CLABSI
- related: ICU
- tags: #icu
- Look at time to positivity: for central line infection, culture becomes positive 2 hours from central line blood compared to peripheral blood
Cause
- cause:
- central line, HD catheters
- bacteria:
- coag neg staph
- staph aureus
- GNR
Empiric treatment
- management:
- 2 sets of blood cultures, ideally one from a peripheral site and one from the central catheter
- Empiric antibiotic therapy should then be initiated with vancomycin plus cefepime (or gentamicin).
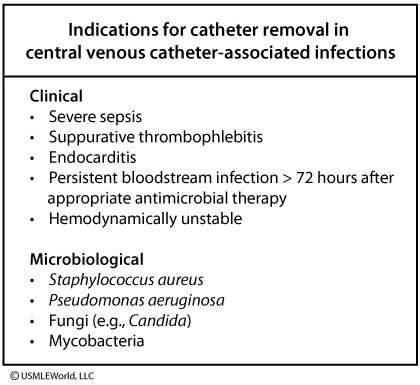
Catheter removal
- Catheter removal is indicated if any of the following are present:
- Severe sepsis
- Hemodynamic instability
- Evidence of metastatic infection (eg, endocarditis)
- Pus at the exit site of the catheter
- Continued symptoms after 72 hours of empiric antibiotics
Systemic antibiotics are usually not required for tunneled catheter-related bloodstream infection (CRBSI) patients with positive catheter tip culture, phlebitis without signs of infection (e.g., fever), or those with positive blood cultures through the catheter but negative cultures from the peripheral vein. All other cases (such as with this patient) usually require systemic antibiotics in addition to catheter removal. If catheter removal carries a high risk for reinsertion, then guidewire exchange may also be attempted. In patients with uncomplicated CRBSI, catheter salvage with close monitoring may be attempted.
Certain organisms (e.g., coagulase-negative Staphylococcus) can form biofilms on central venous catheter surfaces, making it very difficult to eradicate these organisms without catheter removal. Antimicrobial “lock” therapy involves placing a supratherapeutic antibiotic amount (100-1000 times higher than the normal dose) in the catheter lumen for hours to days to attempt catheter salvage in these cases. However, Pseudomonas aeruginosa CRBSI usually has poor outcomes with catheter salvage, thus long-term catheters should be removed. Afterwards, surveillance blood cultures should be drawn to document bacteremia clearance.
Catheter-related bloodstream infections due to E. coli susceptible to cephalosporins can be treated with systemic antibiotics and catheter salvage as long as there are no acute indications for catheter removal. However, catheter removal should be strongly considered for CRBSI due to multidrug resistant E. coli.
Catheter salvage may be considered for stable CRBSI due to E. faecalis and Streptococcus species as long as the patient has no acute indications for catheter removal.
Unless the patient has indications for catheter removal, current guidelines allow catheter salvage for infections from coagulase-negative Staphylococcus sensitive to vancomycin. However, catheter salvage should be avoided in catheter associated infections caused by Staphylococcus aureus.
- Infected CVCs should be removed. CVC removal is particularly important for S. aureus, P. aeruginosa, and Candida species infections.
- Patients who do not require catheter removal should have the catheter changed over a guidewire (once afebrile and clinically stable if there is no evidence of tunnel tract involvement) or antibiotic lock therapy after each hemodialysis session. These measures are required to prevent recurrent infection.
Duration of treatment
- The duration of therapy for most cases of uncomplicated non–S. aureus CLABSI is 7 to 14 days. S. aureus CLABSI is usually treated for at least 4 weeks; however, shorter-term therapy (2 weeks) may be considered in select patients who have immediate catheter removal with resolution of fever and bacteremia within 72 hours of starting appropriate therapy and who have no implanted prosthetic devices, no evidence of endocarditis by echocardiography (preferably transesophageal), no evidence of suppurative thrombophlebitis, no evidence of metastatic infection, and neither diabetes mellitus nor immunosuppression.
- Bacteremia clearance should be confirmed with follow-up blood cultures. If bacteremia persists after CVC removal and appropriate antimicrobial therapy, evaluation for a deeper source of infection, including endocarditis, should be performed. All patients with candidemia should be evaluated by an ophthalmologist to rule out the presence of candida endophthalmitis within 1 to 2 weeks.