Hyperbilirubinemia
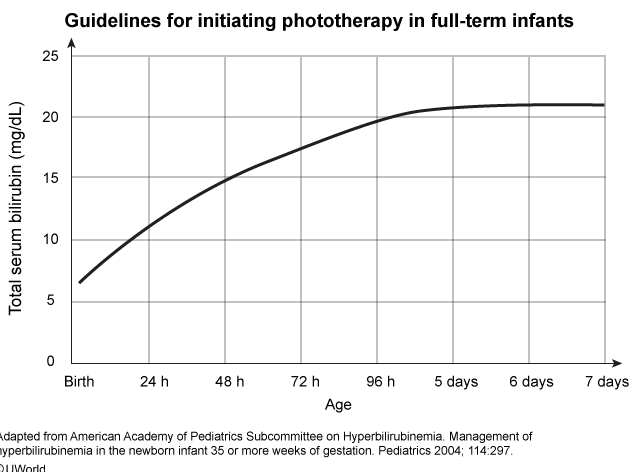
Bilirubin levels in newborns are physiologically elevated due to liver immaturity, lack of intestinal bacteria to break down bilirubin, and high hemoglobin turnover. This infant has pathologic unconjugated hyperbilirubinemia, likely caused by increased red blood cell turnover from a cephalohematoma. Additional risk factors in developing hyperbilirubinemia include prematurity (<37 weeks gestation), exclusive breastfeeding, sibling requiring phototherapy, and East Asian race. The danger of very high bilirubin levels (>20-25 mg/dL) is kernicterus, or bilirubin encephalopathy, which results in severe neurologic dysfunction (eg, movement disorder, sensorineural hearing loss). The above nomogram for full-term infants helps to determine the need for phototherapy based on bilirubin level at a given hour of life.
Phototherapy converts bilirubin into a water-soluble form that can be readily excreted in the urine and stool. As bilirubin levels physiologically rise at this age of life, a stable bilirubin level under phototherapy is not immediately considered a failed intervention and phototherapy should continue with interval bilirubin monitoring. Although formula supplementation can improve hydration and hyperbilirubinemia, stopping therapy (Choices B and E) would be inappropriate as the bilirubin level is still above the level of threshold for treatment. Additionally, although direct sunlight can lower bilirubin levels, it is not recommended in place of phototherapy due to sunburn risk.
Exchange transfusion removes bilirubin and replaces the majority of an infant's red blood cells. It is indicated if phototherapy has been ineffective (eg, rapidly rising bilirubin) or if bilirubin levels are already at toxic levels.