roux-en-y
- related: GI
- tags:
- can cause recurrent calcium renal stones from malabsorption
- Malabsorption causes more intestinal fatty acid binding to calcium, which increases colonic oxalate absorption and renal oxalate excretion.
Diabetes
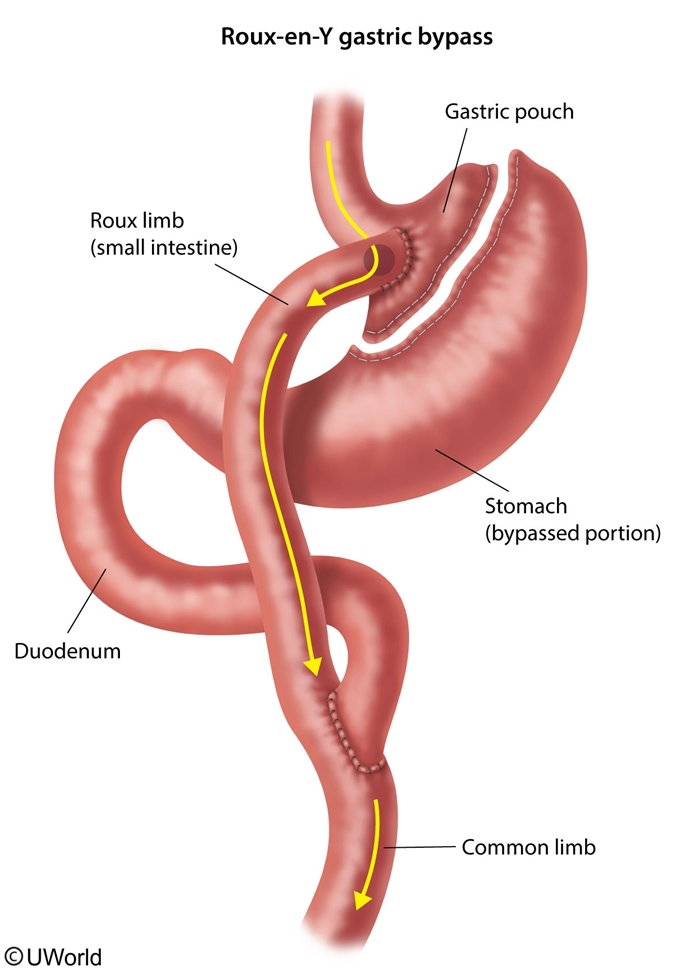
Randomized controlled trials have shown that Roux-en-Y gastric bypass is more effective than conventional medical therapy (eg, lifestyle changes, weight management counseling, oral hypoglycemics, insulin) in patients with uncontrolled type 2 diabetes and severe obesity (BMI >35). In one study, 42% of patients achieved a hemoglobin A1c <6.0% at 12 months with combined medical therapy and Roux-en-Y gastric bypass, versus 12% of patients who received intensive medical therapy alone. In another study, 75% of patients who underwent Roux-en-Y gastric bypass alone achieved a hemoglobin A1c <7% at 12 months, versus 32% of patients who received intensive medical therapy alone.
Complications
This patient's clinical presentation is suggestive of outlet obstruction, a complication of Roux-en-Y bypass (RYGB) surgery. Stomal stenosis at the gastro-jejunal anastomosis is a common complication that occurs in about 5%-20% of RYGB patients. Patients typically present (3-6 months after surgery) with obstructive symptoms such as nausea, vomiting, abdominal pain, gastroesophageal reflux, dysphagia, and eventual inability to tolerate oral intake. Diagnosis is made with endoscopy and the treatment is endoscopic balloon dilation (serial dilations often required).
Cholelithiasis is another frequent RYGB complication that occurs in about 40% of patients due to rapid weight loss contributing to gallstone formation. The incidence of cholelithiasis may be decreased by prophylactic administration of ursodeoxycholic acid for up to 6 months after surgery.
Dumping syndrome occurs in about 50% of RYGB patients. Patients typically present with abdominal pain, nausea, hypotension (due to a rapid osmotic fluid shift from plasma into the bowel), and reflex tachycardia. This can be avoided by replacing simple carbohydrates with complex carbohydrates and high-fiber, protein-rich foods.
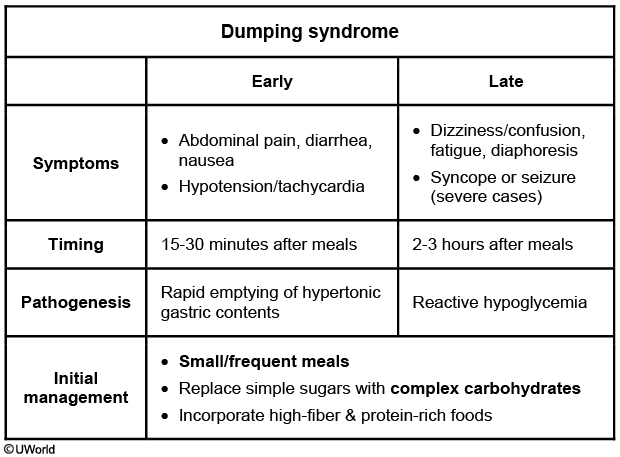
Dumping syndrome is subdivided into early or late based on the timing and etiology of postprandial symptoms. This patient's presentation is consistent with early dumping syndrome given the sudden onset of abdominal pain, diarrhea, and nausea within 15-30 minutes of eating. This is a consequence of rapid emptying of hypertonic gastric contents into the small intestine. Hypotension and tachycardia may also occur due to rapid fluid shifts between the plasma and high osmolality in the bowel.
In contrast, late dumping syndrome occurs 2-3 hours after eating and may present with dizziness/confusion, fatigue, and diaphoresis due to hypoglycemia (Choice B). Patients are initially hyperglycemic due to the speedy transit and absorption of simple carbohydrates in the small intestine; however, this is then countered by a surge of insulin causing hypoglycemia. Severe postprandial hypoglycemia may result in loss of consciousness or seizure. The initial management for both early and late dumping syndrome includes eating small/frequent meals, replacing simple sugars with complex carbohydrates, and incorporating high-fiber and protein-rich foods in the diet.