Psychiatry
- schizophrenia
- catatonia
- PTSD
- adjustment disorder
- parkinsons
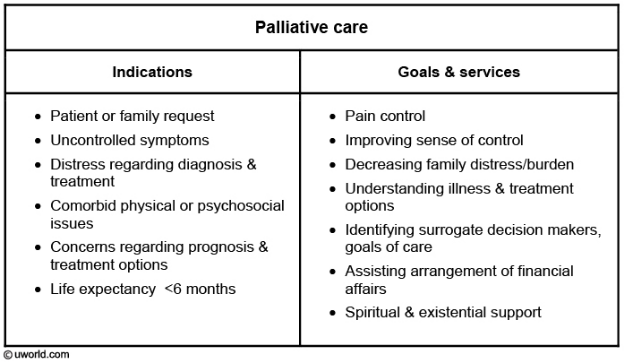
- palliative care
- second generation antipsychotics do not treat negative symptoms
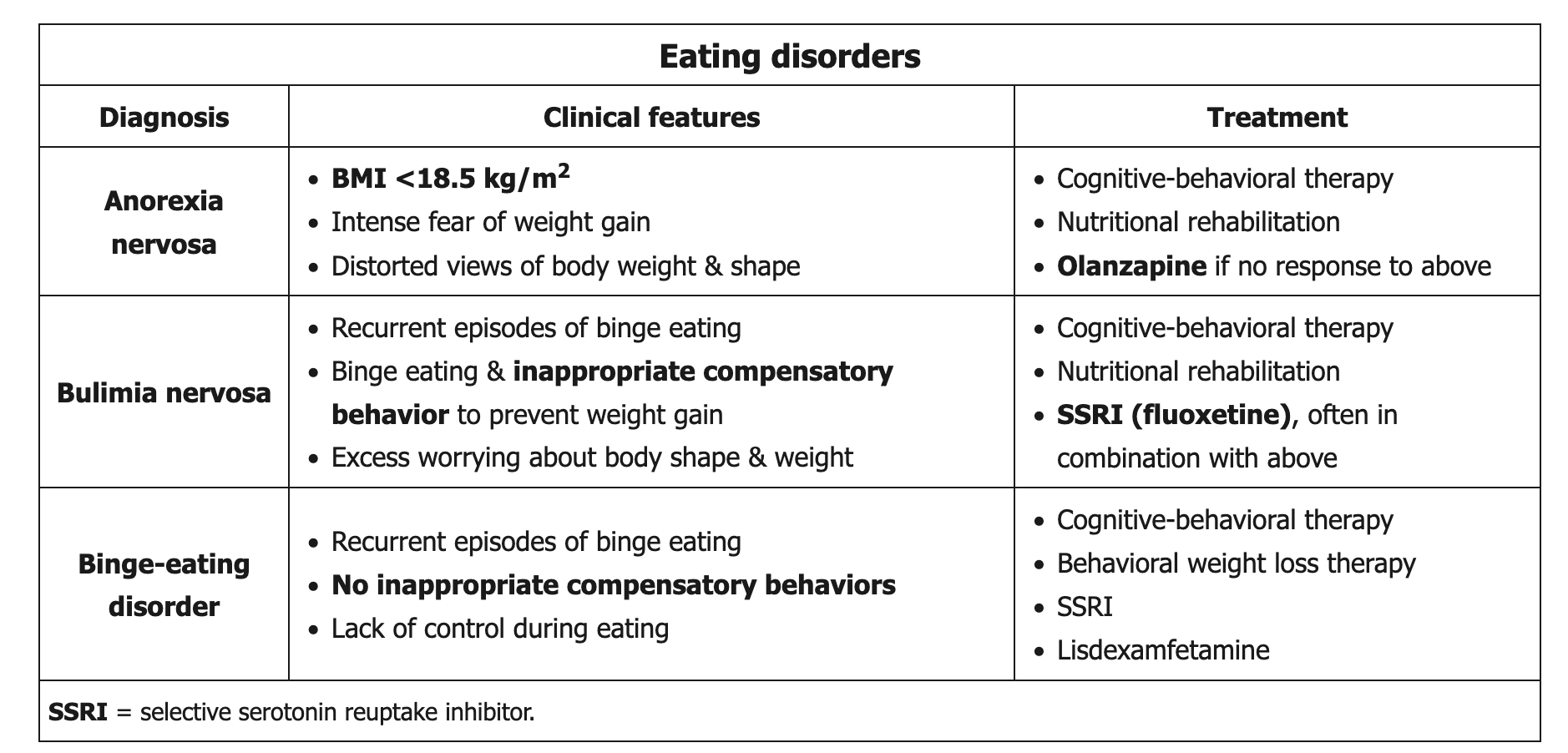
- anorexia and bulimia nervosa
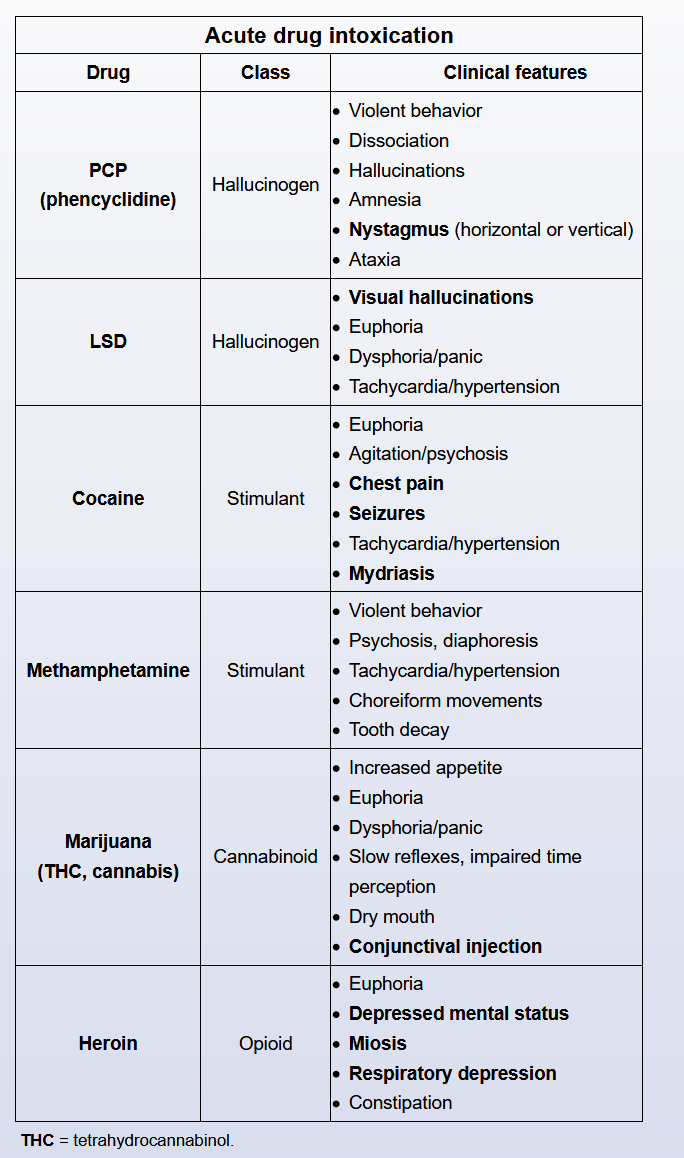
- methamphetammine use
- drug intoxications
- do not start antidepressant monotherapy in bipolar
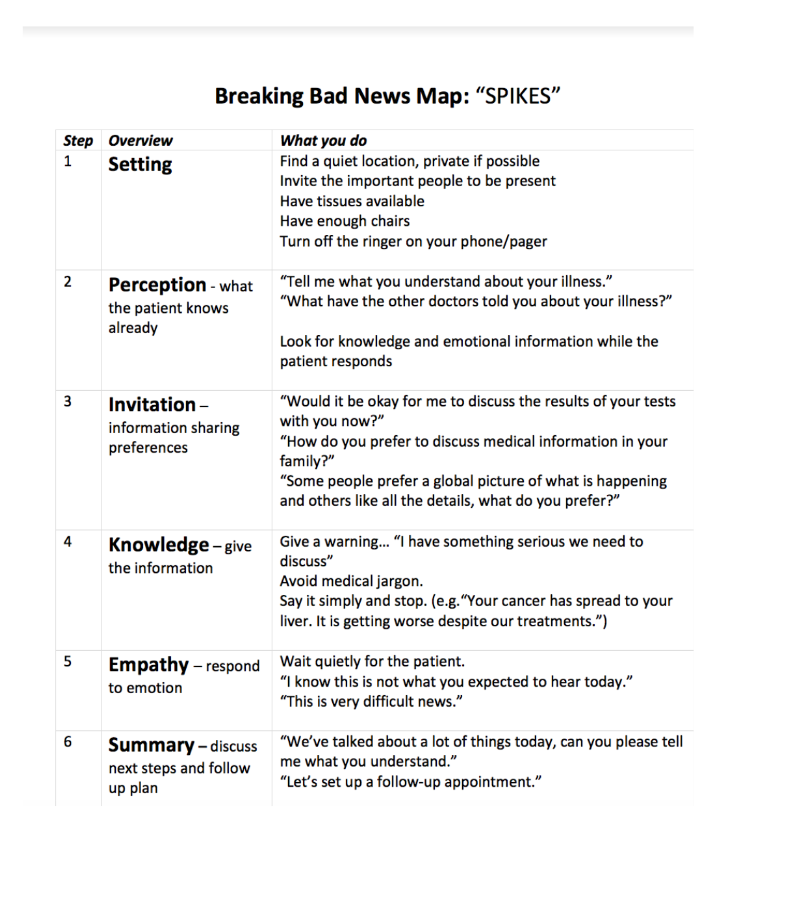
- SPIKES
- depression and anxiety 12 2020 notes
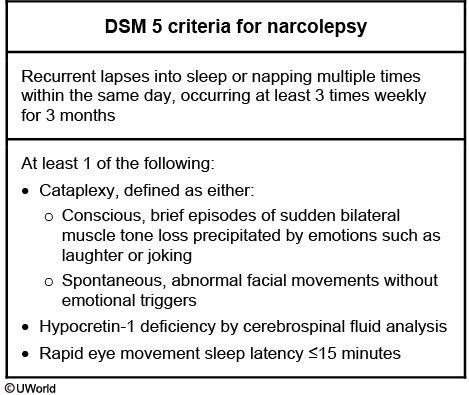
- narcolepsy
- treat end of life depression with methylphenidate
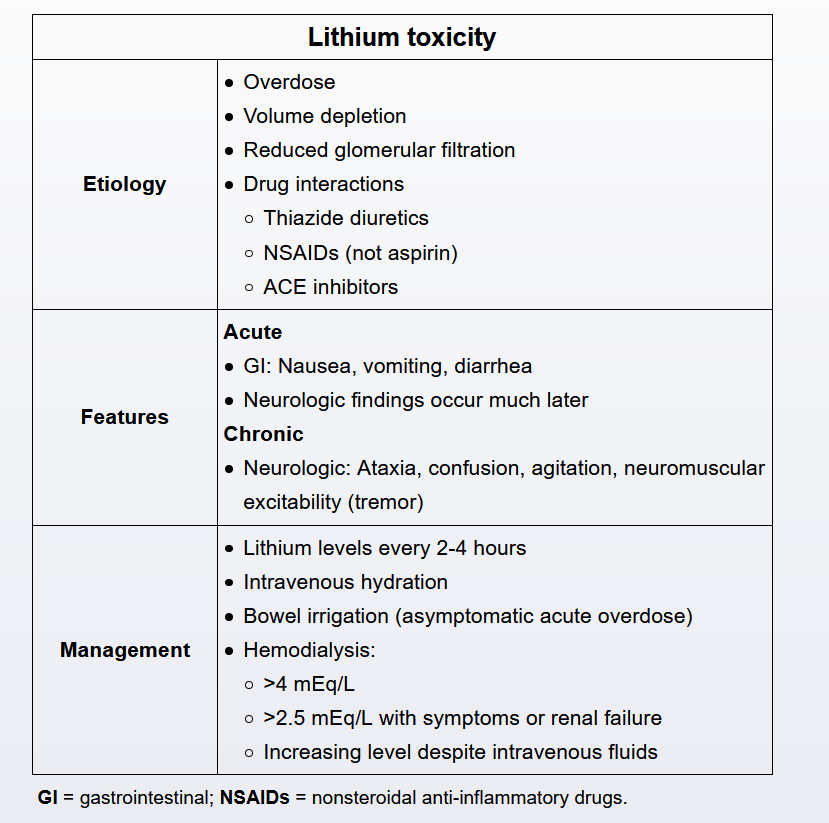
- lithium toxicity
Personality Disorders
Histrionic and borderline
- Pattern of excessive emotionality & attention-seeking behavior since early adulthood
- Inappropriate, sexually seductive or provocative behavior; uses appearance to draw attention
- Shallow, shifting, dramatic emotions
- Impressionistic, vague speech
- Suggestible (easily influenced)
- Considers relationships more intimate than they really are
This patient's vague description of symptoms, use of appearance to attract attention, dramatic but shallow and shifting emotions regarding the romantic breakup, and continued inappropriate familiarity and seductive behavior toward the physician are suggestive of histrionic personality disorder. Patients with histrionic personality disorder exhibit excessive emotionality and may attempt to manipulate the physician-patient relationship through seduction and dramatic descriptions of new symptoms at each visit. This patient's eagerness to move on to more exciting romantic opportunities and disappointment after not receiving attention are also characteristic of this disorder. Histrionic personality disorder should be differentiated from borderline, dependent, and narcissistic personality disorders, but these can also co-occur.
Individuals with borderline personality disorder can also exhibit attention seeking, manipulative behavior, and rapidly shifting emotions. However, this patient does not exhibit self-injurious and suicidal behavior, intense anger, chronic feelings of emptiness, and identity disturbance, which would be expected in borderline personality disorder.
Steroids
This patient's new onset of mood symptoms is most likely due to corticosteroid use. High doses of prednisone (>40 mg/day), often given for allergic, inflammatory, or autoimmune conditions (such as systemic lupus erythematosis), may cause psychiatric symptoms in a dose-dependent fashion, with or without any history of underlying psychiatric disorders. Longer duration of use can increase the risk; however, psychiatric symptoms secondary to corticosteroids may begin at any time during the course of treatment. Corticosteroid-induced psychiatric symptoms are more common in women than in men. In addition to mood symptoms, psychosis and anxiety can also occur. Other neuropsychiatric symptoms seen in patients taking glucocorticoids include sleep disturbances, restlessness, and memory loss.
Whenever possible, the first step in the treatment of corticosteroid-induced psychiatric symptoms is dose reduction (or discontinuation if appropriate) of the offending medication. Once the corticosteroid has been reduced, then psychiatric symptoms can be treated if they persist.
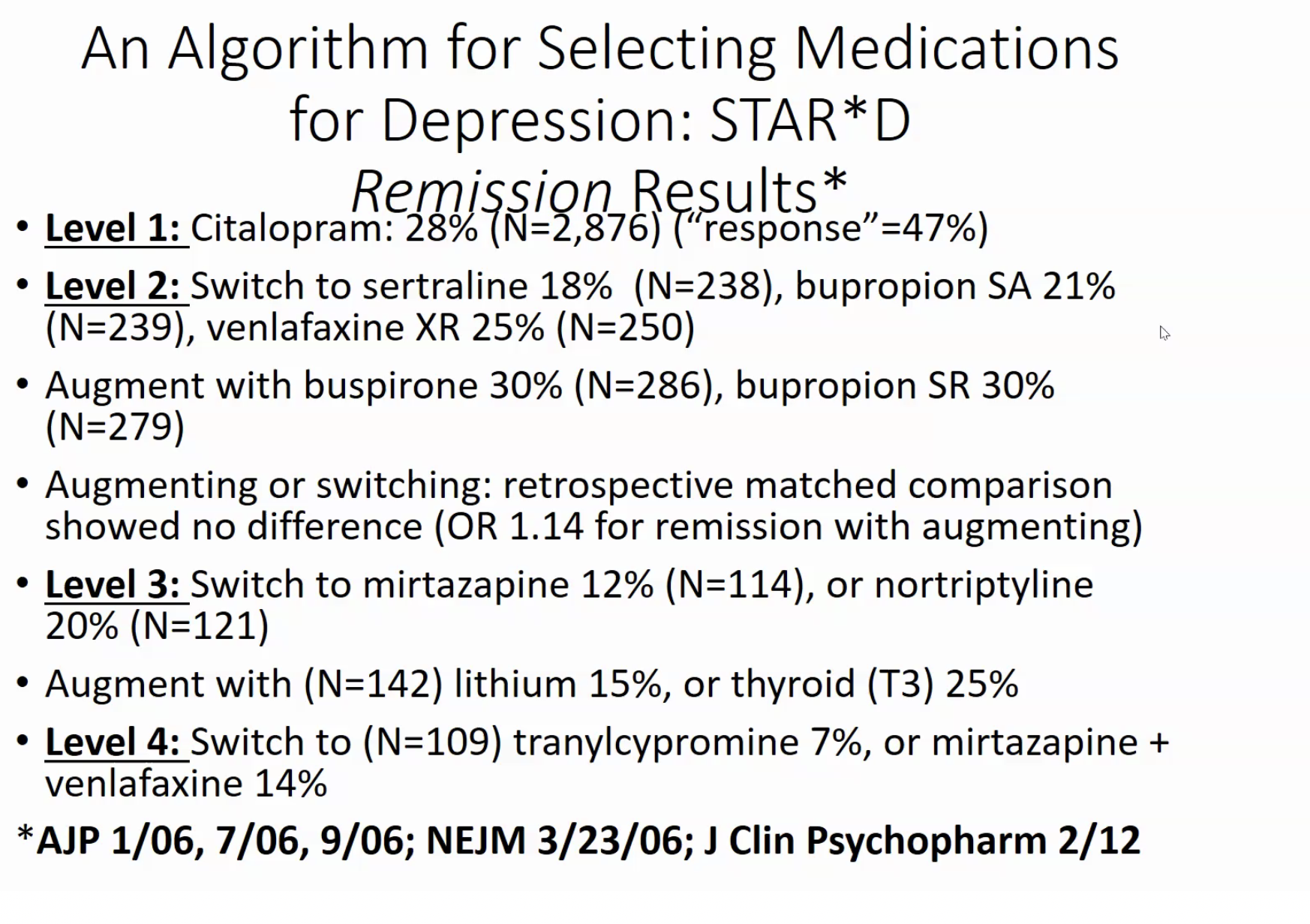
MDD
This patient has a first episode of major depression that has responded to acute treatment with citalopram. To reduce the risk of depressive relapse, guidelines recommend that patients with a single episode of major depressive disorder should continue antidepressant treatment for approximately 6 months following acute response (referred to as "continuation phase treatment"). The dosage that achieved response should be maintained and not reduced (ie, the dose that gets the patient well keeps the patient well) (Choice A).
Patients with a history of multiple episodes (recurrent major depressive disorder), chronic episodes (≥2 years), strong family history, or severe episodes (eg, suicide attempt) should be considered for maintenance treatment. This typically involves continuing antidepressant medication for 1-3 years following remission to reduce the risk of recurrence (Choice D). Patients with a history of highly recurrent (eg, ≥3 lifetime episodes) and very severe, chronic major depressive episodes may need to continue maintenance treatment indefinitely.
Randomized, controlled trials support the use of lithium as either monotherapy or augmentation in preventing suicide. Its protective effect may result from treating or preventing mood episodes and/or decreasing impulsivity and aggression.
Therapies
Exposure and response prevention therapy, a specific form of cognitive-behavioral therapy (CBT), is considered first-line psychotherapy for OCD. Exposure and response prevention therapy involves gradual and repetitive exposure to anxiety-provoking stimuli that produce obsessional thoughts (eg, contamination fears), followed by prevention of performing the associated compulsion or ritual (eg, compulsive cleaning, repetitive showers).
Dialectical behavioral therapy is a form of CBT developed for the treatment of borderline personality disorder.
Interpersonal psychotherapy focuses on improving dysfunctional relationships and interpersonal functioning. It is used primarily in the treatment of depressive disorders.
Psychodynamic psychotherapy, which traces problems back to their origins in childhood, may provide the patient with insight but is not effective in changing the compulsive behaviors seen in OCD.
Acute Grief
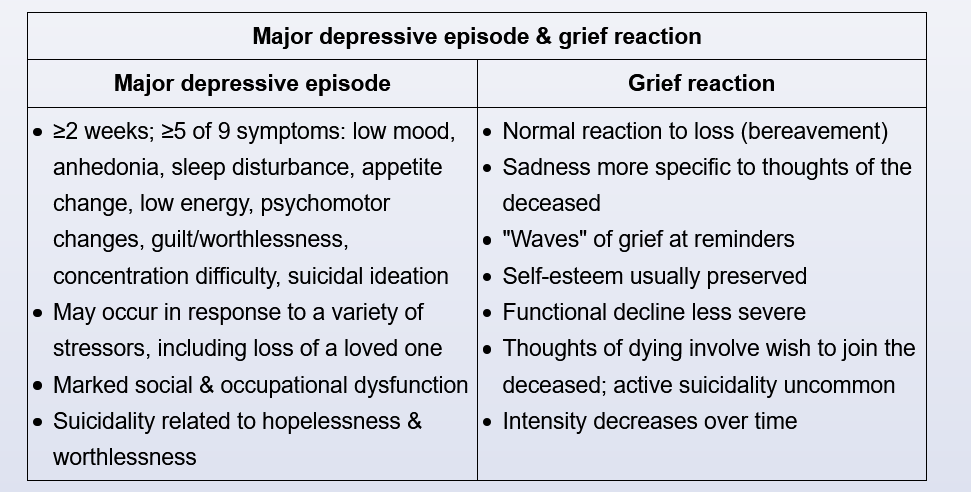
This patient's tearfulness, insomnia, poor appetite, weight loss, hallucinations of her recently deceased husband, and wish that she had died instead are consistent with normal grief. Acute grief shares many symptoms with major depression (eg, sadness, anhedonia, sleep and appetite disturbance, impaired concentration), but the sadness is less persistent and does not involve low self-esteem, excessive guilt, or active suicidal ideation. Management of acute grief includes expressing empathy, education about the range of typical grief symptoms, and monitoring. Patients without mental disorders should be reassured that transient hallucinations are also consistent with acute grief and are not psychotic.
The patient's transient hallucinations and illusions are part of normal grief and do not require treatment with an antipsychotic.
Uncomplicated acute grief does not require treatment and is generally managed with support from family, friends, and clergy. Benzodiazepines have not been shown to be helpful and are not recommended (Choice B). Psychotherapy is generally unnecessary and should not be routinely offered (Choice C). For patients with insomnia, a behavioral approach (eg, sleep hygiene) is the recommended initial intervention. Hypnotic medications are reserved for patients unresponsive to behavioral interventions.