yersinia
- related: ID
Primary pneumonic plague occurs after Yersinia pestis exposure through infectious aerosols and person-to-person transmission through respiratory droplets, which are likely scenarios for bioterrorism. Patients with suspected pneumonic plague require droplet precautions.
Bubonic plague is characterized by lymphadenopathy (buboes), fever, rigors, and headache. Chest radiographs are nonspecific. Gram stain and cultures of sputum and blood (performed using the highest level biosafety procedures) are often diagnostic.
Untreated, pneumonic plague is uniformly fatal. Asymptomatic persons exposed to aerosolized Y. pestis and close contacts of infected patients within the previous 7 days warrant postexposure prophylaxis. The available vaccine is ineffective at protecting against pneumonic plague. A live attenuated vaccine with protection from respiratory challenge is under investigation.
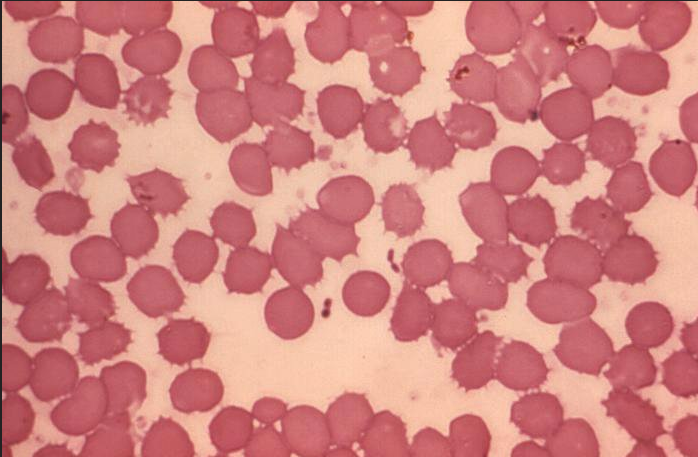
The most appropriate treatment is gentamicin. This patient most likely has pneumonic plague caused by the bacteria Yersinia pestis, one of the biologic agents classified as an A-list bioterrorism pathogen because of its high potential lethality and ease of dissemination. Sputum Gram stain (and possibly blood smear) may identify gram-negative coccobacilli demonstrating the classic bipolar staining or “safety pin” shape shown. Although most pulmonary involvement occurs through secondary hematogenous spread to the lungs from a bubo or other source, primary pneumonic plague can occur after close contact with another person with plague pneumonia, after animal exposure, or as a result of intentional aerosol release for the purpose of terrorism, as in this case. Recommended first-line treatment is either streptomycin or gentamicin.
Anthrax is caused by Bacillus anthracis, a gram-positive, aerobic organism. It appears as a sporulating gram-positive rod on microscopic examination. Patients with inhalational anthrax present with low-grade fever, malaise, myalgia, and headache accompanied by cough, dyspnea, and chest pain. A chest radiograph showing mediastinal widening from hemorrhagic lymphadenitis is characteristic. Ciprofloxacin, levofloxacin, moxifloxacin, or doxycycline should be provided as soon as possible after any actual or suspected case of anthrax that raises concern for a bioterrorism attack.
Ambulatory empiric therapy for community-acquired pneumonia (CAP) is directed against Streptococcus pneumoniae, Haemophilus influenzae, and atypical bacteria, even though a significant proportion of patients with CAP infected with viral pathogens do not benefit from antibiotic therapy. The combination of ceftriaxone and azithromycin would be an appropriate choice for the treatment of CAP but would be inadequate for treating plague, which requires either streptomycin or gentamicin.
When clinical concern for Pseudomonas is present, dual therapy with two active agents is indicated. Options include an antipseudomonal β-lactam (piperacillin-tazobactam, cefepime, or meropenem) in conjunction with either a quinolone (levofloxacin or ciprofloxacin) or an aminoglycoside. Pseudomonas infection should be considered in immunocompromised patients and patients with underlying structural lung disease (bronchiectasis or cystic fibrosis) or medical conditions requiring repeated courses of antibiotics. The combination of piperacillin-tazobactam and levofloxacin would be ideal for a seriously ill patient with CAP and concern for Pseudomonas infection but not for this patient most likely infected with Yersinia pestis.