osteomyelitis
- related: MSK
- tags:#note
Wong D, Holtom P, Spellberg B. Osteomyelitis Complicating Sacral Pressure Ulcers: Whether or Not to Treat With Antibiotic Therapy. Clin Infect Dis. 2019;68(2):338–342. Doi:10.1093/cid/ciy559
This patient with sickle cell disease (SCD) has fever, focal bone pain, and elevated inflammatory markers (eg, C-reactive protein >8 mg/L [2 mg/dL]), after mild trauma. The etiology is likely osteomyelitis, a bone infection that is most commonly spread hematogenously in children. Initial diagnostic testing should include complete blood count, C-reactive protein, erythrocyte sedimentation rate, and blood culture. X-rays should be obtained to evaluate for alternate causes of pain and the late finding of periosteal reaction/elevation seen in osteomyelitis. MRI has excellent sensitivity for osteomyelitis if the diagnosis is unclear.
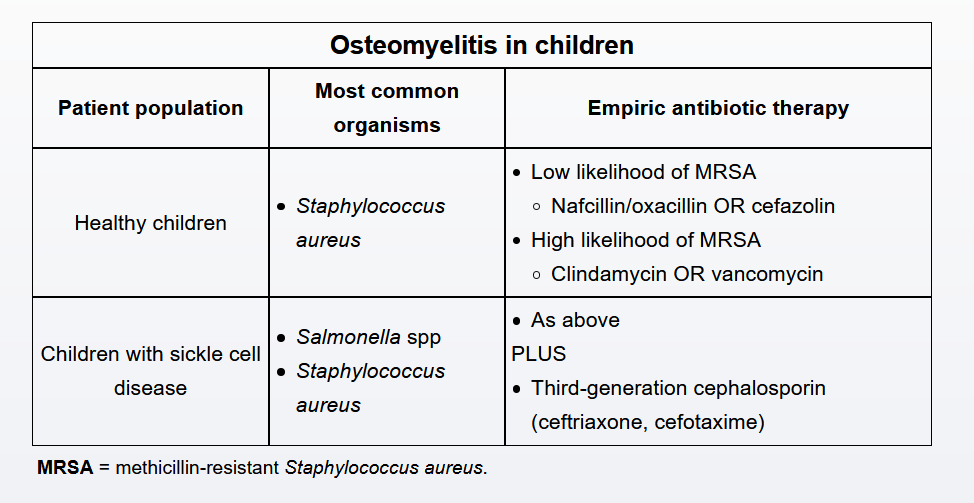
The most common etiology is the gram-positive cocci Staphylococcus aureus, including methicillin-resistant S aureus (MRSA). However, this patient's history of SCD raises his risk of osteomyelitis due to gram-negative organisms, including Salmonella. Patients with SCD have functional asplenia due to repeated splenic microinfarctions, rendering vulnerability to encapsulated organisms.
Empiric antibiotic therapy should therefore include gram-positive coverage with nafcillin, oxacillin, or cefazolin if rates of MRSA are low or clindamycin or vancomycin if MRSA is suspected. In addition, this patient's history of SCD necessitates additional treatment with a third-generation cephalosporin (eg, ceftriaxone, cefotaxime) for gram-negative coverage. Antibiotic therapy should begin promptly after initial laboratory studies are drawn to reduce the risk of further morbidity and mortality.