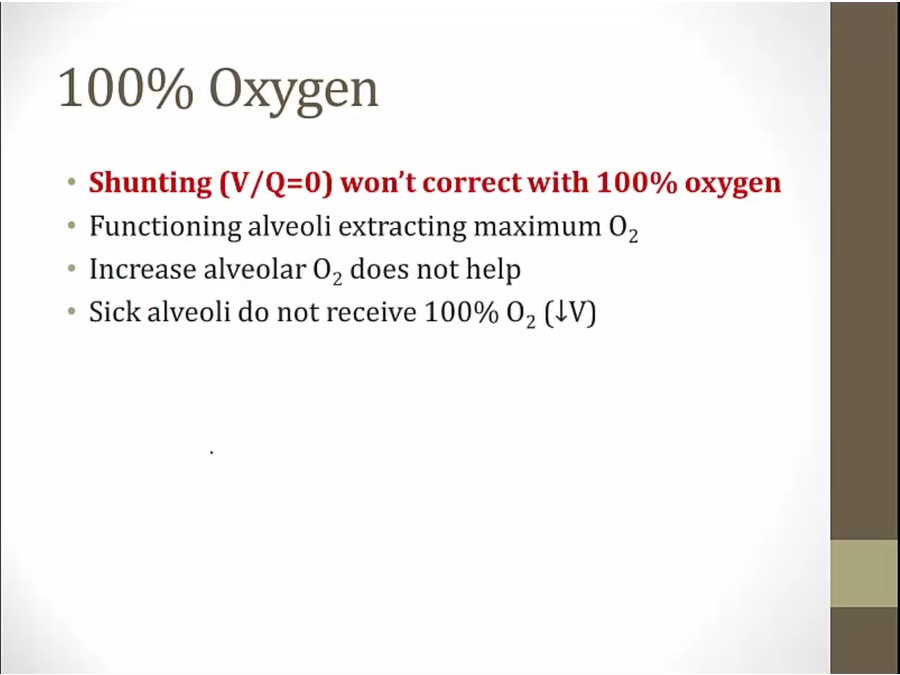
- O2 only goes to right side
- nothing changes on left side, even if give 100% O2
- hypoxemia persists
- all blood pushed to right side, Q very high
- hypoxemia if on room air, 21%
- can fix hypoxemia if changed to 100% O2
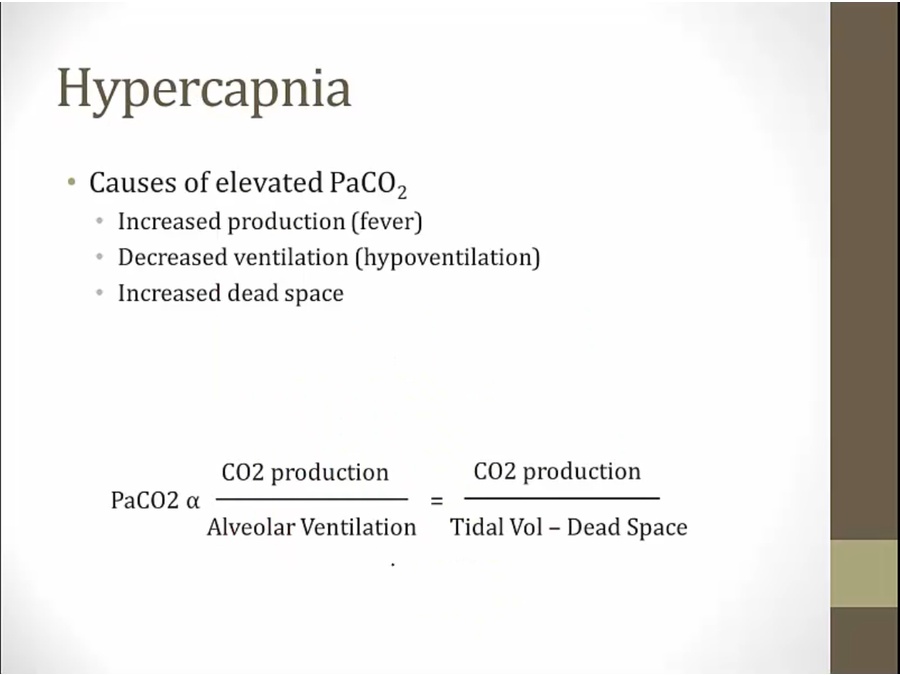
Hypercapnia
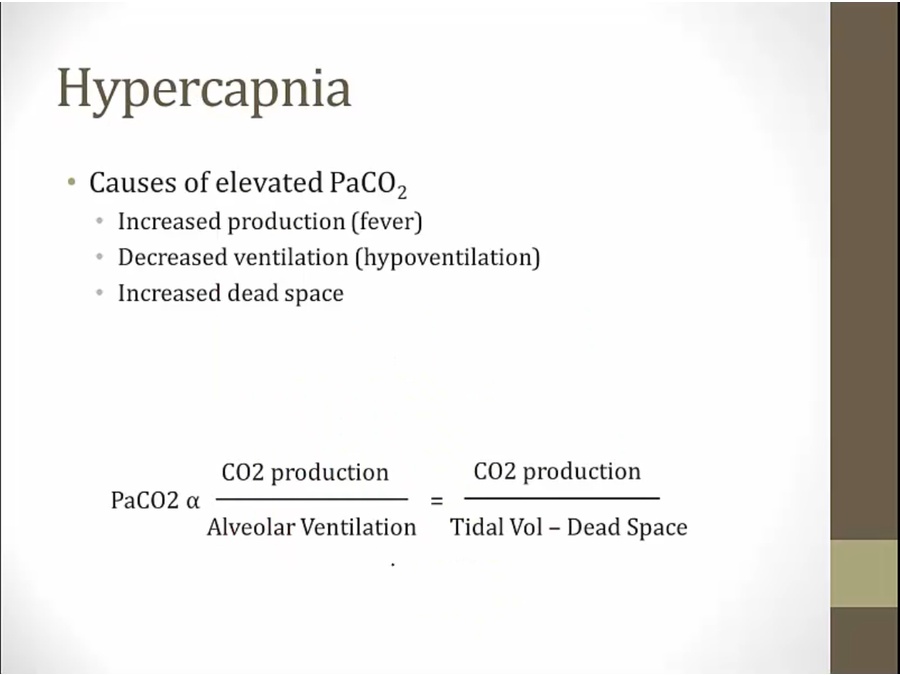
- increased dead space causes hypercapnia
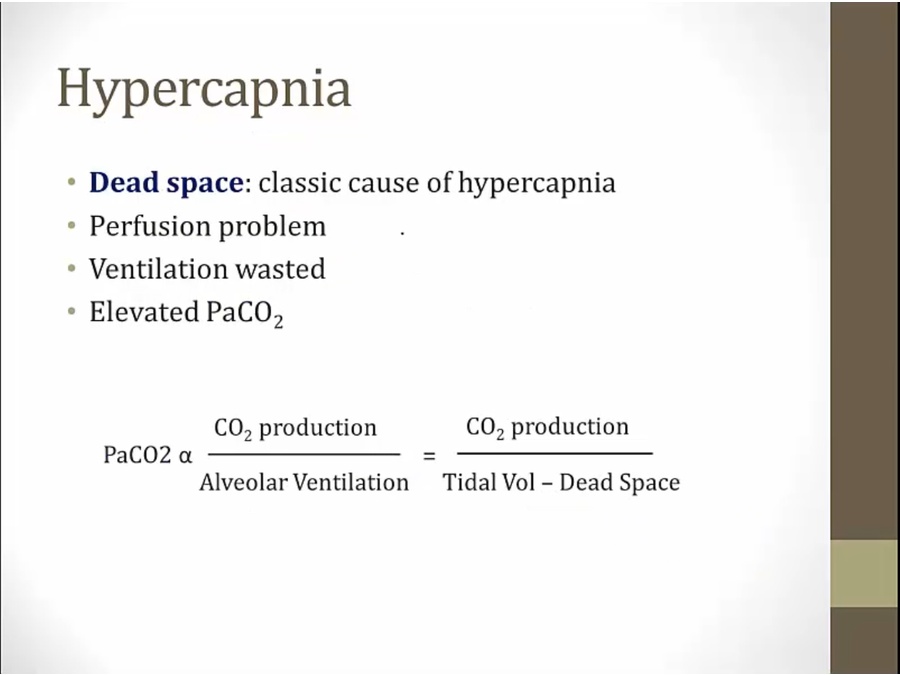
- when patient ventilates, none of the ventilation wasted on left side
- less ventilation to left side
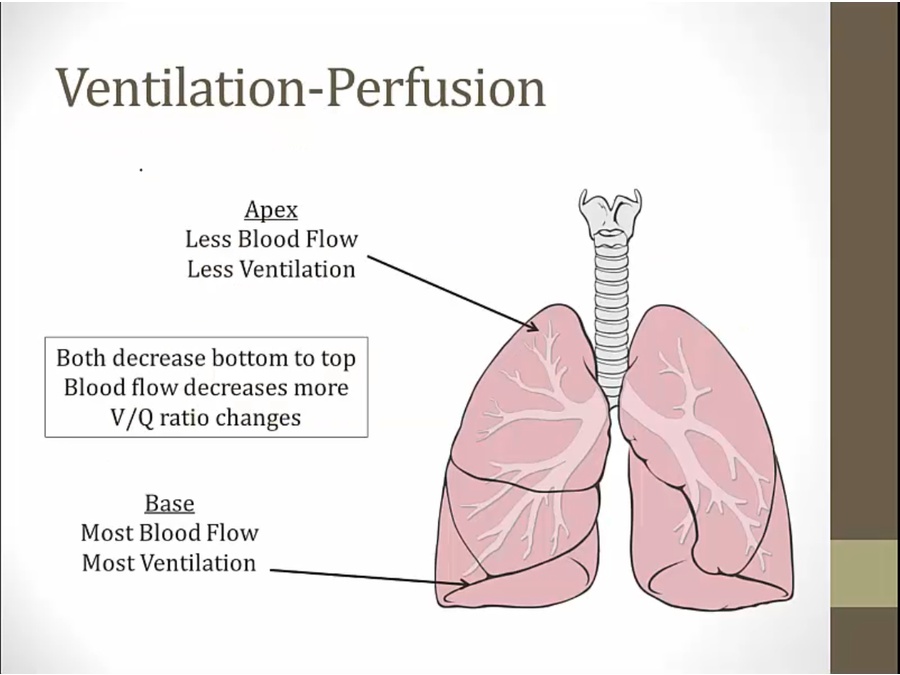
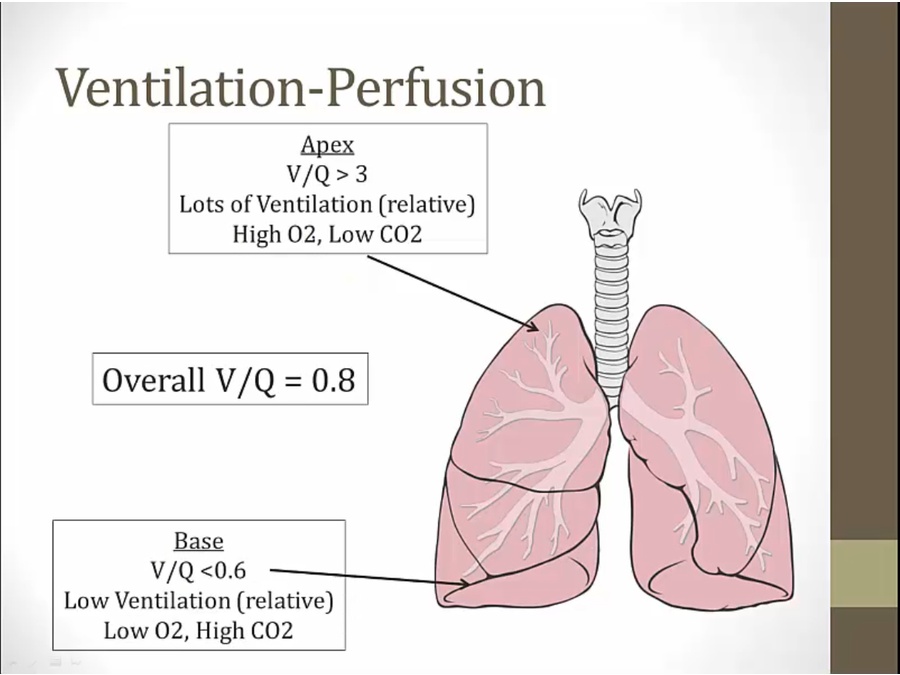
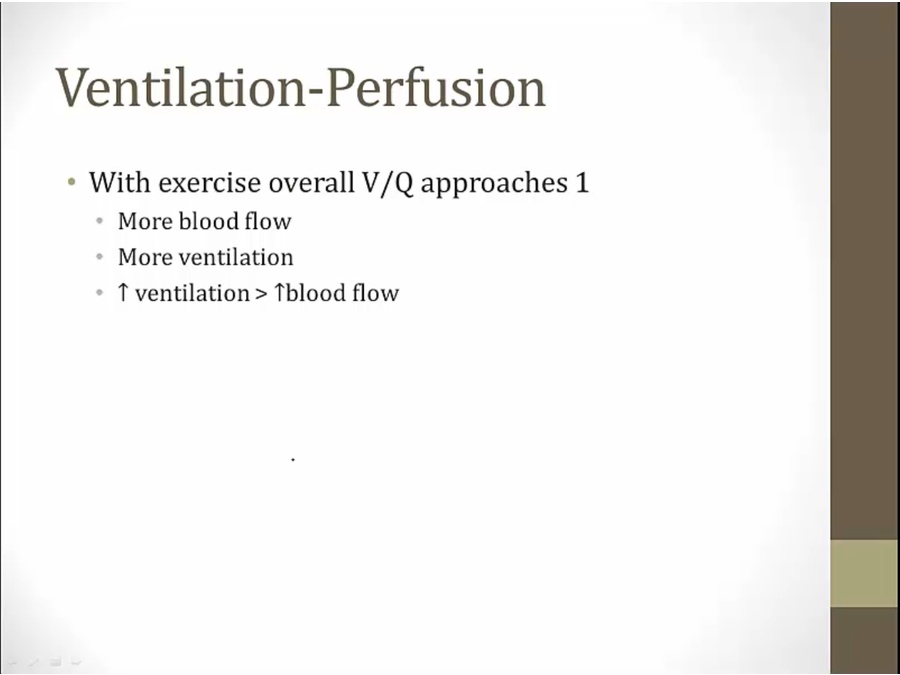
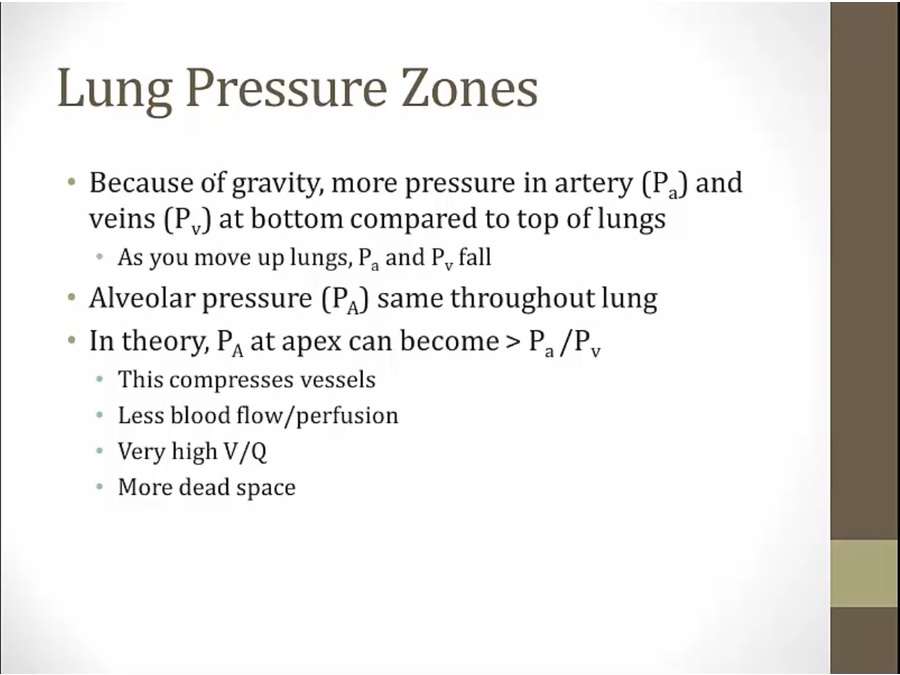
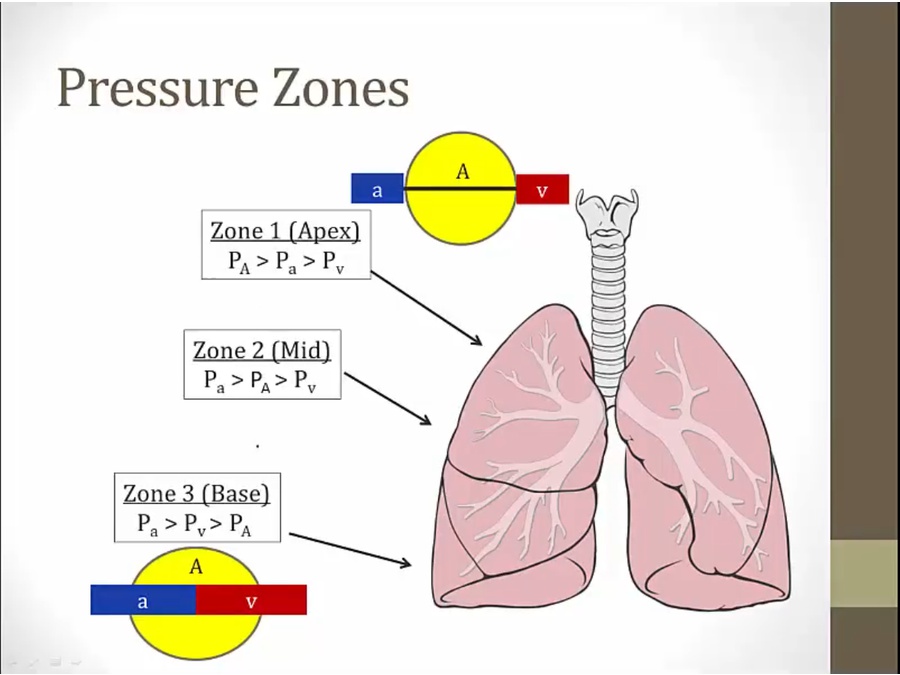
Lung Zones
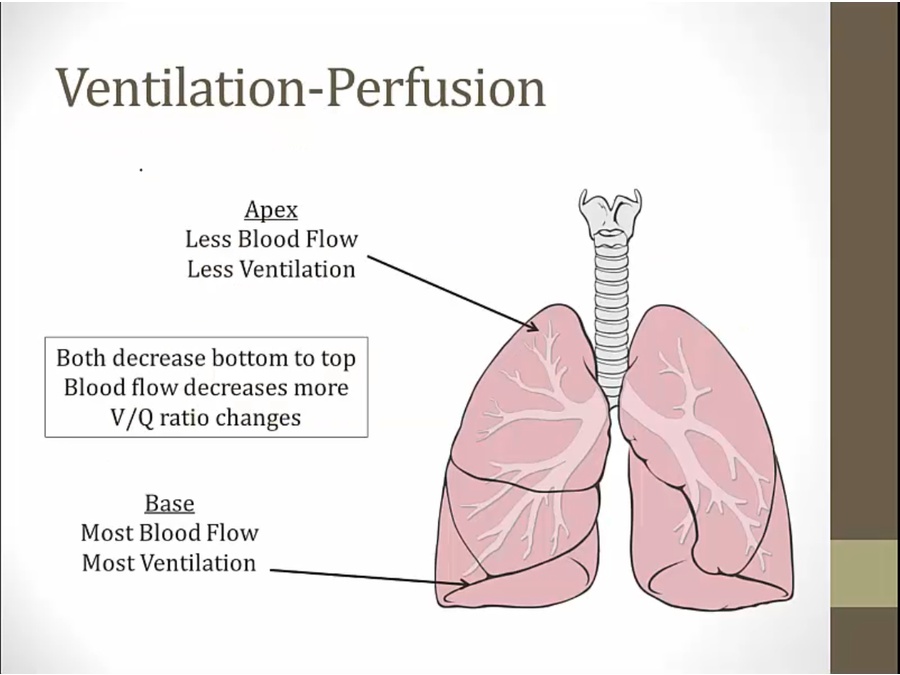
- apex least blood flow: blood has to push up against gravity
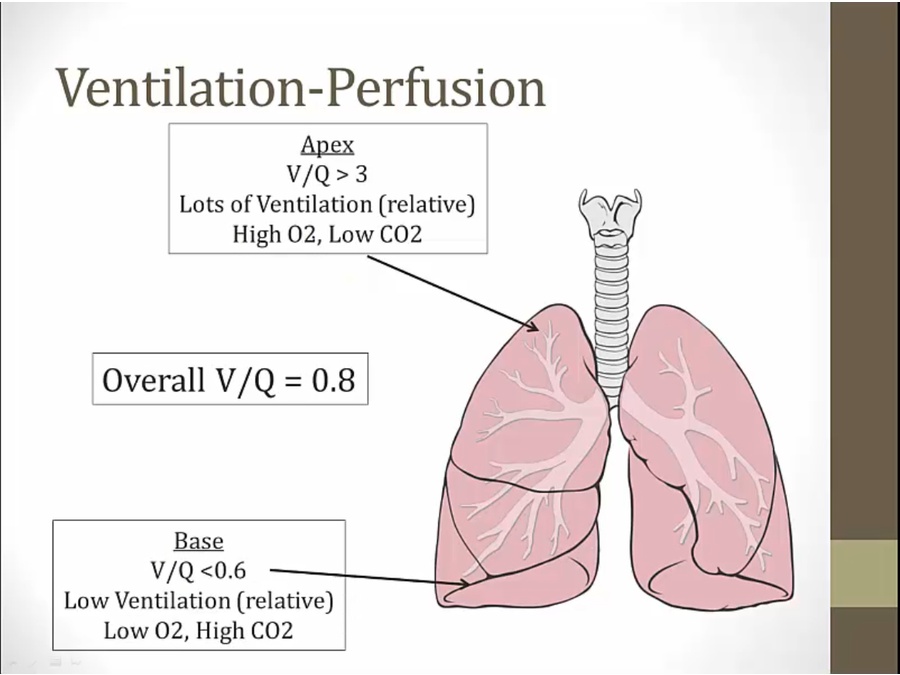
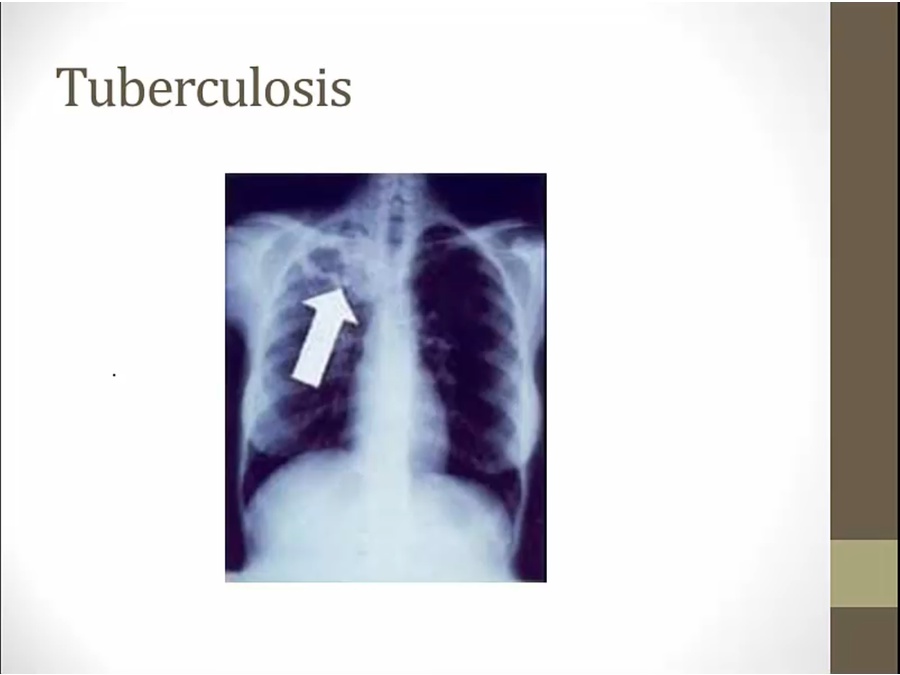
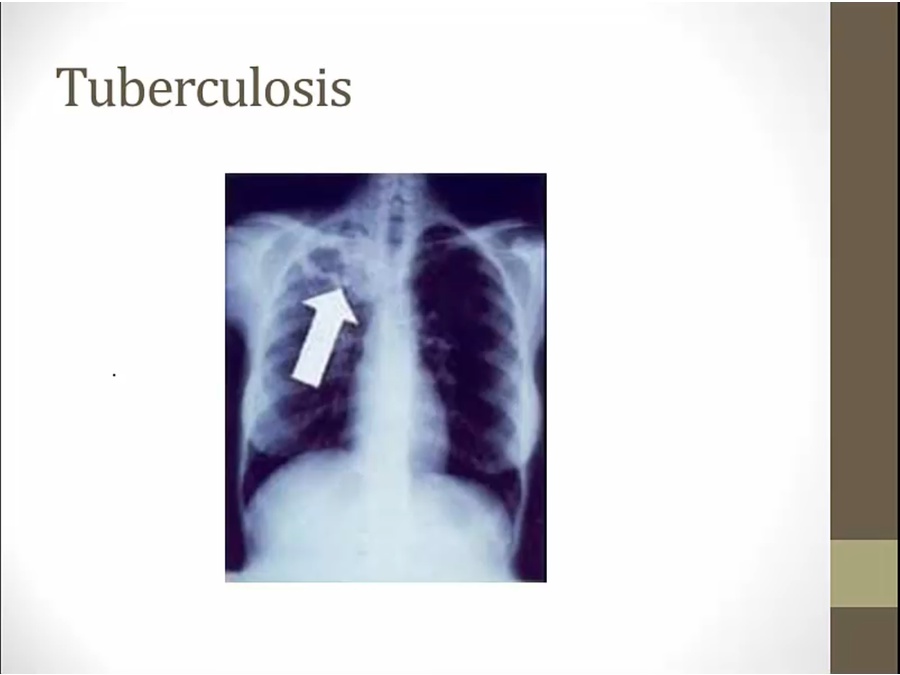
- Tb has affinity for highly oxygenated part of body, upper lobe
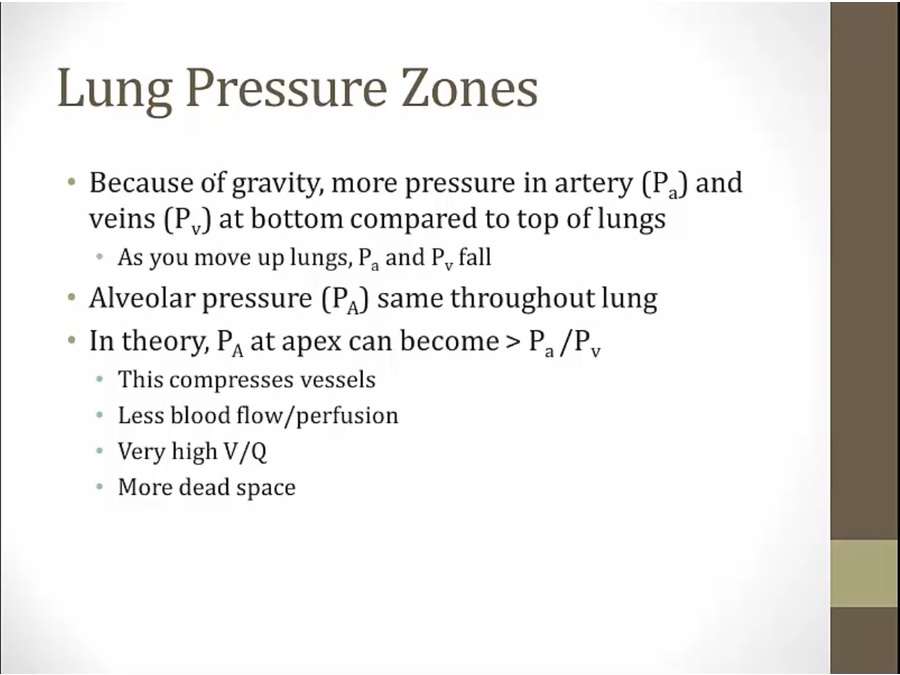
- more hydrostatic pressure at bottom
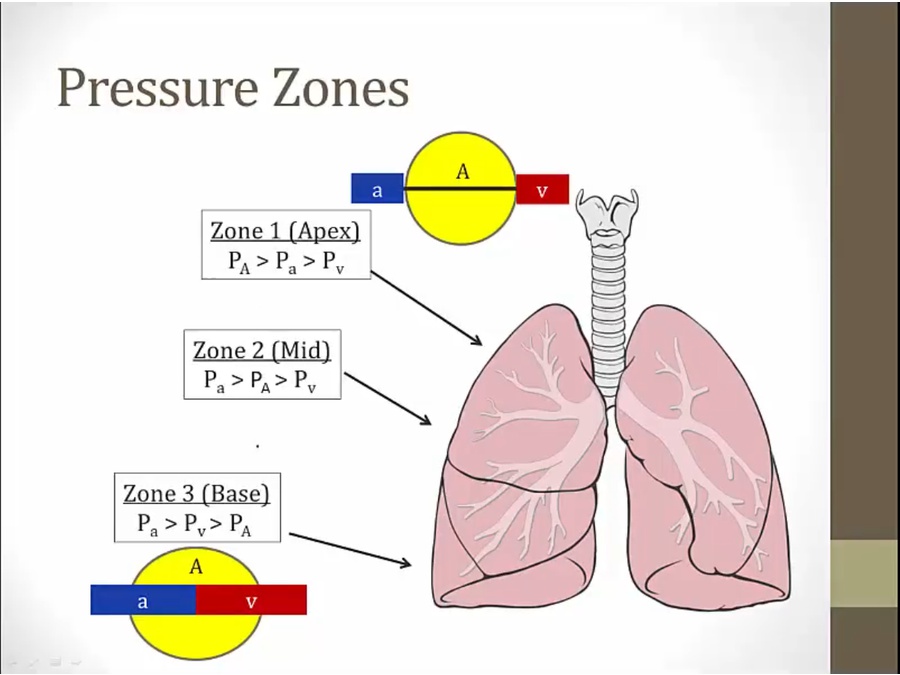
- bottom blood vessels fully extended; blood flow normally
- top: alveolar pressure higher, compress vessels, no blood flow
- middle: compress veins, pulsatile flow when RV contract to push blood through but no flow in veins in diastole
- in real life, most lungs are all zone 3
- in pathologic state: more lungs in Zone 1, especially ventilator (pressure in alveoli very high )
Backlinks