-
AKI
AKI
- related: Nephrology
- tags: #note
- AKI is either oliguric or nonoliguric
- prerenal AKI: responds to fluids
- ATN = AKI + one of following
- not responding to fluids
- labs: UNa, FENA, casts
- Contrast AKI happens more often with 2 hits, contrast + one of following
- nsaids
- ckd
- ace/arb
- diabetes
- CKD-epi calculator is better than Cr or GFR alone
-
Medicine
Medicine
Todos
- tolearn
- MKSAP todos
- heart murmurs
Organ Systems
- Allergy and Immunology
- Rheumatology
- Cardiology
- Dermatology
- Endocrine
- ENT
- GI
- Hemeonc
- ID
- MSK
- Nephrology
- Urology
- Neurology
- Pulmonology
- Podiatry
Subject Areas
- General
- Biostats
- Psychiatry
- [[Geriatric
-
Analgesic Nephropathy
analgesic nephropathy
- related: Nephrology
- cause: nsaid medications
- pathology: reversible decline in renal blood flow and GFR due to PGE inhibition. Can result in AIN
- sx: increased Cr and decreased GFR
- dx
- AIN: biopsy showing minimal change, typical interstitial inflammatory pattern
This patient most likely has analgesic-induced nephropathy. Analgesic-induced nephropathy can present with florid
-
Interstitial Cystitis
interstitial cystitis
- related: UTI, Nephrology
- tags: #nephrology
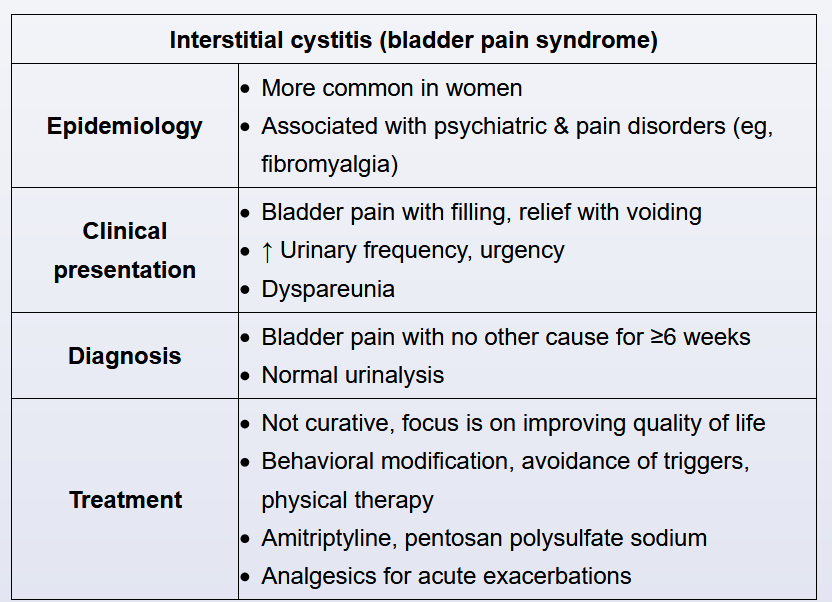
Interstitial cystitis (also known as painful bladder syndrome) is a chronic, painful bladder condition of uncertain etiology. The pelvic pain in interstitial cystitis is classically exacerbated by bladder filling and relieved by voiding. The onset of the symptoms is typically gradual, and the symptoms wors
-
Nephrotic Syndrome
nephrotic syndrome
- related: Nephrology
- tags: #nephrology
Patients with severe nephrotic syndrome are predisposed to thrombotic events. One possible mechanism for hypercoagulability is loss of natural anticoagulants in the urine. Thromboses occur most commonly in the renal veins and deep veins of the lower extremities. Chronic renal vein thrombi are usually asymptomatic. (Acute renal vein thrombi oft
-
RTA
RTA
- related: nephrology
- tags: #nephrology
Type 1 RTA
- pt: sjogren, RA, kid, amphotericin B
- cause: distal tubule cannot excrete H or absorb K
- sx:
- recurrent bilateral stones
- rickets disease
- growth failure in children
- dx:
- non AG metabolic acidosis but high urine pH (can't excrete H)
- acidosis increases Ca excretion (stones)
- hypokalemia (can't absorb K)
- hyperchloremia
- positive urine AG
- rx: Na bicarb
Type 2 RTA
- pt
- c
-
Calcium Renal Stones
calcium renal stones
- related: Nephrology, kidney stones
- tags: #nephrology
Potassium citrate
In addition to increasing fluid intake, potassium citrate is appropriate to prevent future calcium oxalate stones in this patient. Patients with chronic diarrhea and malabsorption are at increased risk for forming calcium oxalate stones for three reasons. First, because of the diarrhea and concomitant metabolic acidosis, urine citrate, an inhibitor
-
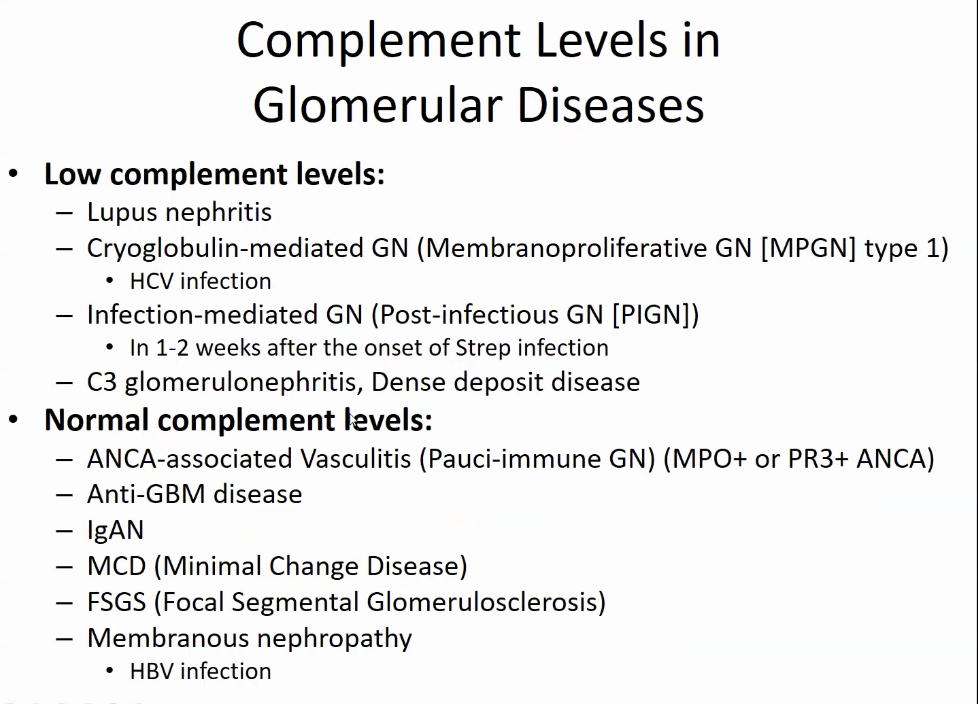
Nephrology Glomerular Disease 2 10
nephrology glomerular disease 2 10
- related: Nephrology
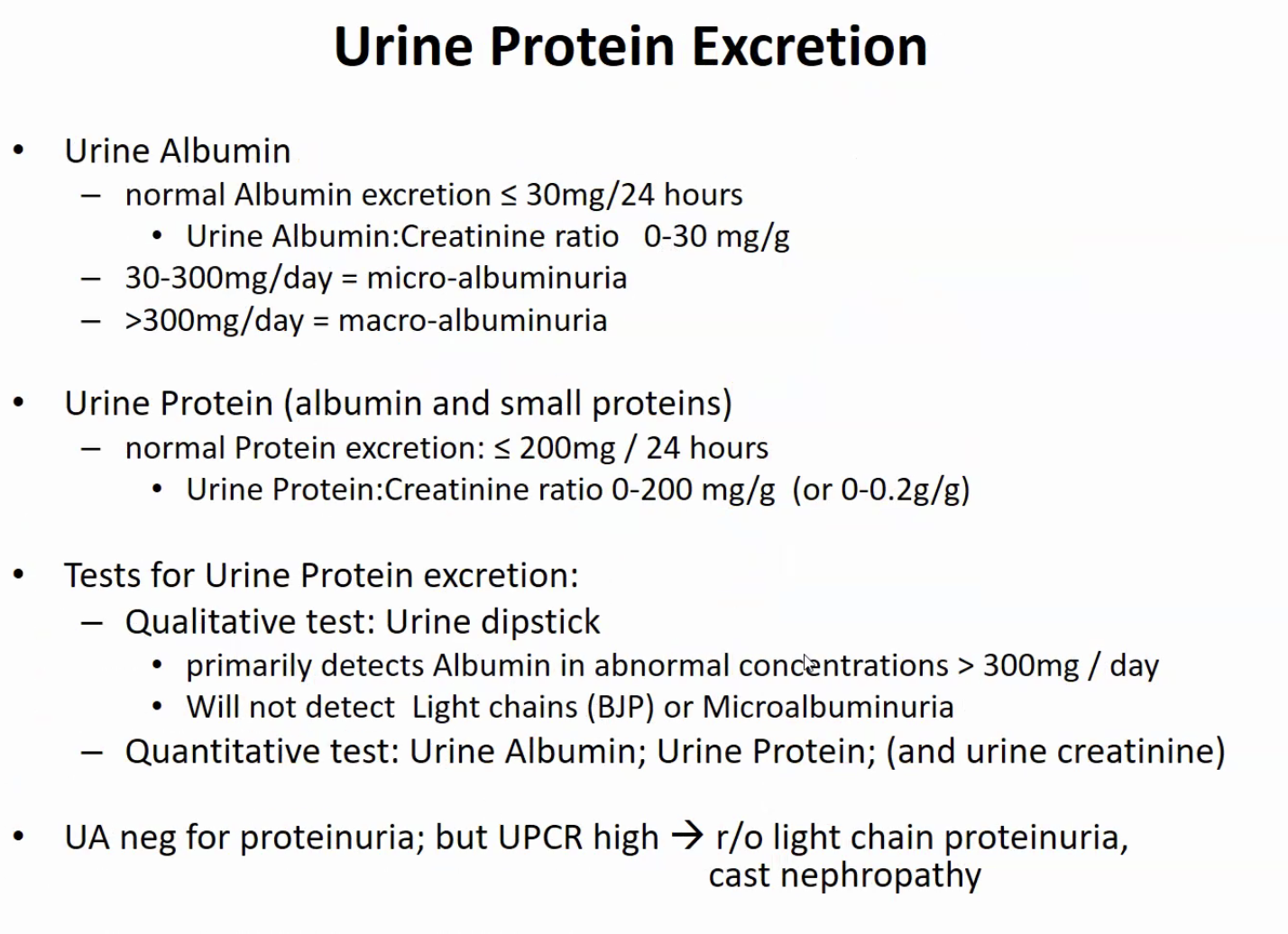
- MM: urine dipstick negative but abnormal UPC
Glomerular disease
- nephritic
- nephrotic
- RPGN
-
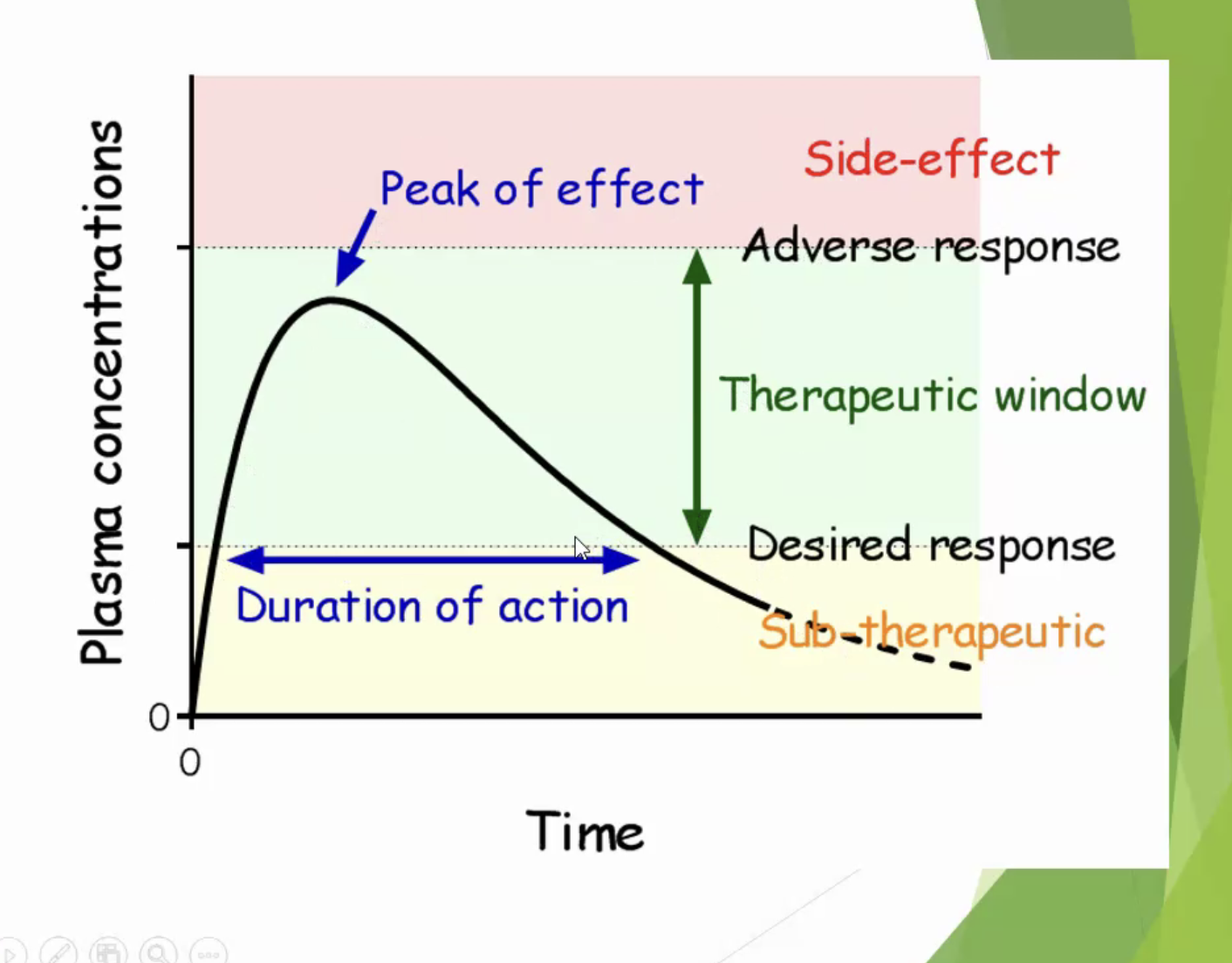
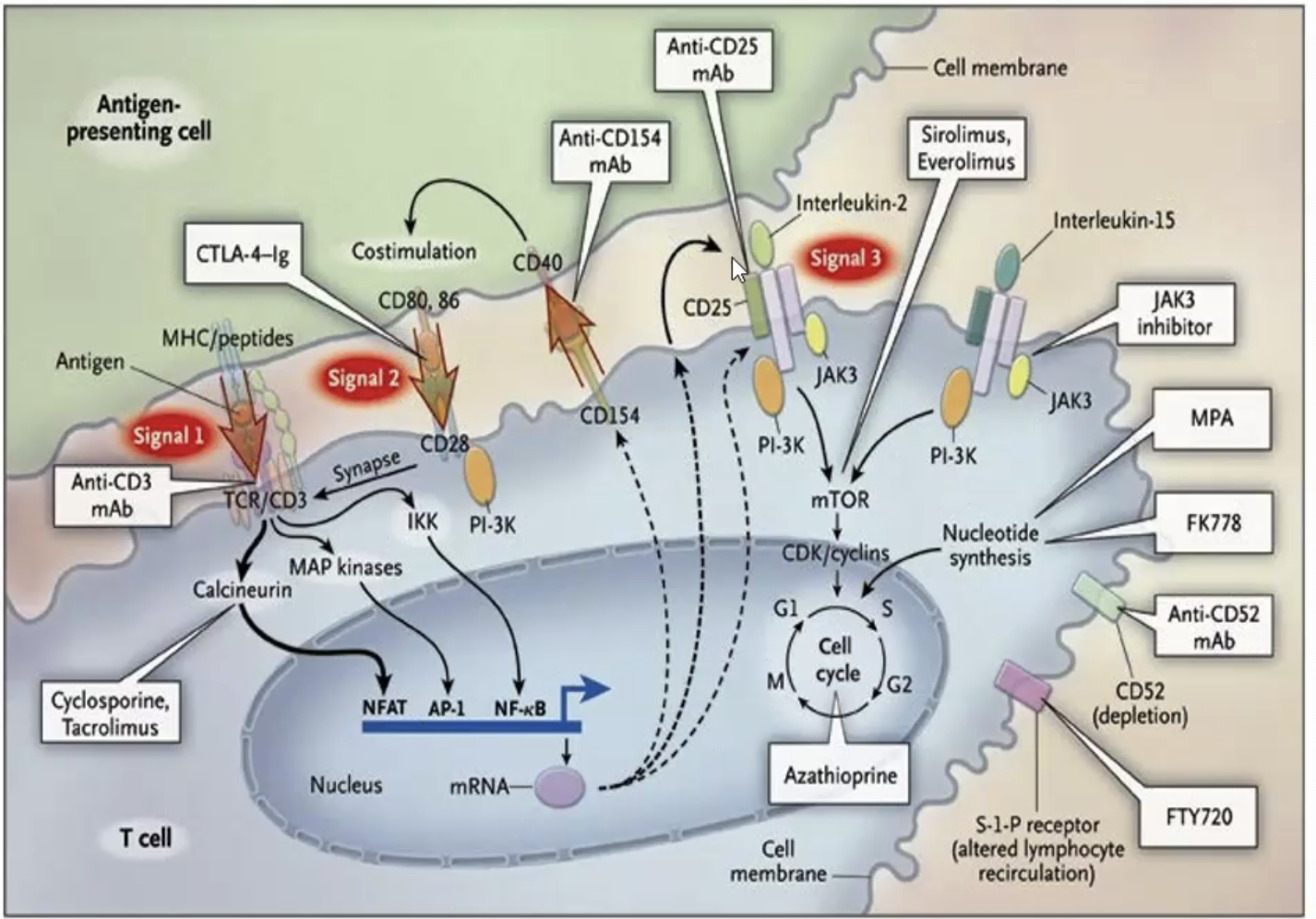
Nephrology Transplant Lecture 2 10
nephrology transplant lecture 2 10
- related: Nephrology
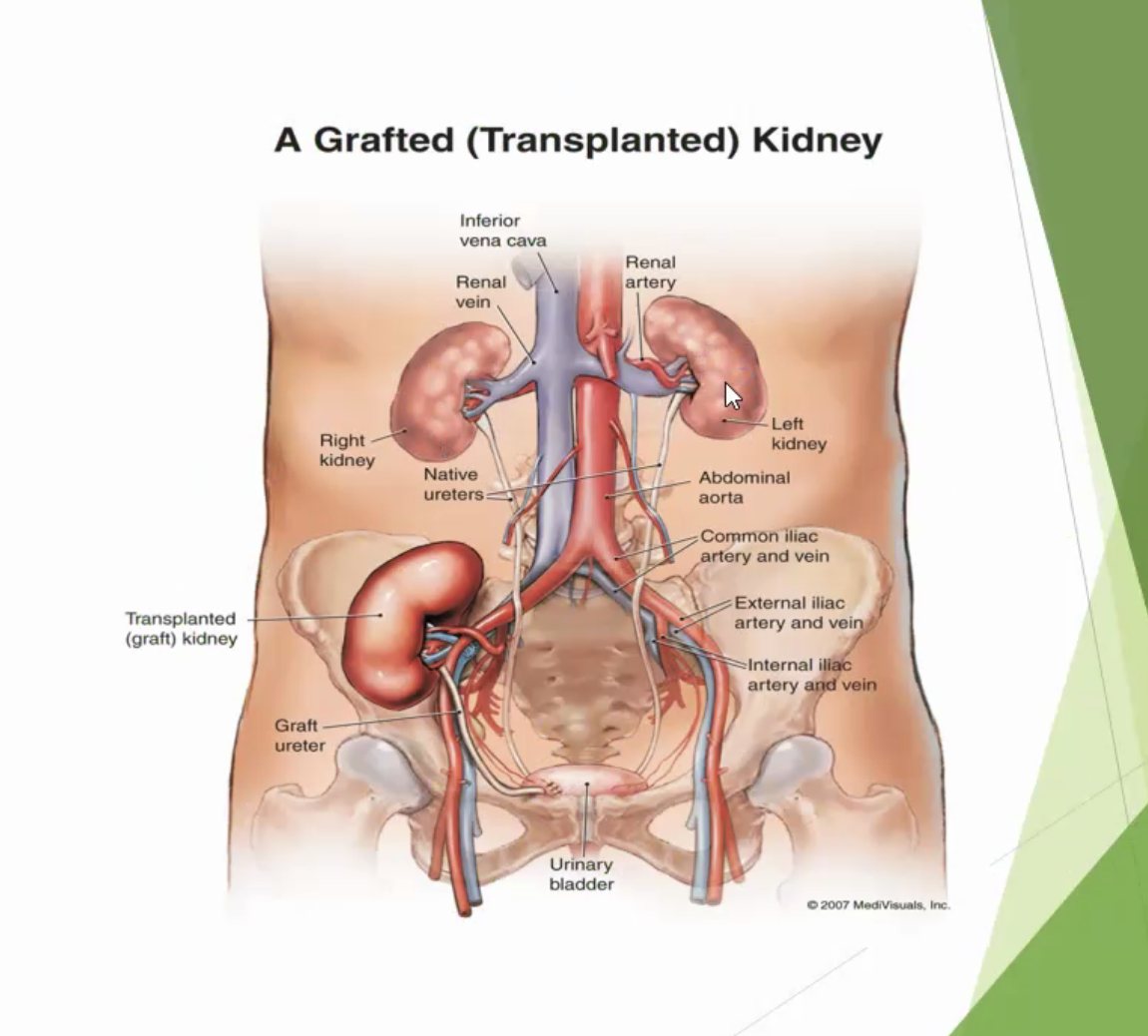
kidney placed in abdomen, on to iliac artery
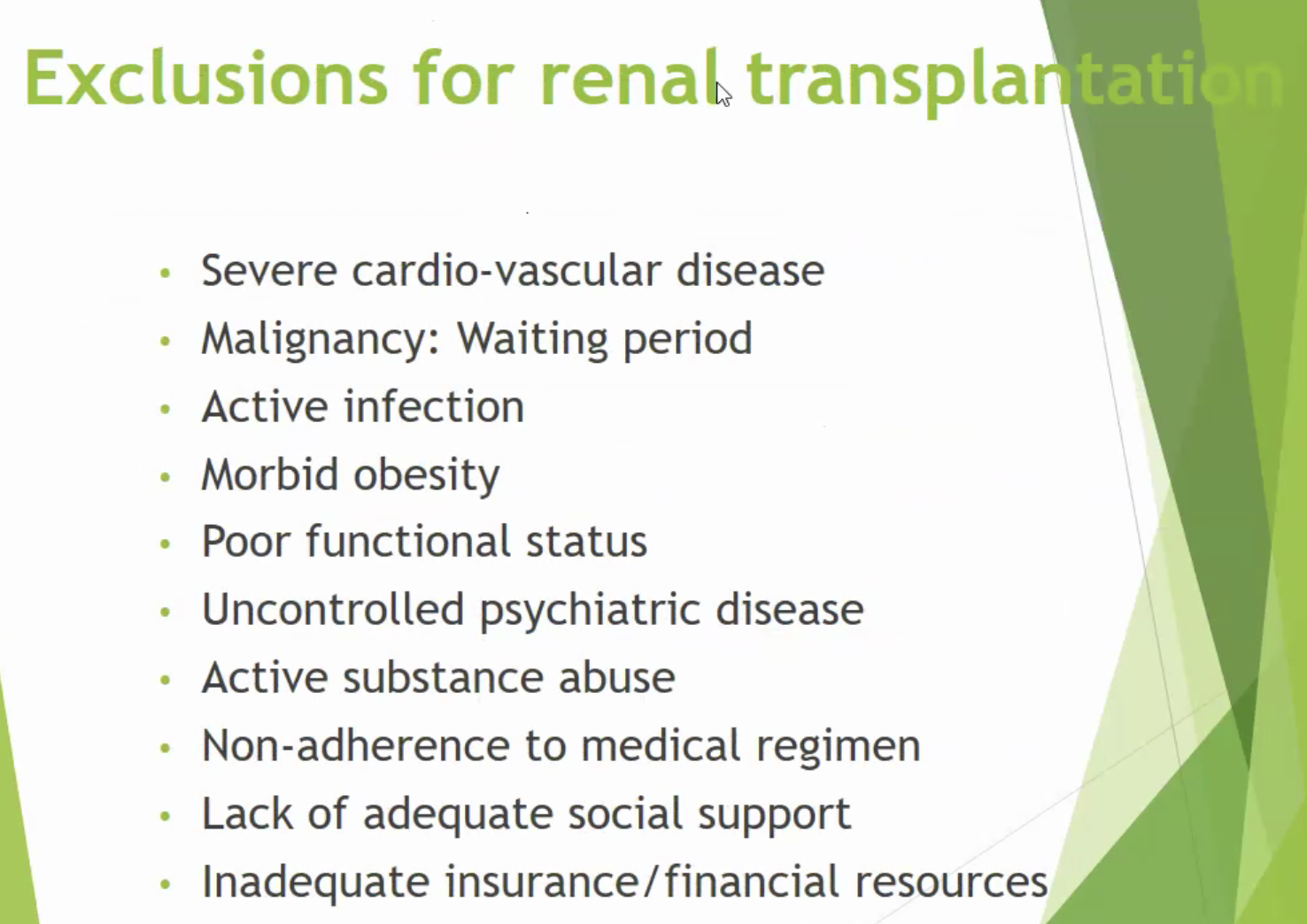
Exclusion criteria:
Immunosuppression
-
Nephrology Urinalysis Lecture 2 10
nephrology urinalysis lecture 2 10
- related: Nephrology
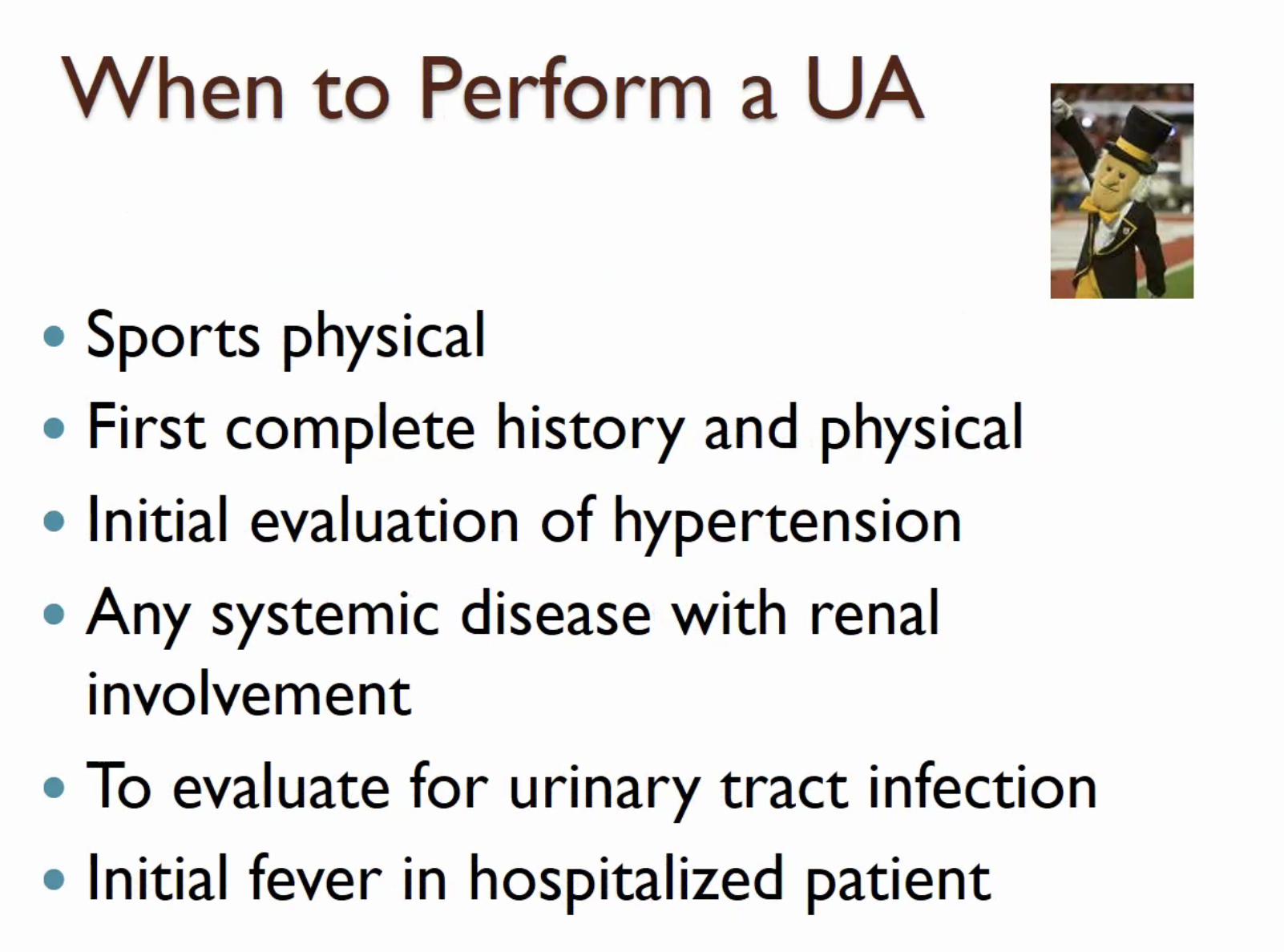
- best collected first morning void (most concentrated and acidic)
UA components
- specific gravity: how concentrated urine is
- water: 1.000
- concentrated urine >1.02
- very concentrated >1.04
- Heme
-
- in hemolysis, rhabdo from myoglobin, rbc from hematuria
-
- Protein
- small amount of urine protein can be from tubule <3g/day
-
AKI Note 2 24
AKI note 2 24
- related: Nephrology
Definition
- KDIGO criteria
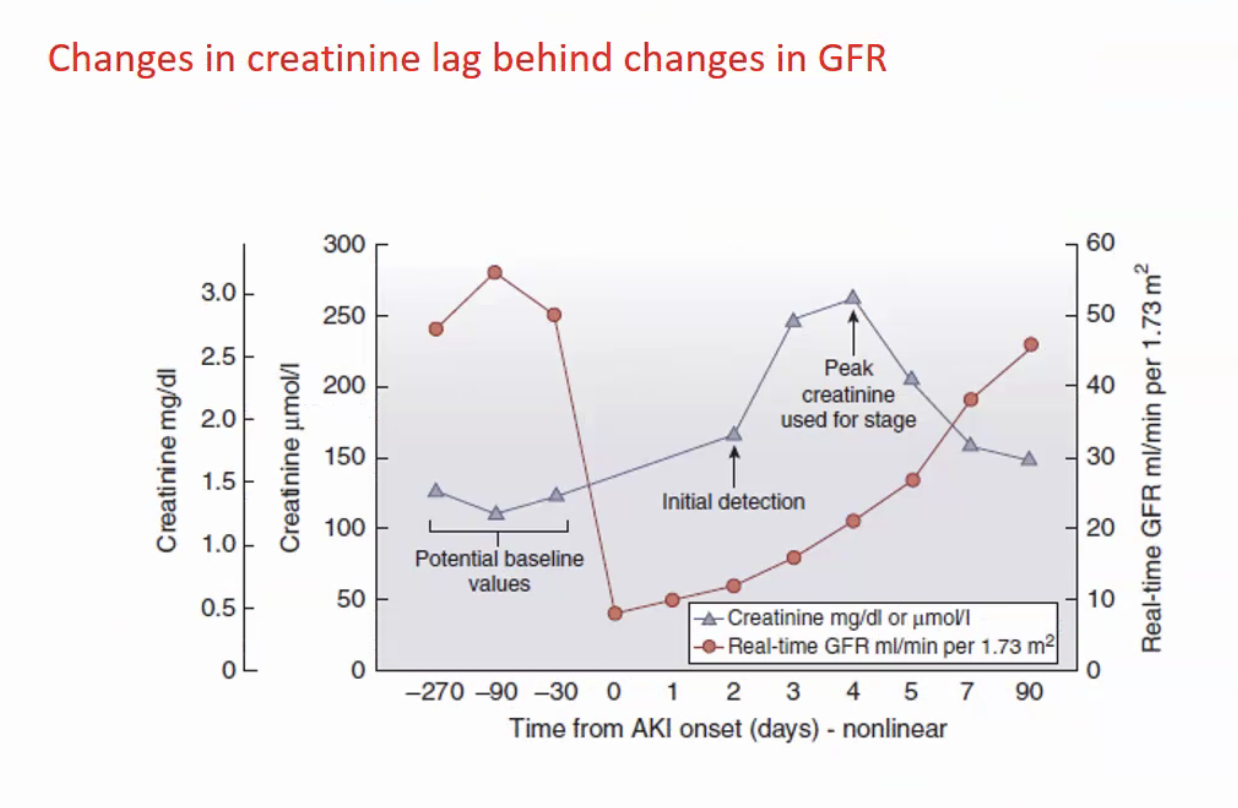
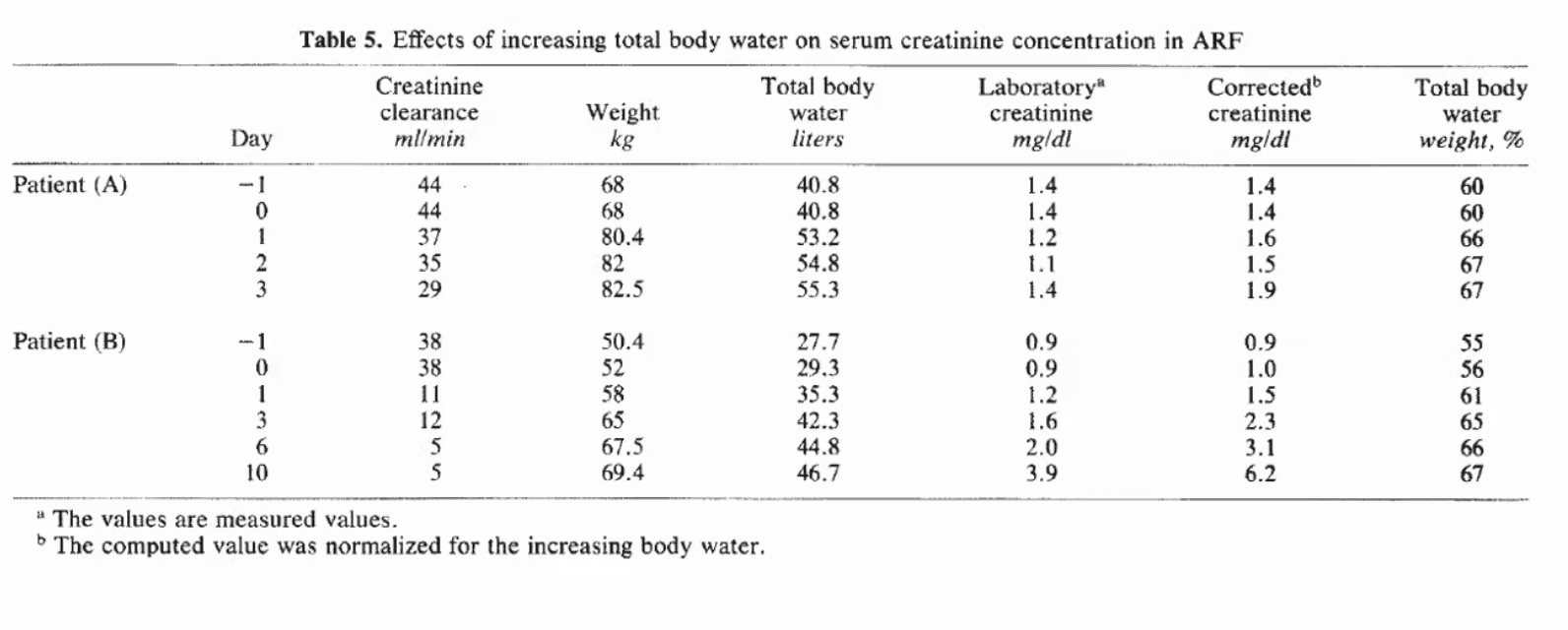
- creatinine can be affected by medication, secretion, muscle mass
- generation of creatinine lower in septic states
- volume resuscitation can dull change in GFR
Causes
- Sepsis: most common cause in ICU
- cardiac surgery: 2nd most common cause
- acute
-
CKD
CKD
- related: Nephrology
- PTH starts to climb up in CKD
-
900 is very high
- Can check PTH to see progressin of CKD vs AKI
-
When to Start Sevelamer
when to start sevelamer
- related: Nephrology, hyperphosphatemia
- tags: #note
- Correct Ca x phosphorus > 55
Hyperphosphatemia has been clearly shown to play a major role in the pathogenesis of secondary hyper-parathyroidism, extraosseous calcification, and increased mortality risk in hemodialysis patients. Serum phosphorus exceeding 5.5 mg/dL and calcium phosphate product (Ca × P) over 52 mg2/dL2 each correlate with increased mortality risk in dial
-
CARE Study
CARE study
- related: Nephrology, hyperphosphatemia, when to start sevelamer
- tags: #note
CARE study: https://www.kidney-international.org/article/S0085-2538(15)50372-4/pdf
-
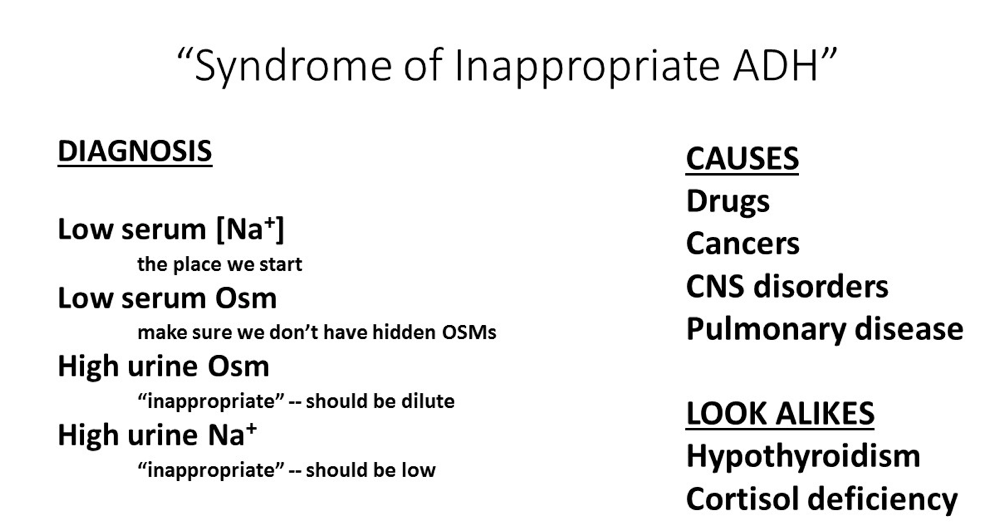
Hyponatremia
hyponatremia
- related: Nephrology, hypernatremia
- tags: #nephrology
Causes
Thiazide Induced
This patient's symptoms are most likely due to hyponatremia; an occasional, but possibly fatal complication of thiazide diuretics. Thiazide-induced hyponatremia usually occurs within 1-2 weeks after starting the drug, more commonly in older woman with low body mass index. One study showed that 36% of patients had a plasma sodium < 130 mEq/L and patient
-
Metabolic Acidosis in CKD
metabolic acidosis in CKD
- related: Nephrology
- tags: #note
Metabolic acidosis frequently occurs in patients with CKD due to defective acid excretion (resulting in reduced bicarbonate generation), most commonly due to impaired ammoniagenesis. Untreated metabolic acidosis can lead to muscle loss (due to increased muscle proteolysis) and bone loss (due to increased bone resorption and impaired bone formation). In early CKD, metabolic acidosis is typic
-
Minimal Change Glomerulopathy
minimal change glomerulopathy
- related: Nephrology
- tags: #note
An 81-year-old man is hospitalized for an acute onset of edema in his legs and abdomen. History is significant for chronic back pain, for which he takes daily ibuprofen. He has no other symptoms.
On physical examination, vital signs are normal. There is no rash. Cardiac examination is without extra sounds or murmurs, and the estimated central venous pressure is normal. The lungs are clear on exami
-
IgA Nephropathy
IgA nephropathy
- related: Nephrology
- tags: #nephrology
The glomerulonephritides with granular immunofluorescence microscopy staining patterns all fall under the umbrella category of immune complex–mediated glomerulonephritis, with antigen-antibody complexes depositing in the kidney at various locations and in various patterns (see Table 18). Immune complex deposition activates the classic
-
MGUS in Kidney
MGUS in kidney
- related: Nephrology
- tags: #nephrology
MGRS
Monoclonal gammopathy of renal significance (MGRS) is characterized by kidney damage caused by monoclonal Ig that is secreted by a B cell or plasma cell clone not meeting diagnostic criteria for multiple myeloma or a lymphoproliferative disorder. All pathological findings associated with the clonal expansion of Ig-secreting cells can be seen in both myeloma and MGRS. The underlying pathology is
-
Diabetetic Nephropathy
diabetetic nephropathy
- related: Nephrology
- tags: #nephrology
The cornerstone of treatment of diabetic nephropathy involves glycemic control and blood pressure control. Blockade of the renin-angiotensin system with an ACE inhibitor or angiotensin receptor blocker (ARB) is recommended, typically to the maximal tolerated dose, because these agents both reduce blood pressure and levels of proteinuria, which, along with glycemic control, are the most impor
-
Kidney Stones
kidney stones
- related: Nephrology, calcium renal stones
- tags: #nephrology
Overview
Approximately 7% to 11% of the U.S. population will develop nephrolithiasis, and 50% will have recurrent disease. Risk factors for developing kidney stones include male gender, increased age, White race, obesity, diabetes mellitus, the metabolic syndrome, decreased fluid intake, chronic diarrheal states, and Roux-en-Y gastric bypass.
Clinical Manifestations
Althoug
-
Sodium and Glucose
sodium and glucose
- related: Nephrology
- tags: #nephrology
Hyperglycemia causes the osmotic translocation of water from the intracellular to the extracellular fluid compartment, which results in a decrease in the serum sodium level by approximately 1.6 to 2.0 mEq/L (1.6-2.0 mmol/L) for every 100 mg/dL (5.6 mmol/L) increase in the plasma glucose above 100 mg/dL (5.6 mmol/L). Although the patient has mild hyperglycemia, her glucose is not elevated enough to l
-
ANCA Associated Glomerulonephritis
ANCA associated glomerulonephritis
- related: Nephrology
- tags: #nephrology
Epidemiology and Pathophysiology
ANCA-associated glomerulonephritis (pauci-immune crescentic glomerulonephritis) accounts for more than half of all RPGN cases and has a particularly high prevalence in patients >65 years of age presenting with AKI and active urinary sediment. ANCA are autoantibodies that target proteins within neutrophil granules and monocyte lysosomes. There are tw
-
FSGS
FSGS
- related: Nephrology
- tags: #nephrology
Epidemiology and Pathophysiology
Focal segmental glomerulosclerosis (FSGS) is the most common form of the nephrotic syndrome in Black patients and, in certain parts of the world, has replaced membranous glomerulopathy as the leading cause of the nephrotic syndrome in White patients. The prevalence of FSGS in the United States is more than 20,000 patients, with a yearly incidence of approximately 5000 newly di
-
MPGN
MPGN
- related: Nephrology
- tags: #nephrology
Epidemiology and Pathophysiology
Membranoproliferative glomerulonephritis (MPGN) is a rare form of chronic glomerulonephritis diagnosed primarily in children and young adults. The name stems from its pattern of glomerular injury. The entity is divided into immune-complex forms of MPGN (mediated by antigen-antibody interactions triggering the classical complement pathway) versus ==complement-mediated f
-
RPGN
RPGN
- related: Nephrology
- tags: #nephrology
Rapidly Progressive Glomerulonephritis
Epidemiology and Pathophysiology
Rapidly progressive glomerulonephritis (RPGN; also known as crescentic glomerulonephritis) is not a specific disease; rather, RPGN is a clinical entity that can be caused by multiple diseases and manifests as (1) at least a 50% decline in glomerular filtration rate over a short period (usually days to weeks) with (2) pathology
-
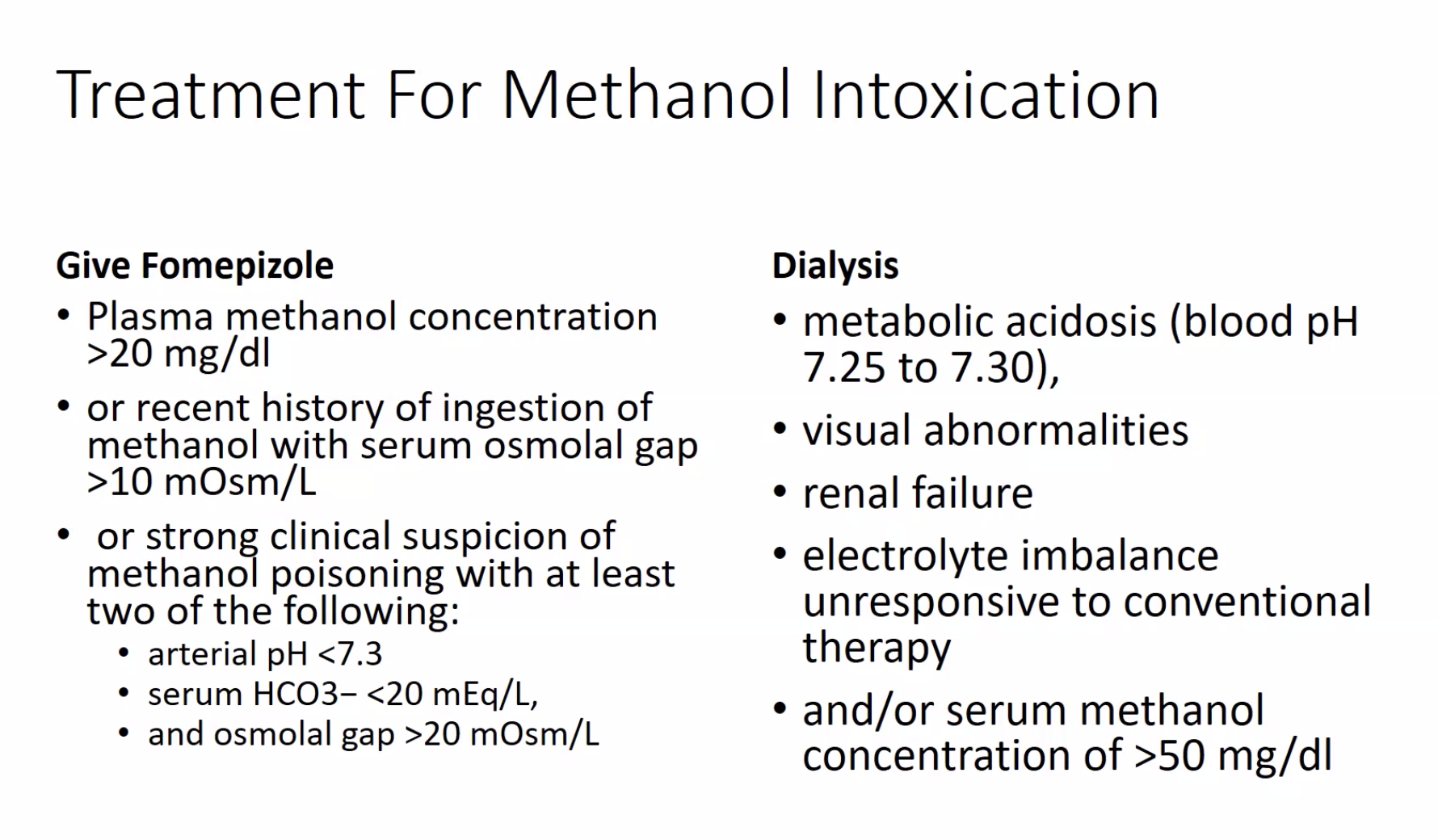
Anion Gap Metabolic Acidosis
anion gap metabolic acidosis
- related: Nephrology, nonanion gap metabolic acidosis NAGMA
- tags: #nephrology
Etiologies

CAT MUDPILES
- CO/cyanide/congenital heart failure
- aminoglycosides
- toluene (glue sniffing)/teophylline
- Methanol
- Uremia: BUN elevation
- DKA, alcoholic ketoacidosis, starvation ketoacidosis
- Paracetamol/acetaminophen, paraldehyde, [[pyroglutamic acid
-
Anti-GBM
anti-GBM
- related: Nephrology
- tags: #nephrology
Epidemiology and Pathophysiology
Anti–glomerular basement membrane (anti-GBM) antibody disease is a rare form of RPGN with an incidence of less than one case per million per year. Anti-GBM antibody disease accounts for about 20% of RPGN cases in adults. The lesion is more frequently seen in White patients and has a bimodal age and gender distribution, with peak incidences in ==young men in the second
-
Contrast Induced Nephropathy
contrast induced nephropathy
- related: Nephrology
- tags: #nephrology
Contrast-associated nephropathy (CAN), defined as an increase in serum creatinine levels within 24 to 48 hours of contrast exposure, is a common cause of reversible AKI in the hospital setting. Contrast-induced nephropathy (CIN) includes that subset of CAN in which the kidney injury can be more definitively linked to the contrast. Multiple risk factors have been associated with CAN, bu
-
Ethylene Glycol Toxicity
ethylene glycol toxicity
- related: Nephrology
- tags: #nephrology
This patient has typical findings of ethylene glycol toxicity, including central nervous system depression, an increased anion gap metabolic acidosis, and an increased plasma osmolar gap.
Because laboratory confirmation of ethylene glycol intoxication may take days, empiric therapy with fomepizole and aggressive fluid resuscitation with crystalloids (250-500 mL/h intravenous init
-
Infection Related Glomerulonephritis
infection related glomerulonephritis
- related: Nephrology
- tags: #nephrology
Epidemiology and Pathophysiology
Infection-related glomerulonephritis (IRGN) results from a recently resolved infection or an infection that is ongoing at the time of development of glomerulonephritis. IRGN is preferred to the formerly used term “postinfectious glomerulonephritis,” which adequately described classic poststreptococcal glomerulonephritis but did not address t
-
Lupus Nephritis
lupus nephritis
- related: Nephrology
- tags: #nephrology
Lupus Nephritis
See MKSAP 18 Rheumatology for more information on systemic lupus erythematosus.
Epidemiology and Pathophysiology
Kidney involvement in systemic lupus erythematosus (SLE), generally termed lupus nephritis (LN), is a major contributor to SLE-associated morbidity and mortality. Up to 50% of patients with SLE will hav
-
Membranous Glomerulopathy
membranous glomerulopathy
- related: Nephrology
- tags: #nephrology
Epidemiology and Pathophysiology
Membranous glomerulopathy (membranous nephropathy) is a leading cause of the nephrotic syndrome in White adults. Epidemiology has remained constant over the past several decades. Disease occurs at an approximate rate of 1 case per 100,000 persons per year, with a peak incidence between 30 and 50 years of age. Approximately 75% of cases are considered p
-
Rhabdomyolysis Induced AKI
rhabdomyolysis induced AKI
- related: Nephrology
- tags: #nephrology
Heme pigment released from myoglobin or hemoglobin can cause AKI through intravascular volume depletion (seen in rhabdomyolysis), renal vasoconstriction, direct proximal tubular injury, and tubular obstruction. In rhabdomyolysis, myoglobin is released in the circulation from damaged skeletal muscle. Major causes of rhabdomyolysis include ==trauma, drugs and toxins, seizures, meta
-
Abdominal Compartment Syndrome
abdominal compartment syndrome
- related: Nephrology
- tags: #nephrology
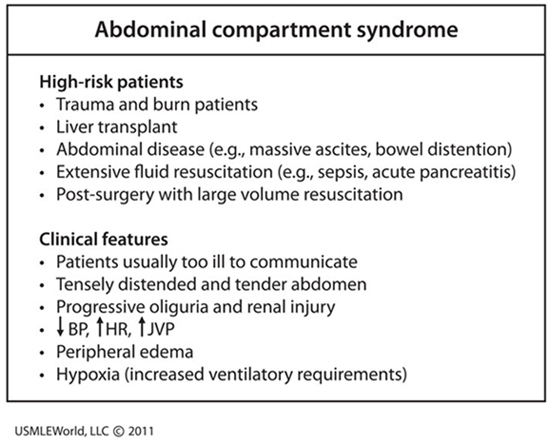
This patient’s presentation is consistent with likely intra-abdominal hypertension (IAH) causing abdominal compartment syndrome (ACS). Intra-abdominal hypertension is defined as pressure > 12 mm Hg; and ACS is defined as IAH with new organ dysfunction. Primary ACS is due to abdominal pelvic disease, whil
-
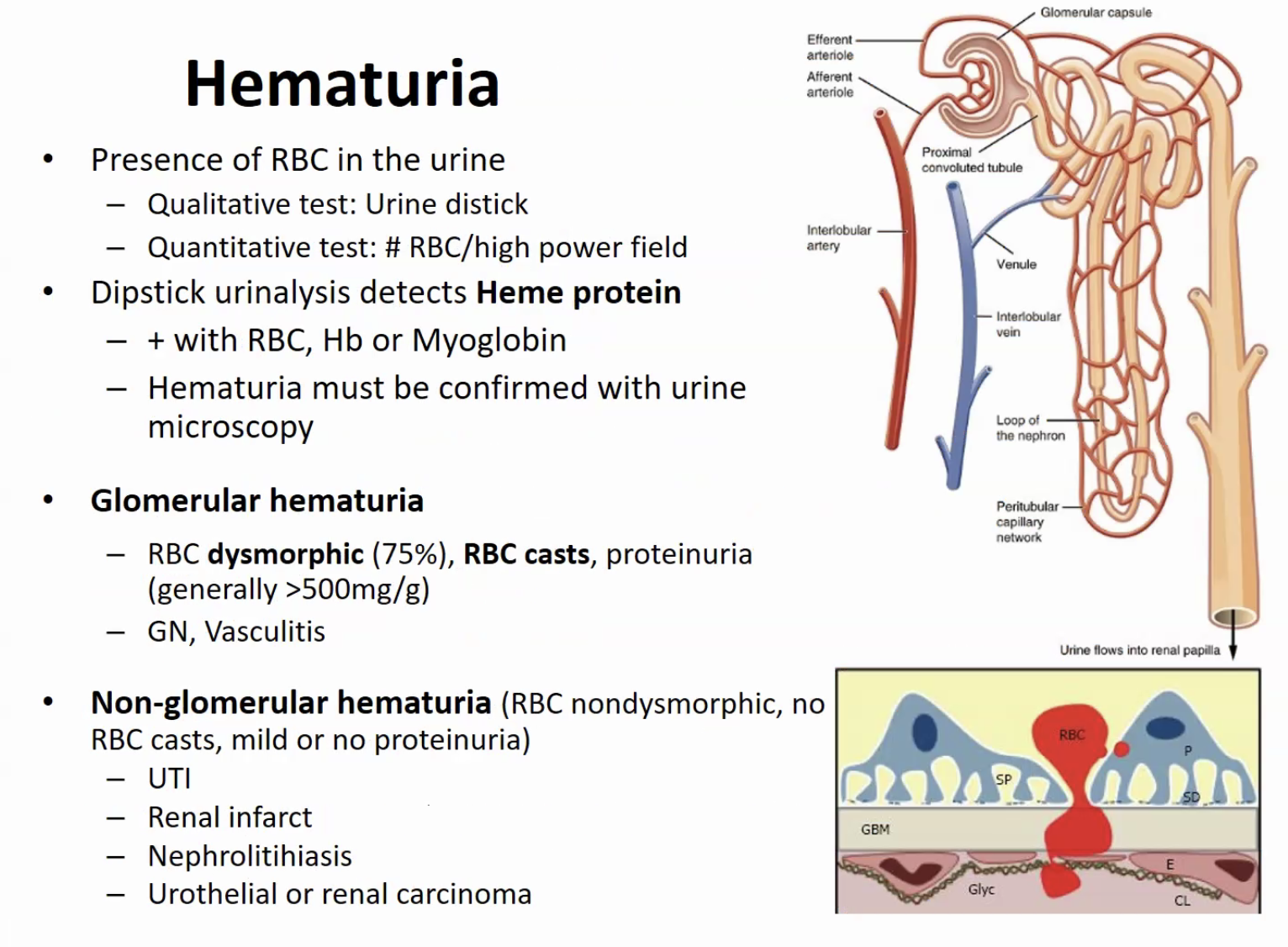
Hematuria
hematuria
- related: Nephrology
- tags: #nephrology
Hematuria is defined as the presence of >3 erythrocytes/hpf in the urine sediment and may be microscopic (detectable only on urine testing) or macroscopic (grossly visible). Hematuria is most often of nonglomerular origin. A glomerular origin is suggested by concurrent proteinuria, presence of dysmorphic erythrocytes, increased serum creatinine or decrease in estimated GFR (eGFR), or systemic signs a
-
Heparin Induced Hypoaldosteronism
heparin induced hypoaldosteronism
- related: Nephrology
- tags: #nephrology
The most likely cause of this patient's elevated serum potassium level is heparin. Hypoaldosteronism caused by heparin, inhibitors of the renin-angiotensin system, type 4 renal tubular acidosis, or primary adrenal disease can cause hyperkalemia. Both unfractionated and low-molecular-weight heparin use is associated with a decrease in aldosterone synthesis. This occurs more frequently in p
-
Peritoneal Dialysis
peritoneal dialysis
- related: Nephrology, sbp
- tags: #nephrology
Peritoneal dialysis utilizes an indwelling catheter to perform exchanges of dialysate with a specified solute concentration and osmolality into the peritoneum, which serves as a semipermeable membrane and allows for diffusion of solutes and osmosis of water. Dialysate needs to be exchanged about three to five times per day to maintain a high concentration gradient and maintain adequate solute
-
Pyroglutamic Acidosis
pyroglutamic acidosis
- related: Nephrology
- tags: #nephrology
The most likely diagnosis is pyroglutamic acidosis. Pyroglutamic acidosis, which presents with mental status changes and an increased anion gap, occurs in selected patients receiving therapeutic doses of acetaminophen on a chronic basis. Susceptible patients are those with critical illness, poor nutrition, liver disease, or chronic kidney disease, as well as those on a strict vegetarian diet. In
-
Normal Renal Function
normal renal function
- related: Nephrology
- tags: #nephrology
The kidney selectively removes waste while retaining needed substrate, maintains fluid and electrolyte homeostasis, and regulates blood pH. Glomerular filtration rate (GFR) measures total nephron filtration of blood and therefore correlates closely with toxin removal and overall kidney function. Early loss of kidney function is difficult to detect because nephron loss is not initially accompanied by
-
IV Fluids
IV fluids
- related: Nephrology
- tags: #nephrology
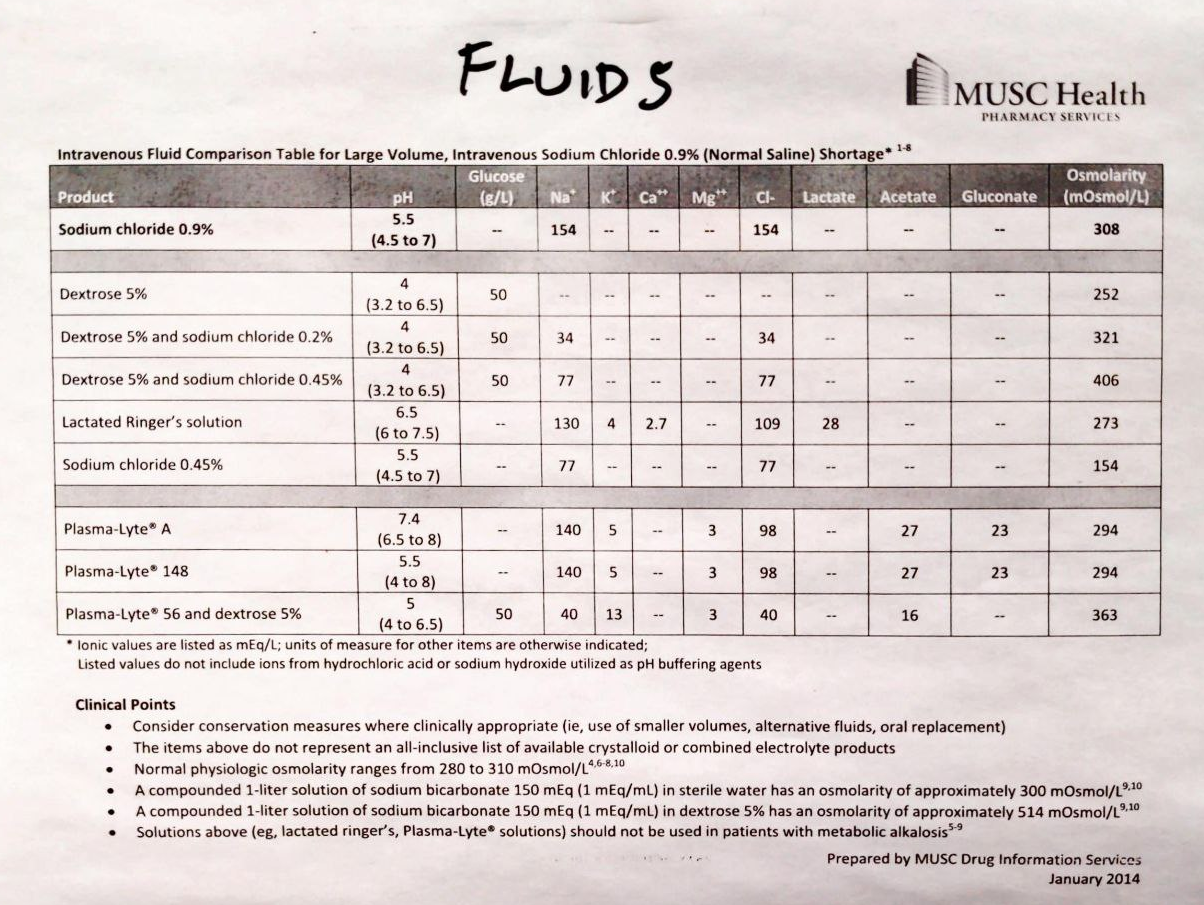
- IV bicarb can cause hypocalcemia
- D5 with Na Bicarb at 150 meQ is isotonic. Use this for acidosis with low volume
- Half NS bicarb is hypertonic
- NS: has chloride and can worsen acidemia.
- LR: has Ca
-
Immune Complex Mediated Glomerulonephritis
immune complex mediated glomerulonephritis
- related: Nephrology
- tags: #nephrology
The glomerulonephritides with granular immunofluorescence microscopy staining patterns all fall under the umbrella category of immune complex–mediated glomerulonephritis, with antigen-antibody complexes depositing in the kidney at various locations and in various patterns. Immune complex deposition activates the classic complement pathway as a co-player in glomerular inflamma
-
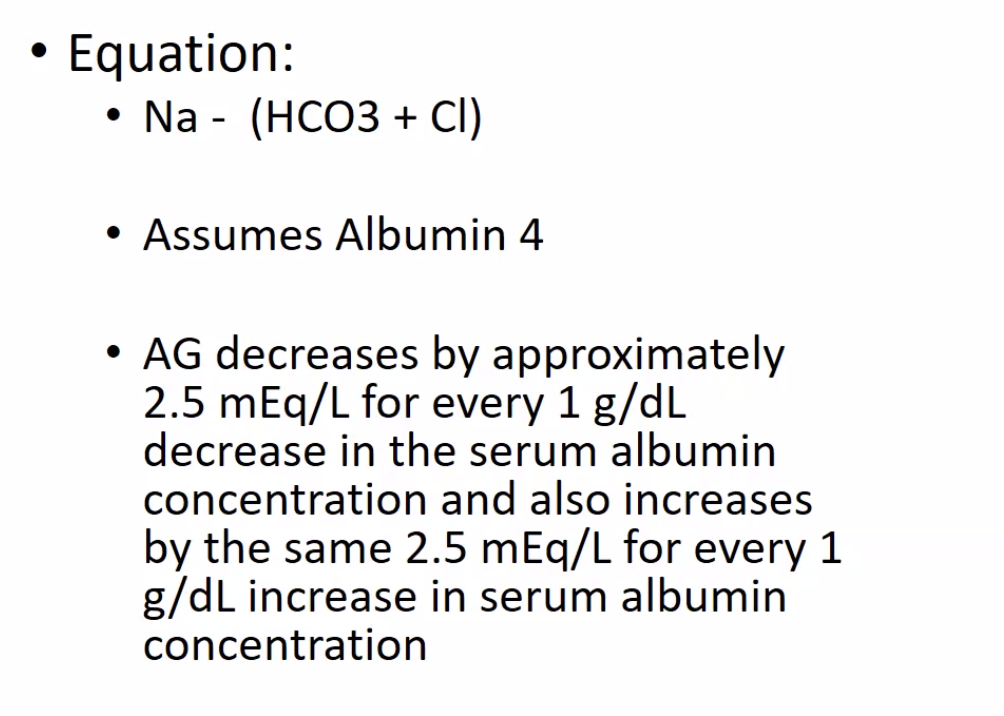
Nephrology Toxicology 1 12
nephrology toxicology 1 12
- related: Nephrology
- tags: #nephrology
AG
- assuming albumin is 4
- for every 1 drop in albumin, expected AG drops by 2.5, same with elevation
NAGMA
-
GI: diarrhea
-
GU: RTA
-
Urine AG to differentiate: Na + K - Cl
-
normal western diet: negative
-
DKA with dialysis: don't give as much fluid because not having polyuria with high glucose. Can give flui
-
Nephrology Tubulointerstitial 1 12
nephrology tubulointerstitial 1 12
- related: Nephrology
- tags: #nephrology
AIN
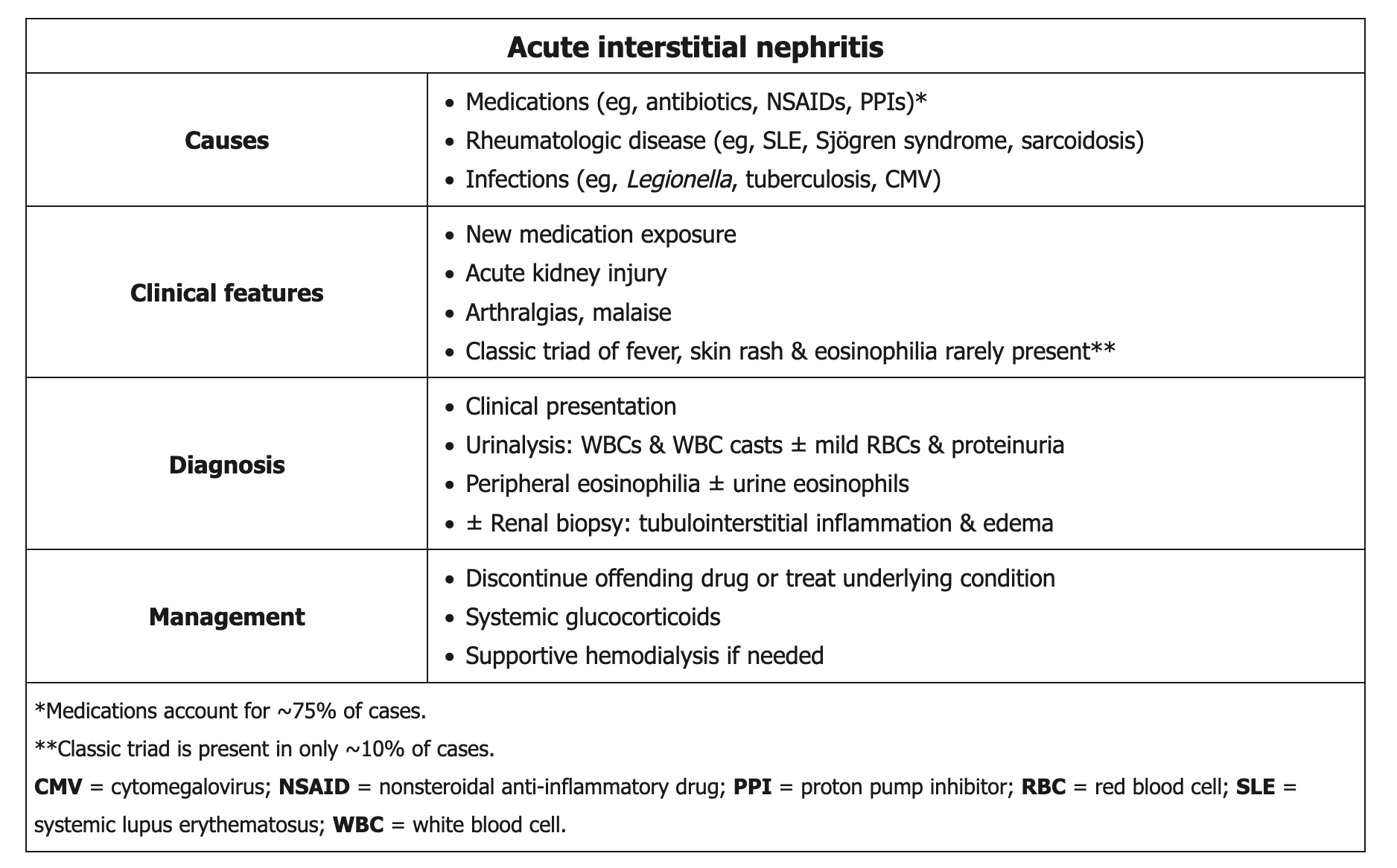
- vasculature, glomerulus spared
- causes
- allergy/drug induced: 70%
- infections: acute/chronic pyelo
- autoimmune: sjogren, lupus, sarcoid
- idiopathic
- Sx
- fever, rash, eosinophilia
- renal failure
- labs
- na wasting, acidification, normal to mildly increased proteinuria
- WBC, hyperkalemia, hyp
-
Urinalysis
urinalysis
- related: Nephrology
- tags: #nephrology
Interpretation of the Urinalysis
Urine dipstick and urine microscopy are indicated in the evaluation of both acute and chronic kidney disease. Analysis is best performed on a fresh specimen within 30 to 60 minutes of voiding. Midstream collection is preferred with a clean catch in women and uncircumcised men.
Urine Dipstick
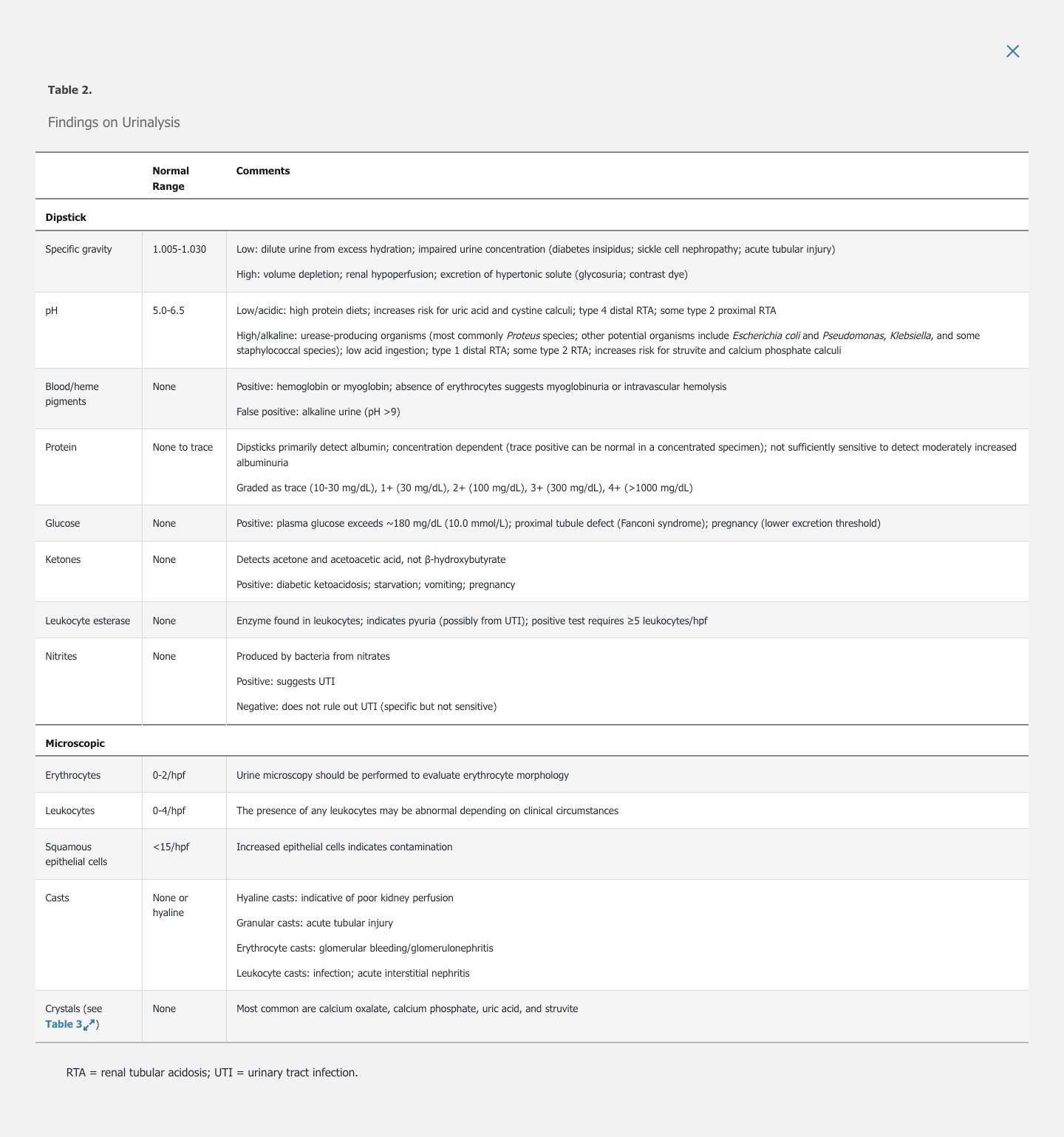
Sp
-
Methanol
Methanol
- related: Nephrology
- tags: #nephrology
Methanol
- blurry vision, abdominal pain, photophobia
- formic acid build up in brain and cause optic swelling
-
Dialysis
dialysis
- related: Nephrology
- tags: #nephrology
When to start outpatient dialysis
The optimal time to start dialysis is debated. Studies are inconclusive with some favoring late initiation of dialysis either at the onset of uremic symptoms or when the estimated glomerular filtration rate (eGFR) is <10 mL/min/1.73 m2 rather than preemptive hemodialysis initiated at eGFR of 10-15 mL/min/1.73 m2 without uremic symptoms. Regardless of the timing of dialysis
-
Hyperphosphatemia
hyperphosphatemia
- related: Nephrology, when to start sevelamer
- tags: #nephrology
Phosphate binders
Dietary restriction of phosphorus, although important, is difficult to accomplish because dialysis patients are encouraged to consume a relatively [[high protein diet]] in order to prevent protein malnutrition. Similarly, ==intermittent hemodialysis alone does not a
-
Tubulointerstitial Nephritis
tubulointerstitial nephritis
- related: Nephrology
- tags: #nephrology
Sx
- nonspecific: polyuria, malaise, anorexia, AKI
- Urine: sterile pyuria, proteinuria, hematuria
- risks:
- daily low dose ASA unlikely to cause IN
- PPI: very common
-
BUN Elevation
BUN elevation
- related: Nephrology
- tags: #nephrology
- elevated BUN can happen indoor
- GI bleed
- decadron
- TPN: amino acid infusion
- catabolic states
-
Calciphylaxis
calciphylaxis
- related: Nephrology, hypocalcemia
- tags: #nephrology
- Avoid Ca supplement in high phos When to consider
- when Ca x P > 80
Treatment
- Use sodium thiosulfate
- SE: can cause metabolic acidosis: CO2 between 15-18
- Can also use vitamin K
-
Give Hypotonic Fluid in Post ATN Diuresis
give hypotonic fluid in post ATN diuresis
- related: Nephrology
- tags: #nephrology
Avoid NS as the hypertonic NS could cause more diuresis as kidney is unable to reabsorb Na. LR is ok. Hypotonic saline such as 1/2 NS could be an option.
When in doubt, check urine osm/Na to see if patient is excreting low osm urine. Then match it with IVF.
-
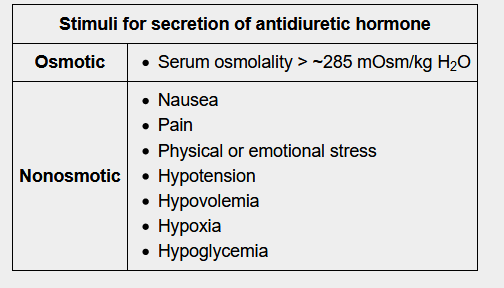
Postoperative Hyponatremia
postoperative hyponatremia
- related: Nephrology
- tags: #nephrology
This patient, who is experiencing nausea, headaches, and drowsiness following lithotripsy, has acute symptomatic hyponatremia, likely related to her recent surgery. Postoperative hyponatremia can develop within hours of surgery due to release of vasopressin related to surgical stress, the use of nonelectrolyte solutions (eg, glycine, sorbitol) for irrigation, or the infusion of hypo
-
Kidney Manifestations of Deposition Diseases
Kidney Manifestations of Deposition Diseases
- related: Nephrology
- tags: #nephrology
Overview
Various kidney diseases are associated with deposition of immunoglobulin (Ig) and non-Ig proteins. On electron microscopy, these deposits can be unstructured or organized into fibrils or tubules (Figure 14). Monoclonal Ig deposits may be caused by myeloma, Waldenström macroglobulinemia, or chr
-
Metabolic Alkalosis
metabolic alkalosis
- related: Nephrology
- tags: #nephrology
Metabolic Alkalosis
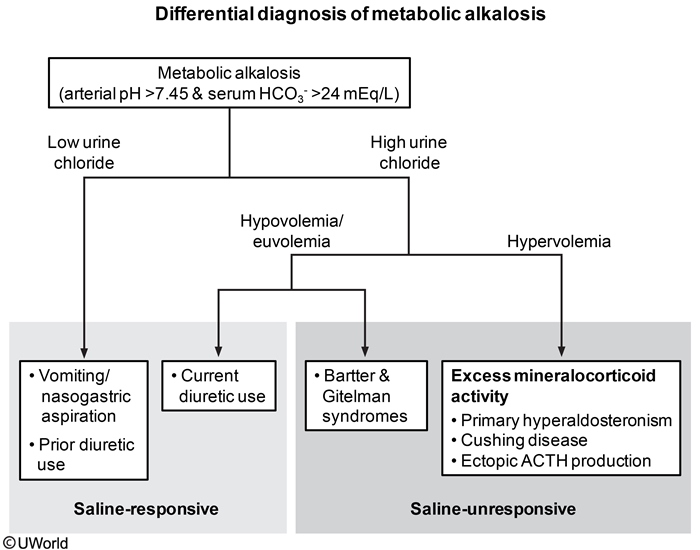
This patient's presentation is consistent with metabolic alkalosis, defined as arterial pH >7.45 and serum bicarbonate level >24 mEq/L. Metabolic alkalosis can be further classified as saline-responsive and saline-unresponsive. It can also be classified according t
-
Pickering Syndrome, Flash Pulmonary Edema in Renal Artery Stenosis
Pkcering syndrome, flash pulmonary edema in renal artery stenosis
- related: Nephrology
- tags: #nephrology
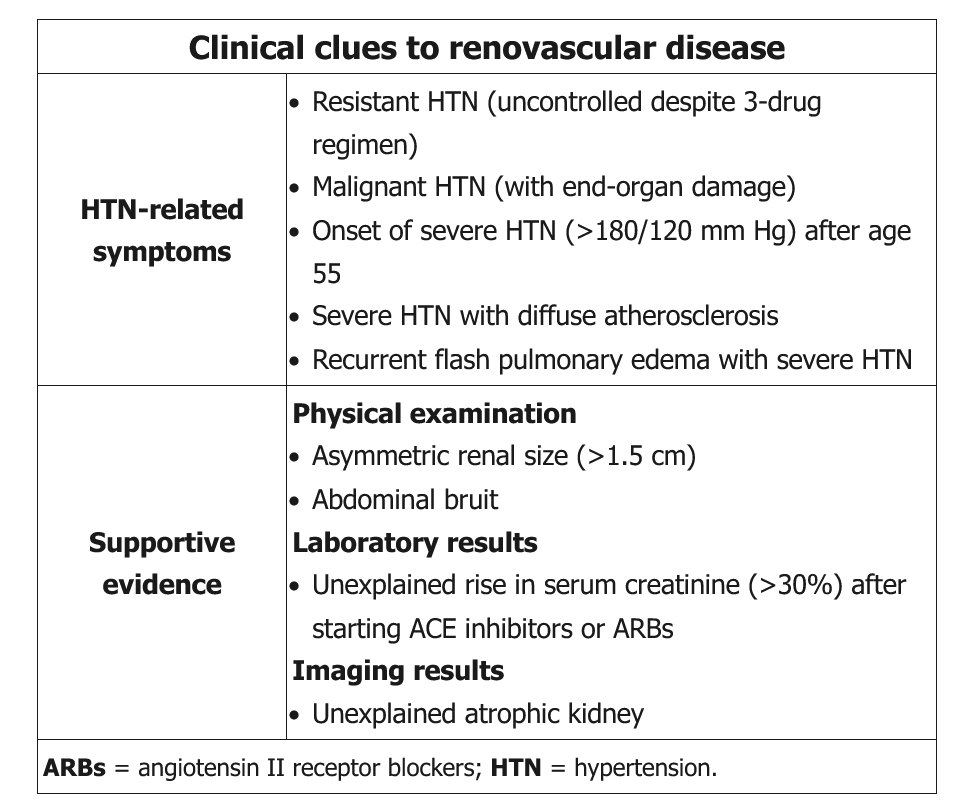
This patient is experiencing her second episode of flash pulmonary edema associated with severe hypertension. She has peripheral arterial disease (intermittent claudication) and multiple risk factors (smoking, diabetes, hyperlipidemia) for diffuse atherosclerosis. Recurrent
-
AKI in Transplant Patients
AKI in transplant patients
- related: Nephrology
- tags: #nephrology
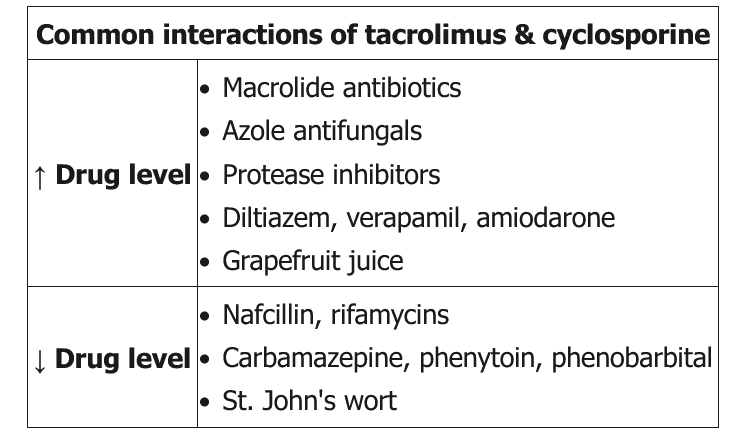
This patient has acute kidney injury and electrolyte abnormalities while on tacrolimus and fluconazole; this should raise suspicion for calcineurin inhibitor nephrotoxicity. Calcineurin inhibitors (eg, tacrolimus, cyclosporine) are common immunosuppressants used in organ transplantation; toxicity may be due to me
-
Hypernatremia
hypernatremia
- related: Nephrology, hyponatremia
- tags: #nephrology
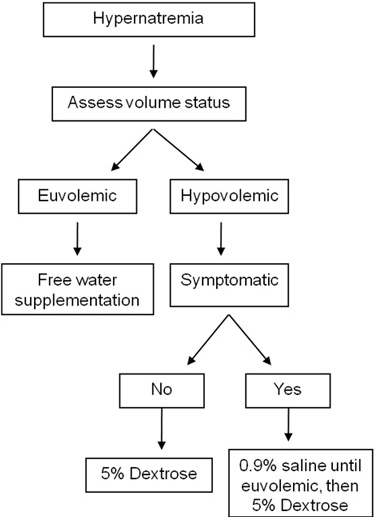
Hypotonic fluid loss usually activates the thirst mechanism to increase one's water consumption and prevent the development of hypernatremia, provided that the ongoing fluid loss has stopped. Most individuals that develop hypernatremia have neurologic deficits, so they either do not sense or cannot express thirst. Elde
-
Use ACE I in Renal Artery Stenosis
use ACE I in renal artery stenosis
- related: Nephrology
- tags: #nephrology
This elderly patient who has uncontrolled hypertension despite multidrug therapy and is found to have high-grade bilateral renal artery stenosis (>60% stenosis) should be treated with an ACE inhibitor.
Bilateral renal ischemia (caused by limited blood supply to the poststenotic kidney) induces the activation of the renin-angiotensin-aldosterone system (RAAS), which leads to
-
Sickle Cell Disease Can Cause Papillary Necrosis
sickle cell disease can cause papillary necrosis
- related: Nephrology
- tags: #nephrology
This patient presents with recurrent gross hematuria. The absence of active urinary sediment makes intrinsic glomerular disease less likely. The normal ultrasound findings and lack of clinical symptoms also makes a structural kidney lesion, kidney stone, or urinary tract infection less likely. Since he is a young African American, there is a high probability of sickle ce
-
Hypertension with Primary Hyperaldosteronism
hypertension with primary hyperaldosteronism
- related: Nephrology, Cardiology
- tags: #nephrology
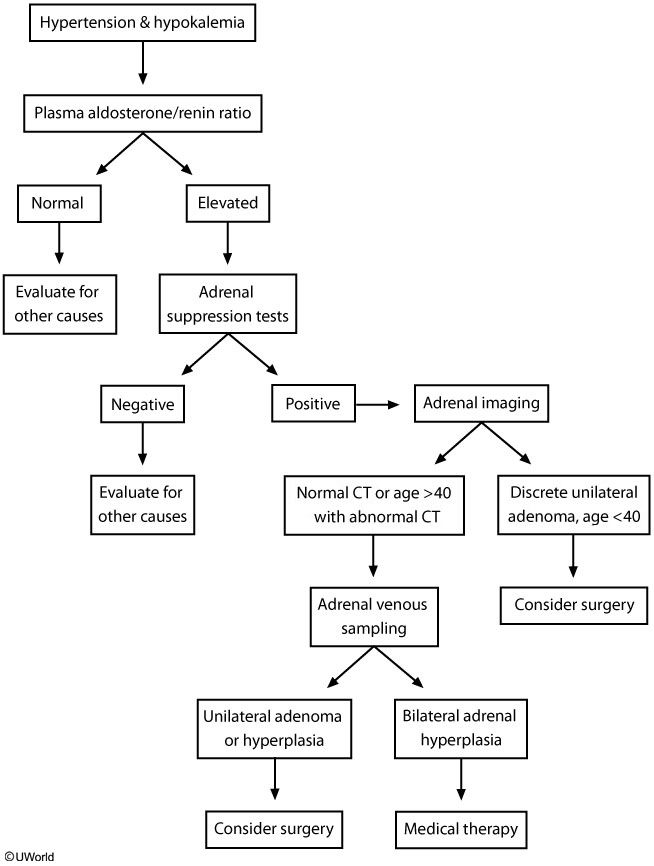
Primary hyperaldosteronism (PH) is characterized by hypertension associated with hypokalemia and metabolic alkalosis. Some patients may not have spontaneous hypokalemia but rapidly develop hypokalemia if given diuretics. Despite increased renal reabsorption of sodium, edema
-
Management of Renal Cysts
management of renal cysts
- related: Nephrology
- tags: #nephrology
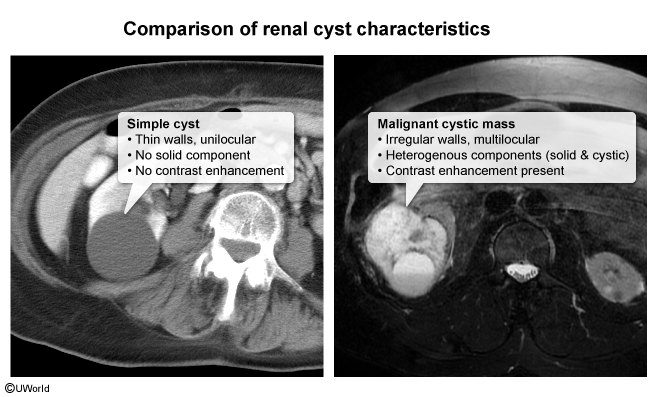
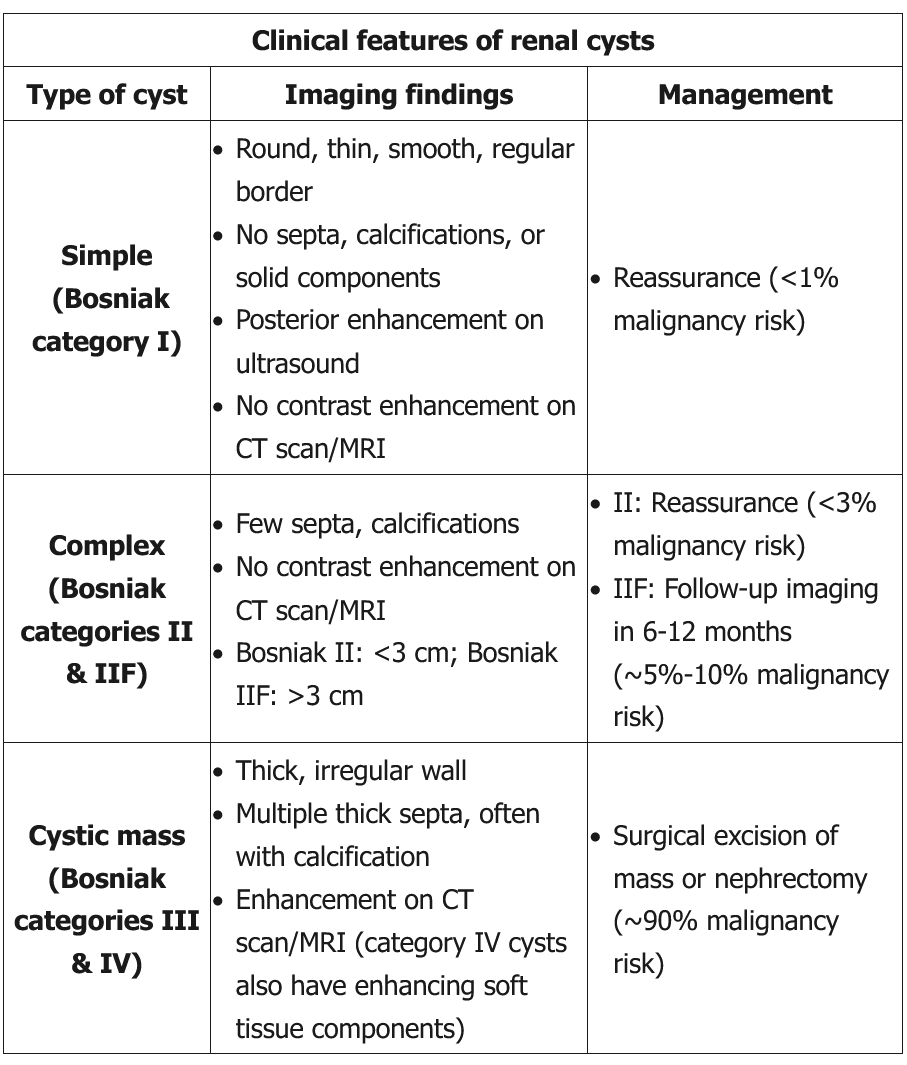
Renal cysts are classified as simple or complex based on imaging characteristics. Most (60%-70%) are simple cysts (Bosniak category I), occurring more commonly at age >50. These cysts are typically asymptomatic and do not cause renal damage or hyp
-
Start SGLT2 Inhibitors in CKD Patients with Proteinuria
start SGLT2 inhibitos in CKD patients with proteinuria
- related: Nephrology
- tags: #nephrology
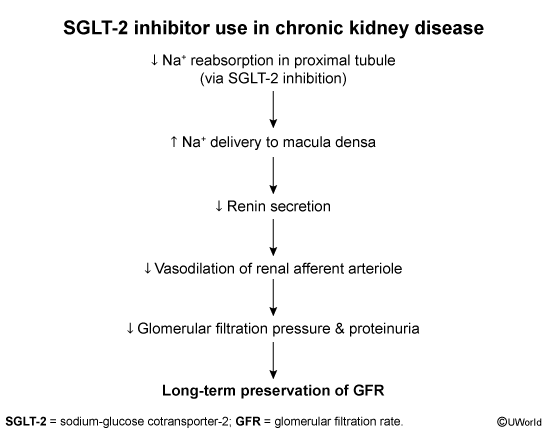
Patients with chronic kidney disease (CKD) should receive treatment for the underlying cause of the renal disease, such as blood pressure medications (eg, hypertensive nephrosclerosis) and glycemic control (eg, diabetic nephropathy). Those with proteinuric CKD should receive **additional m
-
Nonanion Gap Metabolic Acidosis NAGMA
nonanion gap metabolic acidosis NAGMA
- related: Nephrology, anion gap metabolic acidosis
- tags: #nephrology
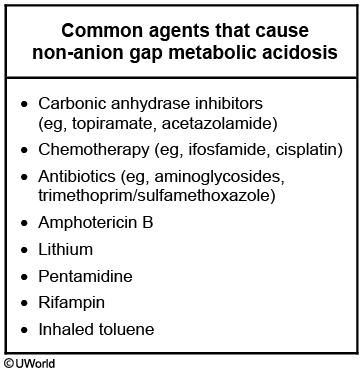
This patient presents with non-anion gap metabolic acidosis, which can be caused by numerous agents. Carbonic anhydrase inhibitors, including acetazolamide (used for glaucoma) and topiramate (used for seizures and migraine headaches), typically cause bicarbonate diuresis w
-
When to Place Fistulas for Dialysis
when to place fistulas for dialysis
- related: Nephrology
- tags: #nephrology
The rate of progression of late-stage chronic kidney disease (CKD) is variable and can be difficult to predict, with some patients quickly progressing to the need for renal replacement therapy and others remaining stable without it for a year or more. This unpredictability is likely due to frequently complex comorbidities and variable individual success of disease-alter
-
Medicine
Todos
Organ Systems
- Allergy and Immunology
- Rheumatology
- Cardiology
- Dermatology
- Endocrine
- ENT
- GI
- Hemeonc
- ID
- MSK
- Nephrology
- Urology
- Neurology
- Pulmonology
- Podiatry
Subject Areas
 ![](
![](