Osteoporosis
- screening
- women age >65
- women postmenopausal, < 65 with following risks
- low body weight
- smoker
- fhx of hip fracture
- steroid use
- treatment:
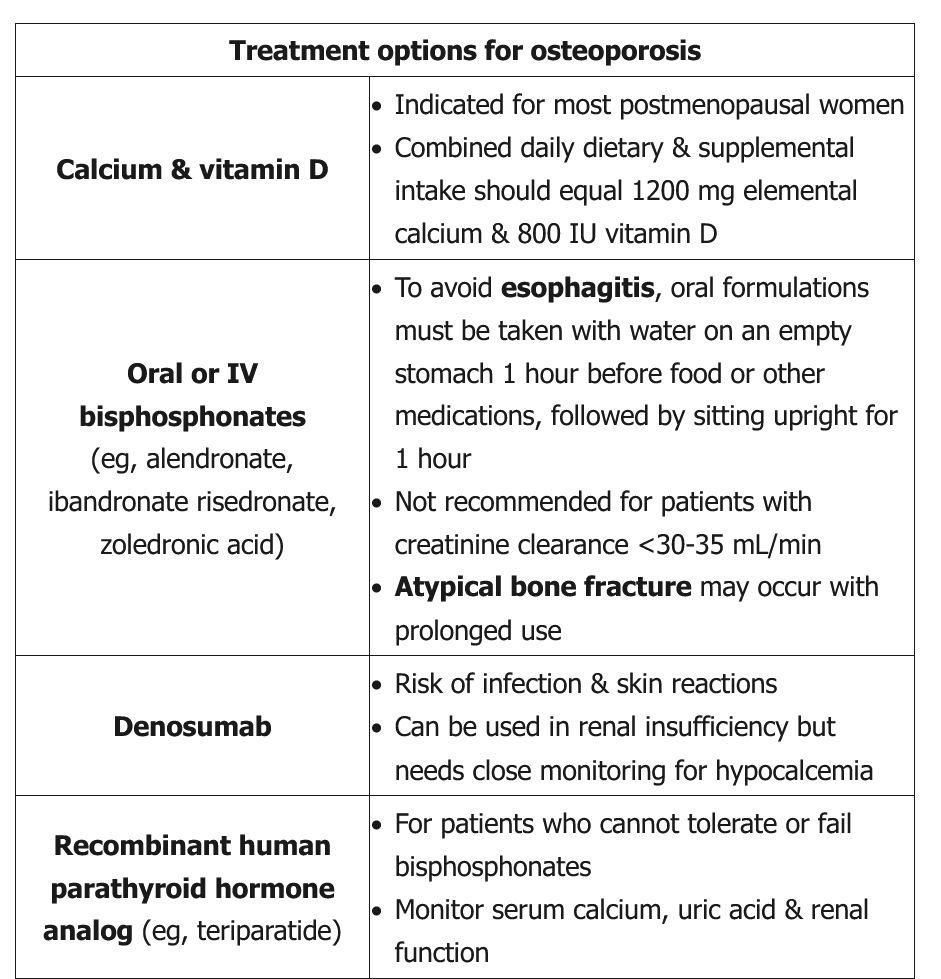
- counseled on regular weight bearing exercises and menopause supplements
- bisphosphonates (eg, alendronate) is indicated for patients who have:
- Low bone mass with a history of fragility fracture
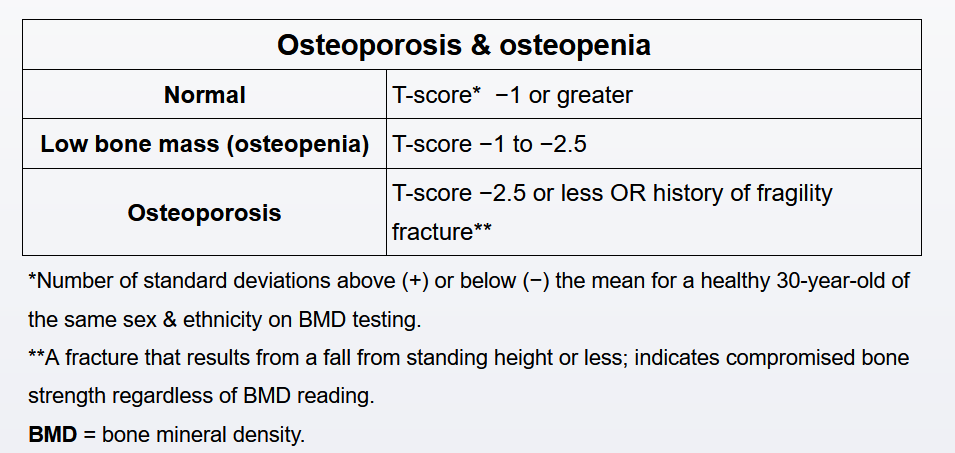
- Bone density criteria for osteoporosis (T-score <−2.5 on DXA)
- Osteopenia (T-score between −1 and −2.5) with a 10-year probability for major osteoporotic fracture >20% or hip fracture >3% based on the FRAX risk calculator
Most experts recommend periodic (eg, every 3-5 years) reassessment with DXA for postmenopausal women with osteopenia.
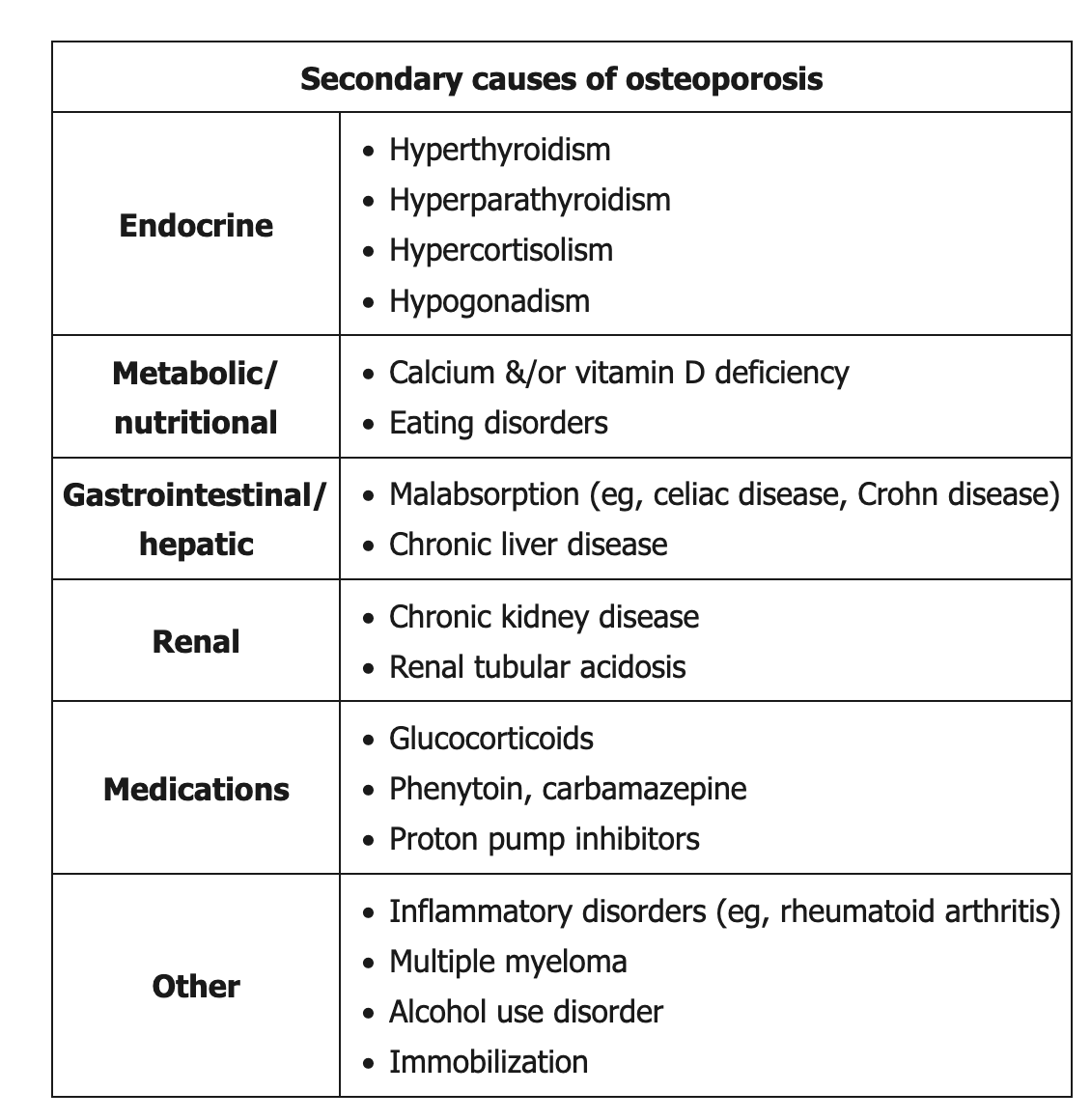
Secondary causes
However, patients with a new diagnosis of osteoporosis warrant a basic laboratory evaluation for reversible secondary causes. Typical studies include serum chemistries (eg, calcium, phosphorus, albumin, total protein, and renal and hepatic function markers) and complete blood count. In addition, vitamin D stores should be assessed with a 25-hydroxyvitamin D level. Intake of adequate amounts of vitamin D and calcium helps reduce bone loss.
Men
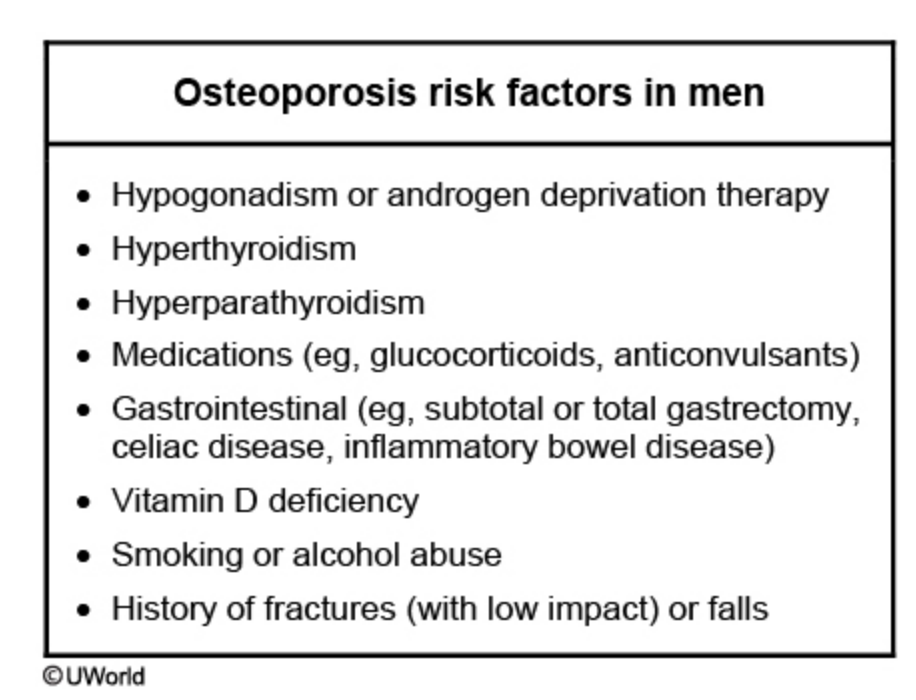
Although men have a lower incidence of osteoporosis compared to women, they are still at risk. Common osteoporosis risk factors in men are shown in the table. Hypogonadism is the best known risk factor as it increases bone turnover and decreases bone density. Congenital hypogonadism can be due to conditions such as Klinefelter syndrome or cryptorchidism.
Acquired hypogonadism is usually due to organic disorders (eg, mumps, cirrhosis, chronic renal failure, HIV), localized radiation, androgen deprivation therapy (eg, leuprolide), or surgical orchiectomy. Androgen deprivation therapy can decrease bone mineral density within 6-9 months of starting the drug. Osteoporotic skeletal fractures occur in up to 20% of men within 5 years of starting androgen deprivation therapy. Therefore, all patients on hypogonadism-inducing agents should take daily calcium (1200 mg) and oral vitamin D therapy for osteoporosis prevention.
Routine osteoporosis screening in men is controversial. Most guidelines do not recommend routine screening unless men have the risk factors shown in the table.
Testosterone therapy is usually recommended for patients with symptomatic hypogonadism, osteoporosis, and no contraindications to testosterone therapy. Pharmacologic therapy (eg, bisphosphonates) is recommended as first-line treatment for men with osteoporosis (T-score < -2.5 or fragility fracture) and no symptomatic hypogonadism or for hypogonadal men with contraindications to testosterone therapy.
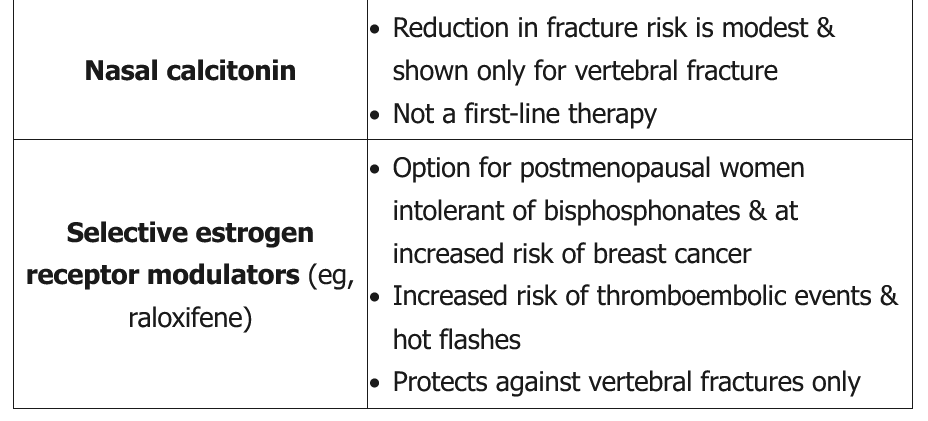
Alternative treatments
Antiresorptive therapy is appropriate for postmenopausal women with:
- Osteoporosis on DXA (T-score ≤−2.5)
- Low trauma hip or vertebral fracture (as in this patient)
- Osteopenia (T-score between −1 and −2.5) and a 10-year probability of hip fracture ≥3% or major osteoporotic fracture ≥20%
Most patients are treated with a bisphosphonate (eg, alendronate, risedronate). However, these medications are cleared by the kidneys and are relatively contraindicated in patients with chronic kidney disease (CKD) and creatinine clearance <30-35 mL/min.
Denosumab is a human monoclonal antibody that inhibits the interaction between RANK and RANK ligand, thereby blocking osteoclast formation. It decreases bone resorption, increases bone mass, and reduces the risk of vertebral, nonvertebral, and hip fracture in postmenopausal women with osteoporosis. It is appropriate for use in patients with CKD; however, calcium levels must be monitored during treatment due to increased risk of hypocalcemia in these patients.
Calcitonin may be used to decrease back pain in patients with acute vertebral fracture. However, it has minimal efficacy in fracture prevention.
Teriparatide is a recombinant human parathyroid hormone analog that can increase bone formation and reduce fracture risk. However, it is not recommended as a first-line drug unless osteoporosis is severe (T-score ≤−2.5 with fragility fracture) and is not well studied in patients with CKD.