sarcoidosis
- related: Step 3, Allergy and Immunology
Sarcoidosis
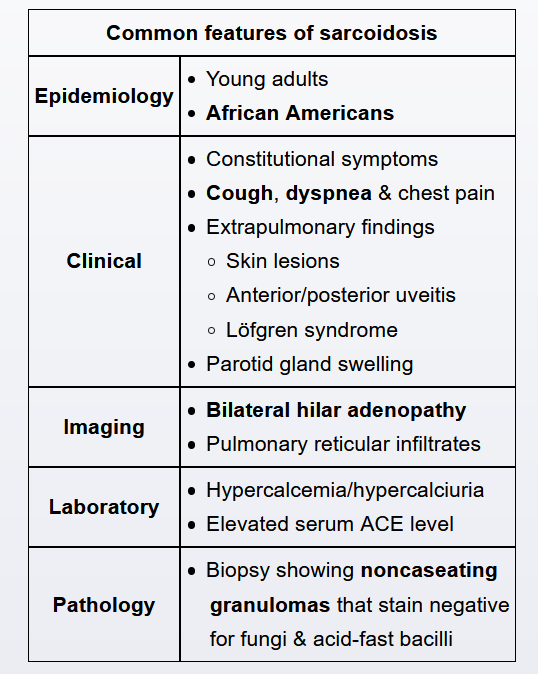

Sarcoidosis is a systemic inflammatory disease characterized by multiorgan noncaseating granulomas. Most patients with sarcoidosis seek medical attention due to pulmonary disease (eg, cough, dyspnea), but extrapulmonary manifestations in the eyes, skin, heart, and joints are common. Ocular disease occurs in approximately 25% of patients with sarcoidosis at some point during illness and is the presenting symptom in 5% of cases. Patient with bilateral hilar lymphadenopathy, erythema nodosum, anterior uveitis likely has sarcoidosis.
This young adult with 3 months of exertional dyspnea and cough has hypercalcemia and bilateral hilar lymphadenopathy, raising suspicion for pulmonary sarcoidosis.
Sarcoidosis is a systemic inflammatory disorder characterized by the formation of noncaseating granulomas against an unknown antigen. Most cases arise in young adults and present with pulmonary (eg, cough, dyspnea, chest pain) and systemic (eg, fatigue, malaise, weight loss) symptoms. Clinical investigation often reveals:
- Bilateral hilar lymphadenopathy with or without diffuse interstitial infiltrates
- A mixed restrictive (reduced diffusion capacity for carbon monoxide) and obstructive (reduced FEV1 and FEV1/FVC) pattern on pulmonary function testing
- Hypercalcemia and elevated inflammatory markers (eg, erythrocyte sedimentation rate)
A biopsy (eg, bronchoscopy with transbronchial biopsy) is typically required for definitive diagnosis, with the notable exception of erythema nodosum, which does not demonstrate noncaseating granulomas even when occurring in association with sarcoidosis. Asymptomatic patients often require no treatment; those with symptoms or pulmonary function impairment usually receive 12-24 months of oral glucocorticoids. Most cases (75%) resolve over time and do not recur.
Most patients with sarcoidosis improve over time, but a minority have progressive lung disease (25%) or organ dysfunction (10%). These patients often require treatment with methotrexate, azathioprine, or tumor necrosis factor-alpha antagonists.
Renal
- can have interstitial nephritis