pheochromocytoma
- related: Endocrine
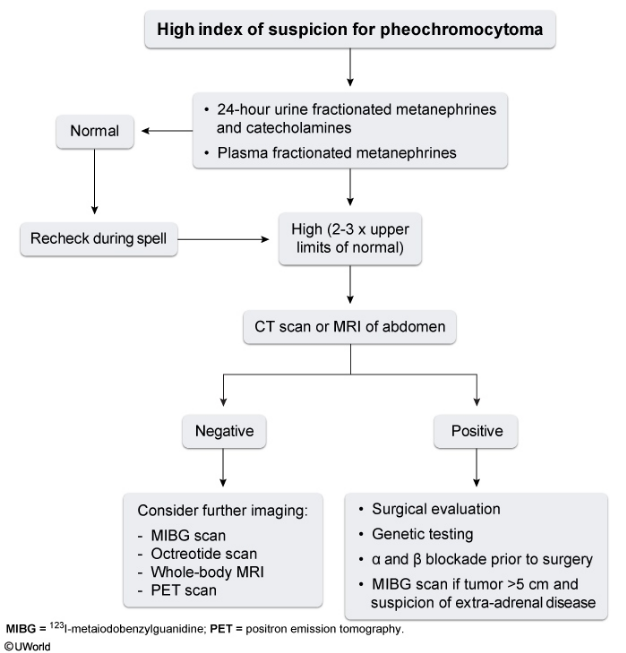
Abdominal imaging is the next step for localizing a pheochromocytoma after biochemical confirmation of the tumor. Both CT and MRI are highly sensitive for localizing pheochromocytomas, which are usually located in the adrenal glands. Clinically active pheochromocytomas are typically >4-4.5 cm in diameter and have a high tissue density on CT scan (generally 40-50 Hounsfield units). Larger tumors are more likely to have central necrosis and calcification. MRI usually shows high intensity on T2-weighted images.
Patients with negative abdominal imaging usually require further testing such as the metaiodobenzylguanidine (MIBG) scan, which is a functional scintigraphy with I123 labeled MIBG (Choice C). MIBG resembles norepinephrine, is taken up by adrenergic tissue, and can detect tumors not detected by CT or MRI. In addition, MIBG is also performed in patients with large tumors (>5 cm diameter) as they have a higher risk of malignancy and possible extra-adrenal disease. Younger patients and those with a familial disorder also require MIBG after initial CT or MRI as they have a higher risk of extra-adrenal and multiple tumors.
Surgical complications
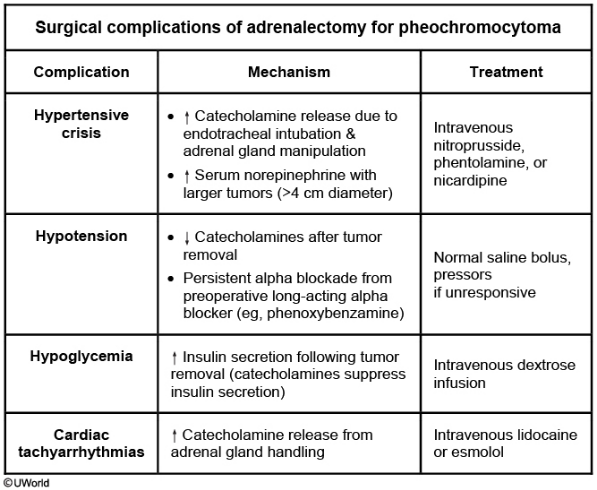
Even with adequate preoperative alpha blockade and adequate fluid replenishment, some patients with pheochromocytoma have intraoperative and postoperative complications. Hypotension is an important intraoperative complication due to decreased circulatory catecholamine levels following tumor removal. In addition, persistent preoperative alpha blockade results in decreased vascular tone. Intra- and postoperative hypotension usually responds well to normal saline bolus. Pressors may be required in patients who do not respond to intravenous fluids. Other complications include hypertensive crisis, hypoglycemia, and cardiac tachyarrhythmias.