04 Adrenal Disorders
Adrenal disorders are divided into 4 types:
- Excess cortisol: Cushing's
- Insufficient cortisol: adrenal insufficiency
- Excess mineralocorticoids: aldosteronism
- Tumors: pheochromocytoma, paraganglioma, neuroblastoma, adenomas
Management
Cushing's
Syndrome with excess cortisol.
Cause
Most common cause:
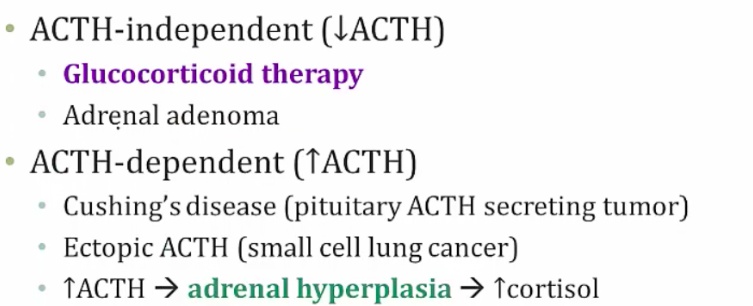
Types of Cushing's syndrome
- ACTH-independent: either exogenous cortisol (steroid) therapy or adrenal adnenoma producing cortisol. In this case, there would be a low ACTH from pituitary because of negative feedback
- ACTH-dependent: tumors secreting ACTH. Could be Cushing's disease (pituitary ACTH tumor) or small cell lung cancer
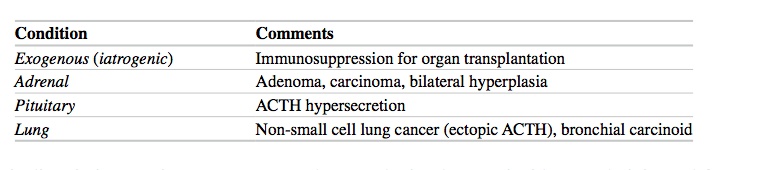
With exogenous, there's bilateral atrophy. In primary adenoma, there is 1 large and 1 small adrenal. Paraneoplastic and ACTH secreting must be distinguished because both have enlargement..
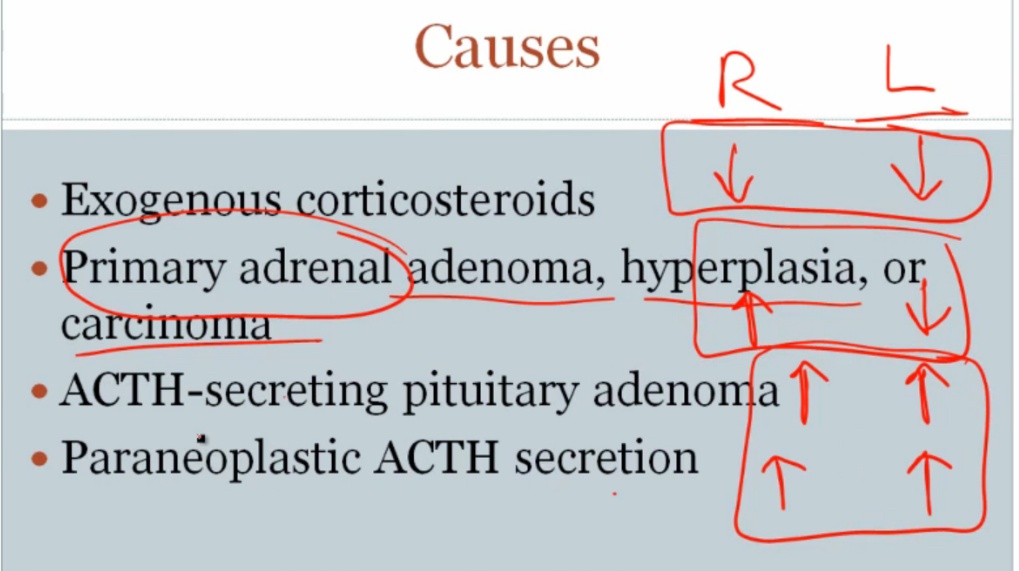
The decreased ACTH levels can lead to bilateral adrenal atrophy..
Only happens in ACTH dependent. Can be Cushing's disease (pituitary ACTH tumor) or small cell lung cancer..
ACTH dependent Examples
- An ACTH-secreting pituitary adenoma
- Paraneoplastic syndromes (e.g. renal cell carcinoma, small cell lung cancer, bronchial carcinoids, neural tumors)
Symptoms
Symptoms are:
- The usual high cortisol and associated symptoms
- Low FH/LSH and associated symptoms
- Stimulation of adipocytes and obesity
- Thinning of skin
- osteoporosis
- very common in women
- fat growth
- Moon face: round like the moon


- cortisol inhibits fibroblasts/collagen
- Most easily seen with forearm..
Diagnosis
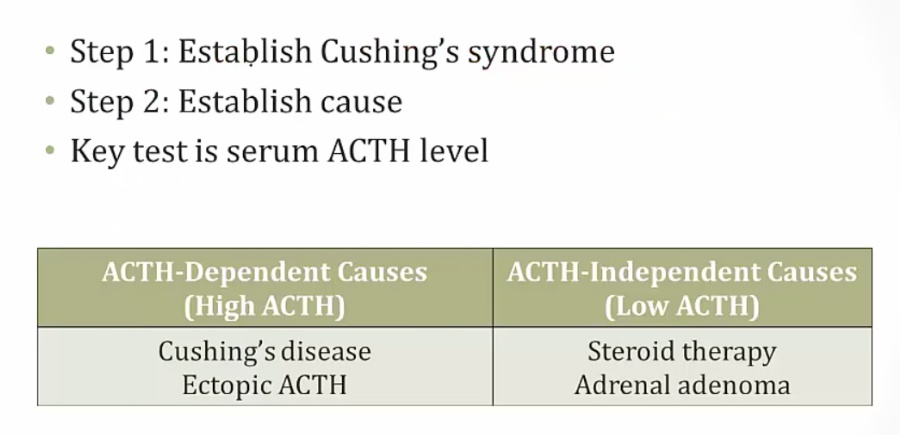
Steps for diagnosing Cushing's:..
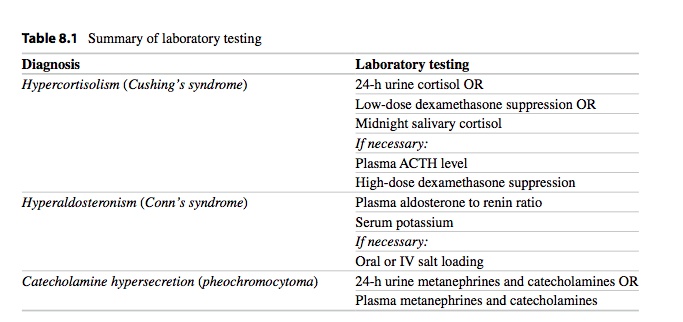
- Diagnosis Cushing's via 24 hour cortisol level or low dose dexamethasone suppression test
- Find cause by measuring ACTH
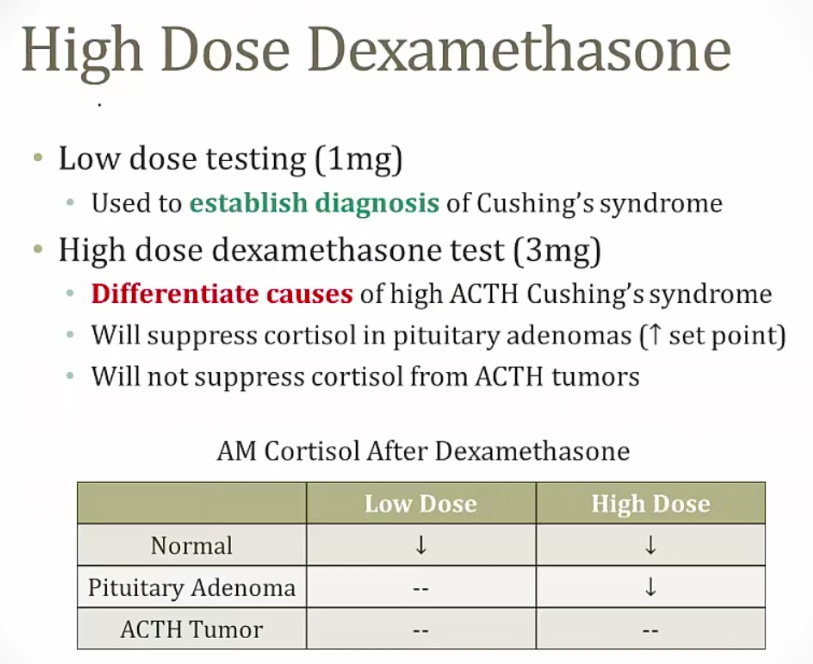
- If high ACTH, use high dose dexamethasone to differentiate between pituitary or ACTH tumors
Step 1, diagnosis Cushing's
- Can also use low dose dexamethasone suppression test
Low dose dexamethasone suppression test
- Diagnosis for Cushing's syndrome
Step 2, find cause
Step 3, Pituitary vs ACTH
- Pitutary adenoma still responds to negative feedback from cortisol
- If pituitary adenoma: confirm with MRI
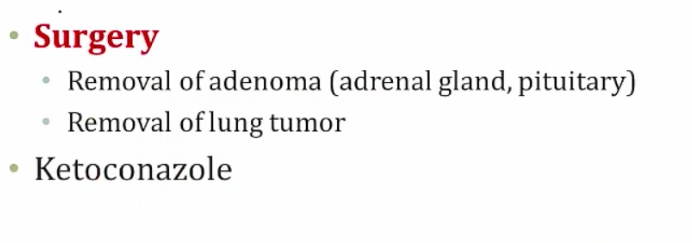
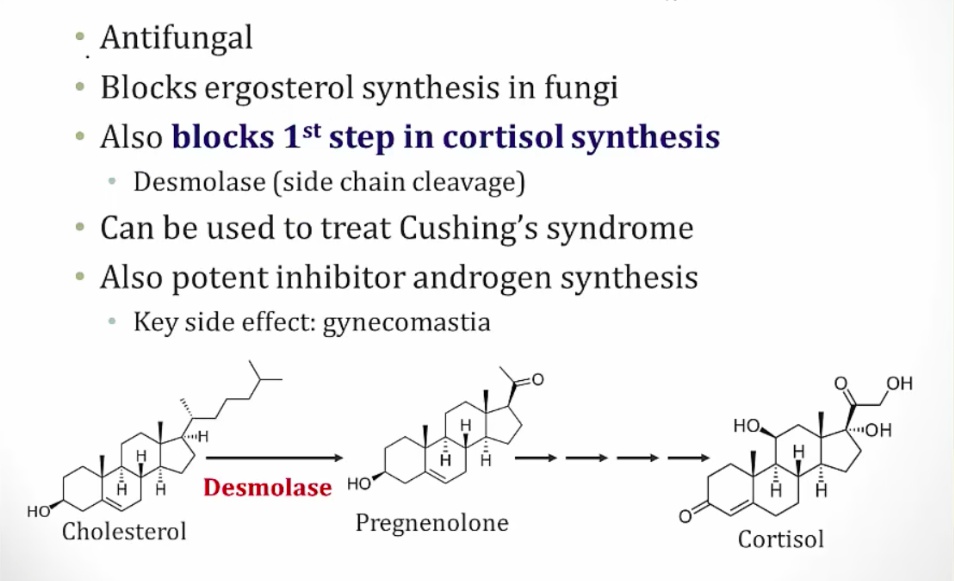
Treatment
 ..
..
 ..
..
Adrenal Insufficiency
Insuficient cortisol, aldosterone.
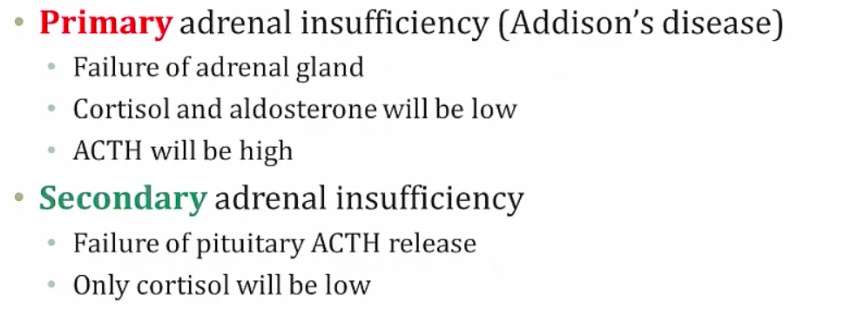
In contrast with primary adrenocortical insufficiency (Addison’s disease), secondary adrenocortical insufficiency has:
- No hyperpigmentation: since ACTH levels are low, melanocyte-stimulating hormone is not elevated as in Addison's disease
- No hyperkalemia: aldosterone synthesis is preserved, and release is regulated by the renin-angiotensin-aldosterone system..
Metyrapone test
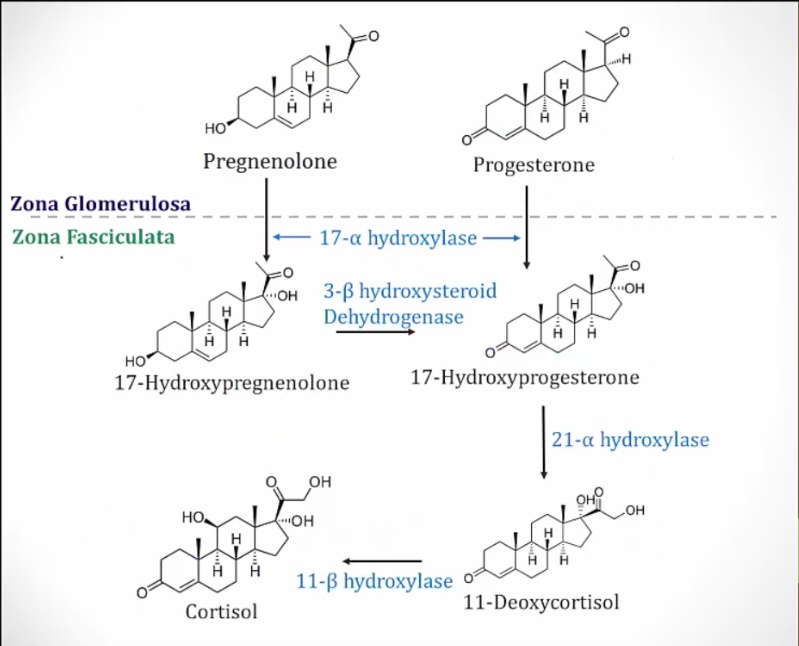
To determine the cause of the defect and confirm the diagnosis, a metyrapone test may be performed. Metyrapone inhibits 11-β-hydroxylase, which is responsible for the conversion of 11-deoxycortisol into cortisol.
- In a patient with a fully intact HPA axis, metyrapone administration will result in increased ACTH levels and increased 11-deoxycortisol levels.
- In primary adrenocortical insufficiency, metyrapone administration will result in increased ACTH levels and no change in 11-deoxycortisol levels.
- In secondary adrenocortical insufficiency, metyrapone administration will not change levels of ACTH or 11-deoxycortisol.
 ..
..
Primary Adrenal Insufficiency
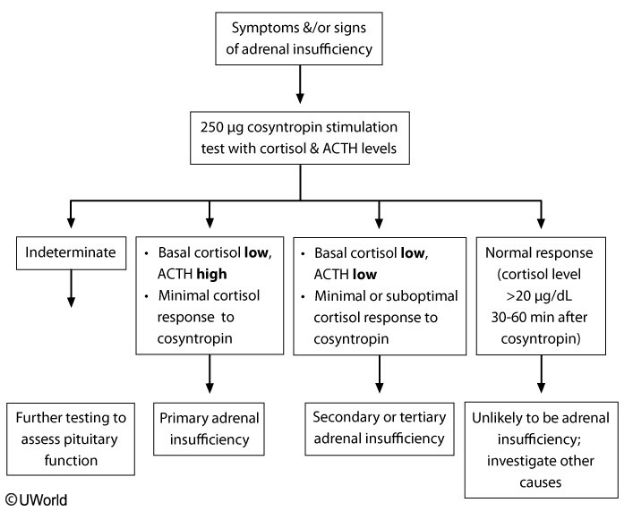
Diagnosis: cortisol and ACTH levels.
Cosyntropin (synthetic ACTH) should result in a brisk increase in cortisol levels. An abnormal cosyntropin (ACTH) stimulation test implies a subnormal response of plasma cortisol following cosyntropin administration, and it is definitive and diagnostic of primary adrenocortical insufficiency..
Symptoms
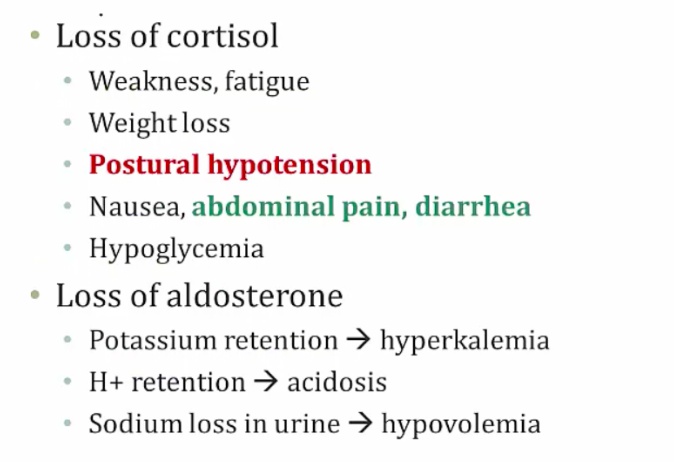
Skin hyperpigmentation (buccal mucosa, skin creases) occurs because elevated ACTH occurs alongside elevated melanocyte-stimulating hormone (MSH) because pro-opiomelanocortin (POMC) is the shared precursor molecule for MSH and ACTH (as well as beta-endorphin).
In primary insufficiency, hormone replacement of glucocorticoids, mineralocorticoids, and in some cases androgens, is indicated.
- Glucocorticoid (hydrocortisone and prednisone- dosage often needs to be adjusted when initiating treatment)
- Mineralocorticoid (fludrocortisone- dosage tailored to manage blood pressure and fluid balance)
- Androgens (dihydroepiandrosterone (DHEA)- recommended for some women to improve libido and well-being)..
Tertiary Adrenal Insufficiency
Rapid cessation of chronic high-dose glucocorticoids can cause this.
In secondary/tertiary insufficiency, only glucocorticoid replacement is necessary. Aldosterone deficiency is not an issue because aldosterone secretion is regulated predominantly by angiotensin II (not ACTH). Skin hyperpigmentation (the result of increased ACTH release) is also not an issue in secondary/tertiary insufficiency..
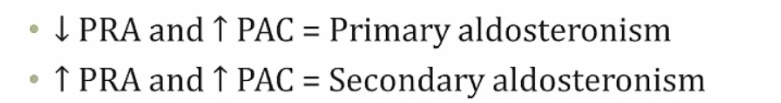
Excess Mineralcorticoids
Primary vs secondary:
- PRA: Plasma renin activity
- PAC: Plasma aldosterone concentration..
Diagnosis method
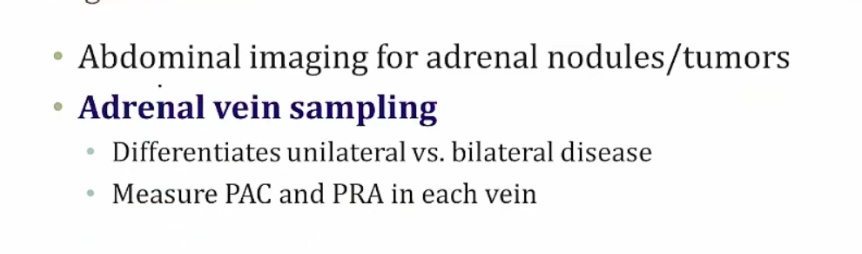
Primary Aldosteronism
Cause:
Labs.
Symptoms:
- Classic: young age hypertension (not expected)
- Hypokalemia: weakness, muscle cramps (unreliable finding because diet)..
Treatment..
- Aka apparent mineralcorticoid excess
- Eat a lot of licorice = looks like hyperaldosteronism
- Cortisol makes aldosterone and is broken down into cortisone
- Licorice inhibits the breakdown = more cortisol = more aldosterone
- Lower plasma aldosterone..
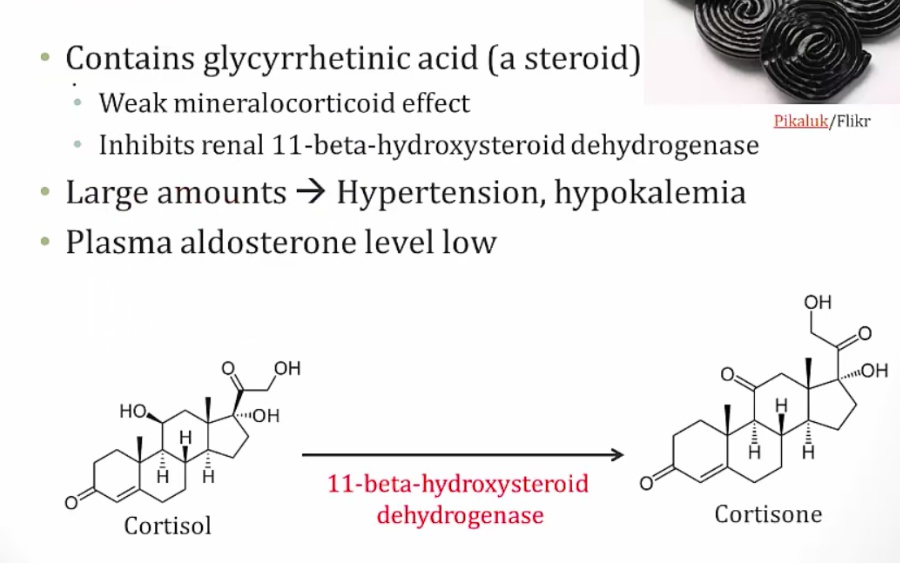
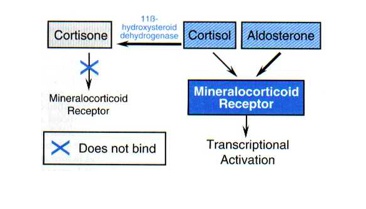
11B HSD
Degrades cortisol in adrenal gland and kidney to protect from aldosterone effects.
Conn Syndrome
Aldosterone producing adenoma.
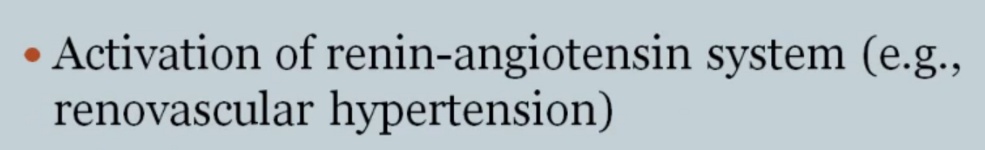
Secondary Hyperaldosteronism
Cause
Labs
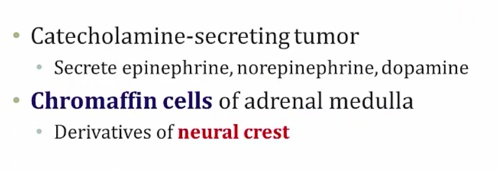
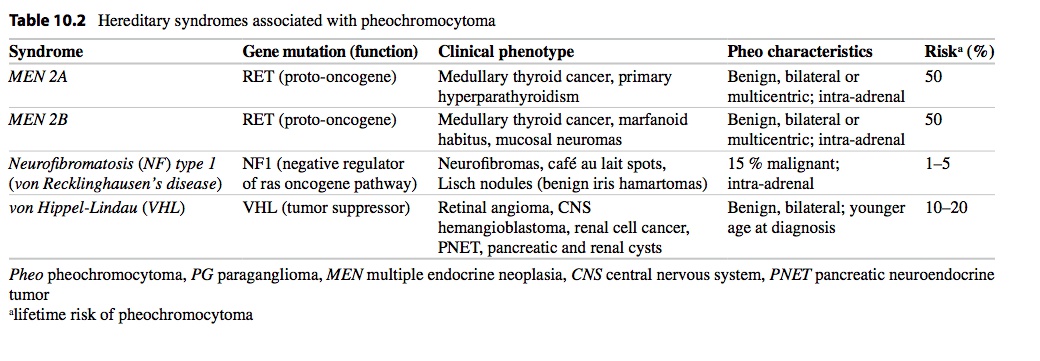
Tumors
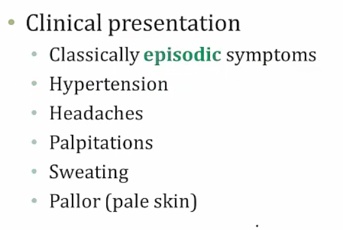
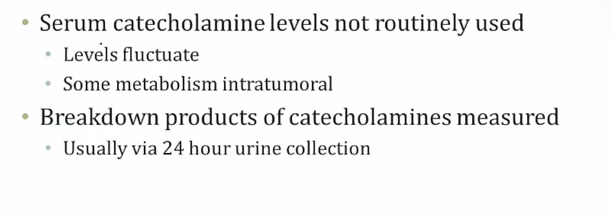
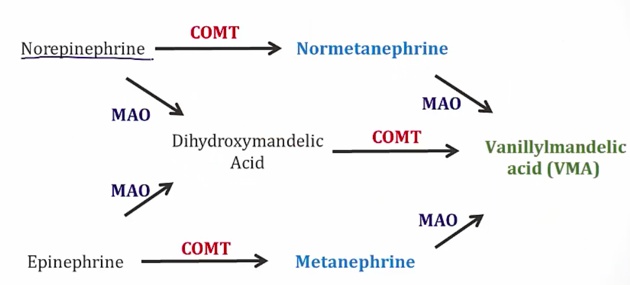
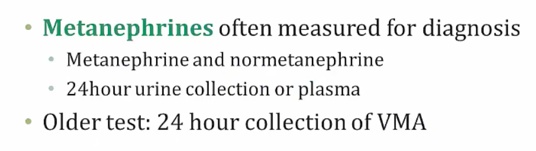
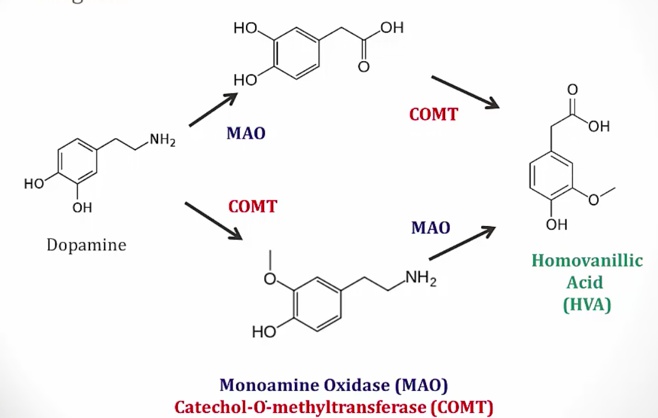
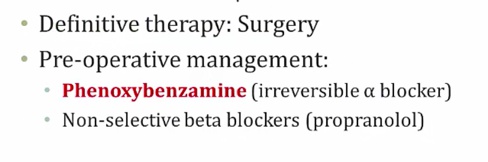
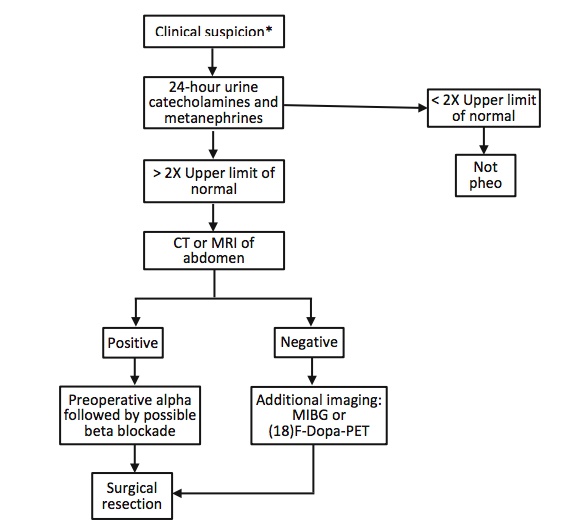
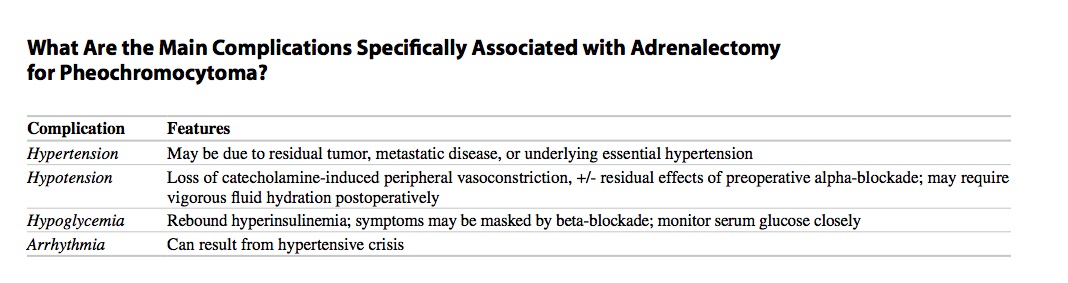
Pheochromocytoma
.
.
Paraganglioma
.
Neuroblastoma
.
.
.
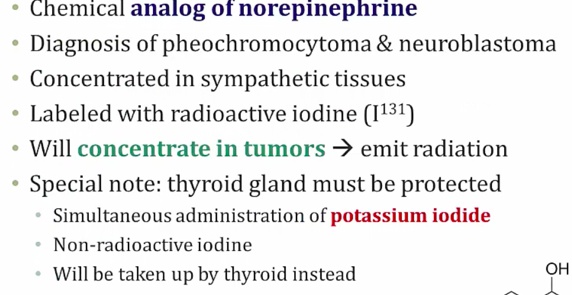
MIBG
.
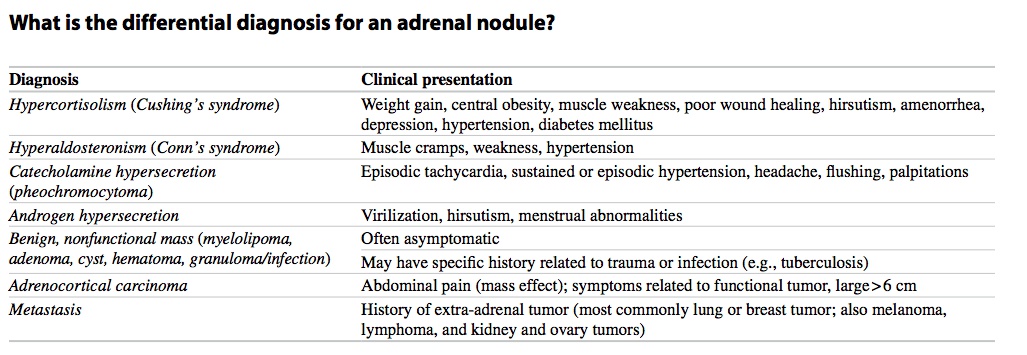
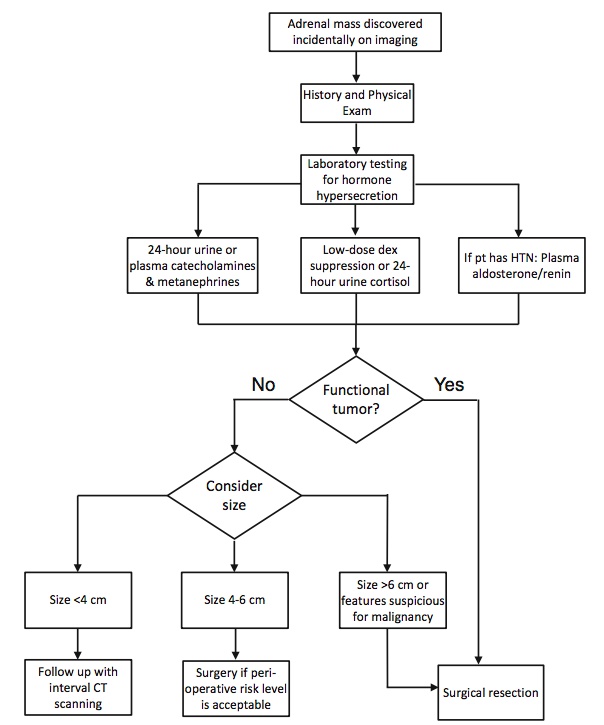
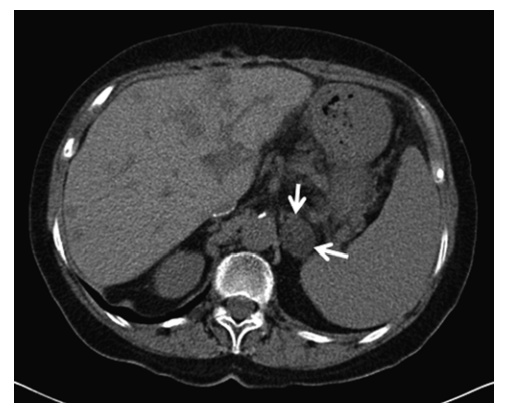
Incidental, nonfunctional adenoma

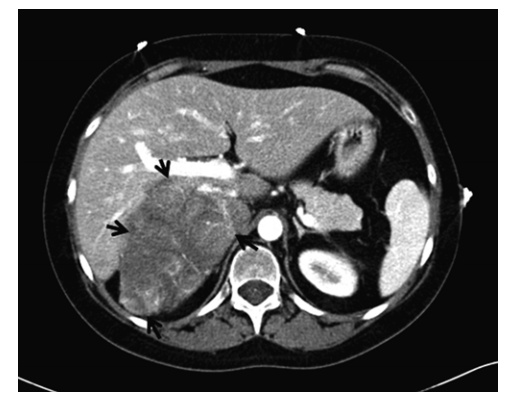
An incidentaloma is an incidentally discovered mass seen on imaging performed for an unrelated reason. Approximately 5 % of patients who undergo an abdominal CT scan will have an incidentally discovered adrenal mass. The incidence increases with patient age, with up to 10 % of patients having adrenal nodules on autopsy studies.
Cortical Carcinoma