date: 2020-09-07
Dermatology
- related: Medicine
MKSAP
- Approach to the Patient with Dermatologic Disease
- Therapeutic Principles in Dermatology
- Common Rashes
- Disorders of Pigmentation
- Drug Reactions
- Acneiform Eruptions
- Common Skin Infections
- Infestations
- Bites and Stings
- Cuts, Scrapes, and Burns
- Common Neoplasms
- Pruritus
- Urticaria
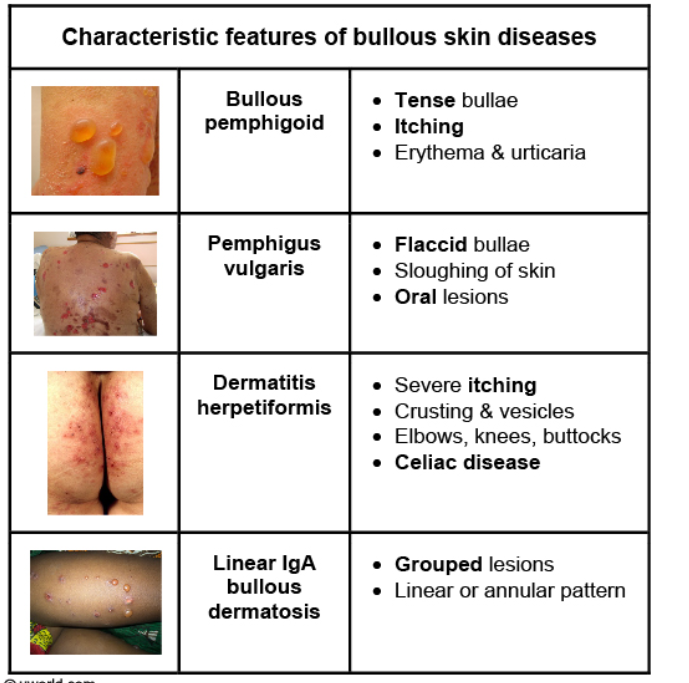
- Autoimmune Bullous Diseases
- Cutaneous Manifestations of Internal Disease
- Dermatologic Emergencies
- Hair Disorders
- Nail Disorders
- Disorders of the Mucous Membranes
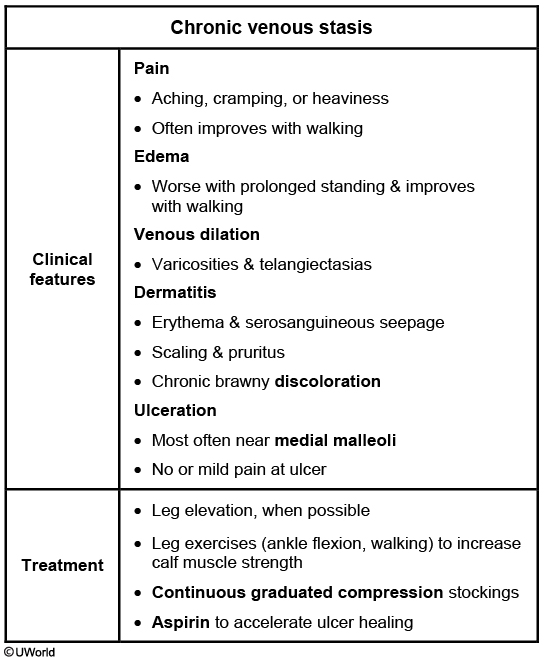
- Foot and Lower Leg Ulcers
- Dermatologic Conditions of Pregnancy and Aging
Others
- pseudofolliculitis barbae
- toxic shock
- hot tub folliculitis
- erythema nodosum
- skin and soft tissues infections
- Sweet syndrome
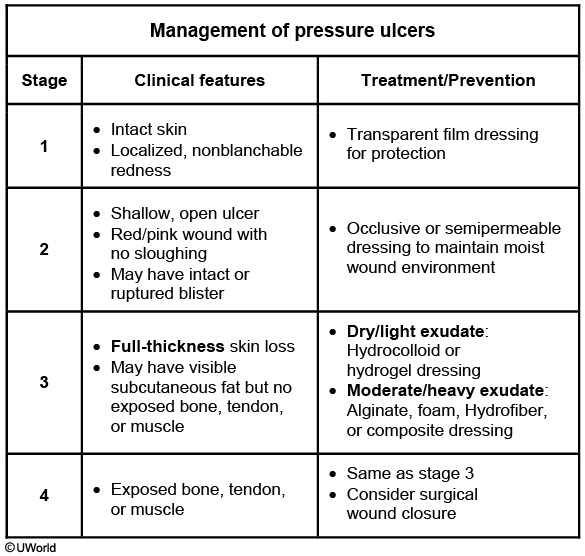
- treatment of pressure ulcers
Impetigo
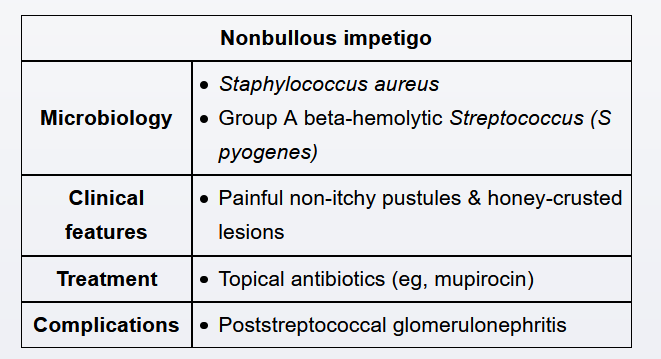
Impetigo is a contagious, superficial skin infection most commonly caused by Staphylococcus aureus or Streptococcus pyogenes. Infection often develops within superficial wounds, such as in this patient with a facial cut. It can also develop from any break in the skin, such as with eczema or insect bites. Presentation includes painful, nonpruritic, erythematous pustules that subsequently develop a classic, thick honey-colored crusting.
Diagnosis of impetigo is clinical. Topical antibiotics (eg, mupirocin) alone can treat isolated, small areas of infection, whereas oral antibiotics (eg, cephalexin) are warranted for extensive infection.
Hidradenitis

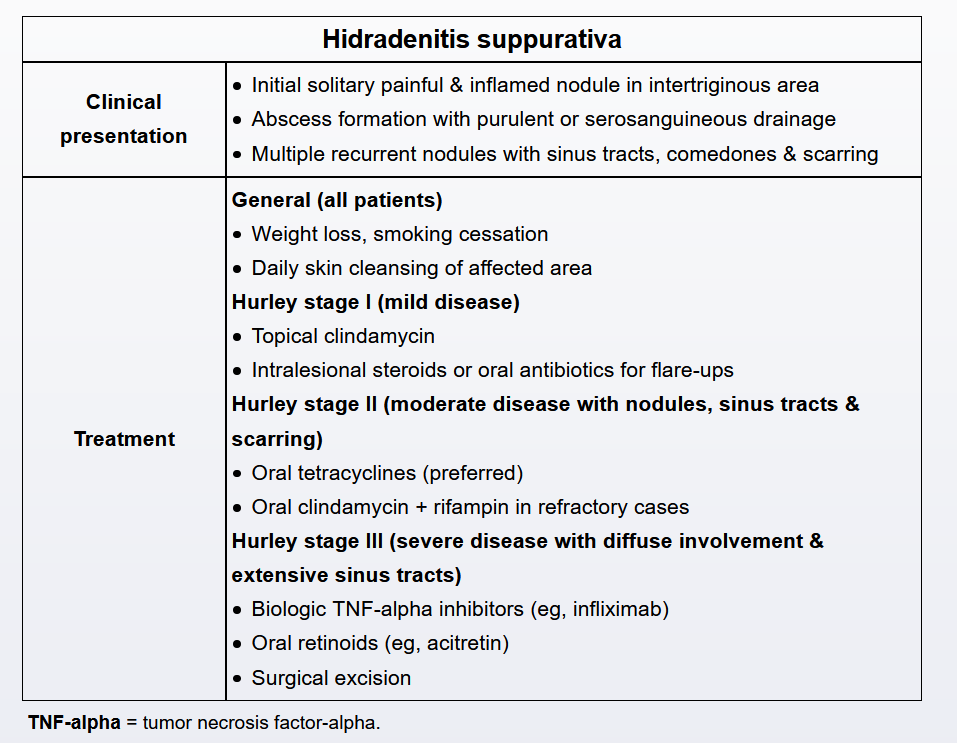
his patient's presentation is consistent with hidradenitis suppurativa (HS) (also known as acne inversa), a chronic inflammatory disorder characterized by occlusion of skin follicles. It is most commonly seen in intertriginous skin areas (eg, axillary, inguinal, genital, perianal, perineal), but can occur in any part of the skin that contains hair follicles. Risk factors for HS include family history of HS, smoking, obesity, and mechanical stress on the skin (eg, friction, patient manipulation). Patients typically develop an initial solitary and painful inflamed nodule in an intertriginous area that can last for several days to months before progressing to an abscess with purulent or serosanguineous drainage. The nodules and pain typically improve after drainage. Multiple recurrent nodules can lead to sinus tracts, comedones, and significant scarring.
General measures for all patients include weight loss, smoking cessation, and daily skin cleansing of the affected area. Mild disease (Hurley stage I) typically responds to topical clindamycin, but some patients may require intralesional steroids or oral antibiotics during flare-ups. Moderate disease (Hurley stage II) presents with inflammatory nodules, sinus tracts, and scarring (as seen in this patient). These patients require oral antibiotics (tetracyclines preferred) for several weeks to reduce inflammation and improve the infection. Severe and refractory disease (Hurley stage III) usually requires medical therapy with biologic TNF-alpha inhibitors (eg, infliximab) and/or oral retinoids (eg, acitretin) and occasionally surgical excision.
Incision and drainage of nodules in HS may provide pain relief for very painful abscesses. However, incision and drainage provides only short-term relief and is generally avoided as it does not prevent recurrent lesions.
Bullous Skin
Sebhorrheic Keratosis

This patient's rash is consistent with seborrheic keratosis (SK), a benign epidermal tumor due to proliferation of immature keratinocytes. SKs typically present after age 50 and are more common in fair-skinned individuals. The pathogenesis is not well understood. Patients can develop single or multiple lesions that are well-demarcated, pigmented, round or oval, and have a dull or verrucous surface with a "stuck-on" appearance. Typical locations include the face, upper extremities, and trunk.
SKs can be asymptomatic or cause pruritus, pain, or bleeding (especially with friction against clothing or jewelry). Explosive onset of multiple pruritic SKs (Leser-Trélat sign) has been associated with malignancies (especially lung and gastrointestinal tumors). Diagnosis is based on the lesions' clinical appearance but sometimes may require biopsy in uncertain cases. Because they are slow growing and benign, SKs usually do not require any treatment. However, symptomatic or cosmetically disfiguring lesions can be treated with cryotherapy or removed by curettage/shave excision or electrodessication.
Cutaneous cryptococcosis

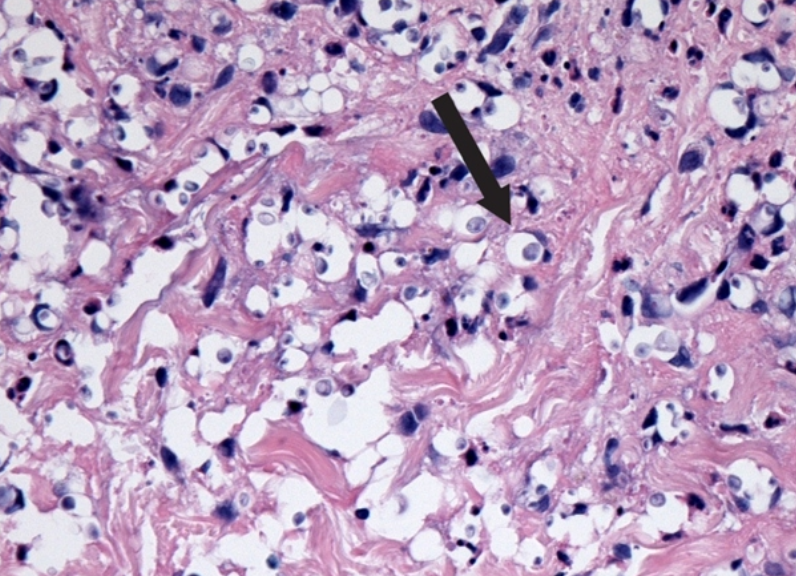
This patient with untreated HIV has widespread skin papules with umbilication, suggesting cutaneous cryptococcosis.
Cryptococcus neoformans is an encapsulated yeast that primarily affects patients who are significantly immunocompromised, particularly those with AIDS with CD4 counts <100/mm3. Although meningoencephalitis is the most common manifestation, pulmonary and/or disseminated disease may occur.
Cutaneous cryptococcosis is usually a manifestation of disseminated infection. Lesions tend to arise quickly with the head and neck preferentially affected. Although appearance may vary, the most common form is papules with central umbilication that resemble molluscum contagiosum. A small area of central hemorrhage or necrosis is an important diagnostic clue.
Disseminated infections also often affect the liver, lymph nodes, peritoneum, adrenal glands, and eyes.
iagnosis requires biopsy of a lesion; histopathological examination after staining (eg, periodic acid-Schiff, Gömöri methenamine silver nitrate) typically reveals hyperplasia of the overlying dermis with underlying granulomas surrounding encapsulated yeasts.
Cutaneous cryptococcosis is usually treated with >2 weeks of intravenous amphotericin B and oral flucytosine followed by a year of oral fluconazole (higher dose for 8 weeks, then maintenance).
Psoriasis
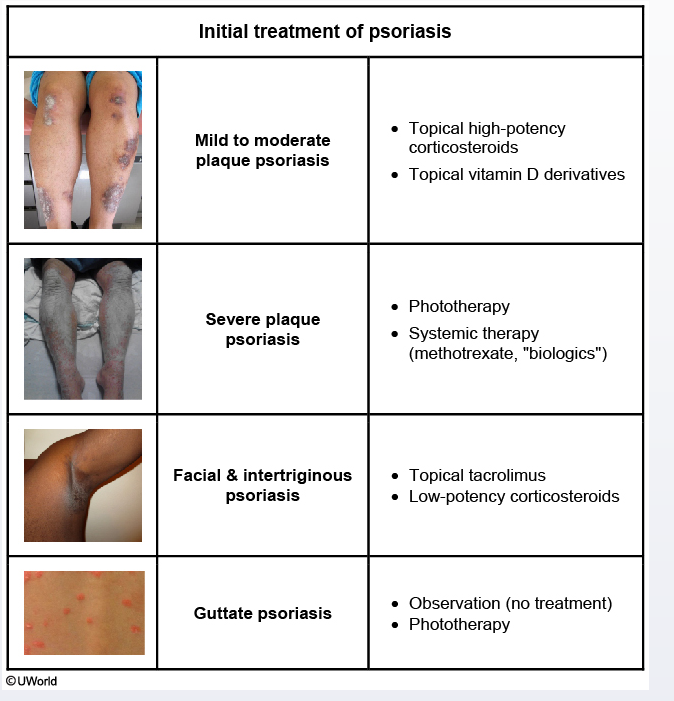
Psoriasis is a common inflammatory skin disorder characterized by erythematous, well-defined plaques covered by thick silvery scales. These lesions are typically seen over the scalp, knees, elbows, back, and nail plates. Patients are usually asymptomatic, but some may have mild itching. Most patients tend to have the disease for life and the severity varies significantly throughout the course of the disease.
A variety of different treatment options (local and systemic) are available for the treatment of psoriasis. Topical corticosteroids are the mainstay of therapy for localized mild-to-moderate plaque psoriasis. High-potency agents (eg, fluocinonide, augmented betamethasone dipropionate 0.05%) should be used initially to treat thick plaques on extensor surfaces; these are given as a twice-daily application for up to 4 weeks. Longer treatment is an option but should be closely monitored, and lower-potency agents should be considered. The lesions may be covered with an occlusive barrier (eg, plastic wrap or occlusion tape) after application to maximize treatment effects.
Seborreic

This patient's erythematous, scaly rash has the typical appearance of seborrheic dermatitis (SD). SD predominantly affects areas with heavy concentrations of sebaceous glands, including the scalp (where it is referred to as "dandruff"), central face (eg, eyebrows, nasolabial folds), and ears. In addition, SD may occasionally be seen on the chest, upper back, axilla, and inguinal/pubic area. SD is most common in the first year of life and again in adulthood. The diagnosis of SD is primarily clinical, with typical findings characterized by pruritic, erythematous plaques with loose, greasy-looking scales.
Malassezia species may play a role in the pathogenesis of SD, and topical antifungal agents (eg, ketoconazole, selenium sulfide) are effective in treating this condition. Other treatments that can be helpful include topical glucocorticoids, keratolytic agents (eg, salicylic acid), coal tar shampoo, and topical calcineurin inhibitors (eg, pimecrolimus, tacrolimus).
Seborrheic dermatitis (SD) is a chronic, relapsing condition. Initial treatment can provide significant improvement in symptoms but is rarely adequate to induce long-term remission (Choice D). As a result, patients usually benefit from intermittent re-treatment. Typical regimens include topical ketoconazole or ciclopirox every 1-2 weeks.

Lichen planus

This patient's rash is most consistent with lichen planus, which is characterized by papules best remembered with the ''4 Ps'': pruritic, planar, polygonal, and purple. The lesions of lichen planus are typically well-defined, and most commonly involve the flexor surfaces of the extremities, although the mucous membranes and genitals can also be affected. Characteristic white, lacelike patterns known as Wickham striae are sometimes seen on the surface of the papules.
Lichen planus is usually seen in middle-aged adults. Although its etiology is unknown, this condition is probably the result of immunologic factors. Lichen planus can arise with the use of certain medications, but this patient's amlodipine is not particularly associated with the disorder. Treatment generally consists of topical corticosteroids, and antihistamines may help control the severe itching.