ADPKD
ADPKD (autosomal-dominant polycystic kidney disease) is the most common genetic cause of chronic kidney disease in adults. ADPKD is a progressive multi-systemic disorder characterized by cyst formation within the kidneys and other organs (e.g. liver, spleen, pancreas).
Development of 100s to 1000s of large, round expanding cysts by 20-25 years of age leads to **massive bilateral kidney enlargement, destruction of renal parenchyma, and ultimately renal failure later in life. **
ADPKD is caused by mutations in the PKD1 (polycystin-1) gene (85%) and the PKD2 (polycystin-2) gene (15%).
Mutations in PKD1 are associated with more severe disease, resulting in ESRD (end-stage renal disease) at an earlier age (55 years of age), while patients with PKD2 mutations present much later in life (75 years of age).
PKD1 encodes polycystin-1: a transmembrane protein important for connective tissue cohesion between renal tubular epithelial cells (esp. the distal nephron) as well as other cells throughout the body.
Patients with autosomal dominant polycystic kidney disease are often asymptomatic with normal renal function until their 40s and 50s.
When symptomatic, patients typically present with hypertension (most common presenting symptom), abdominal mass or enlargement from enlarging kidneys, flank pain, polydipsia, and polyuria.
Renal failure typically occurs from recurrent pyelonephritis and nephrolithiasis.
Diagnosis
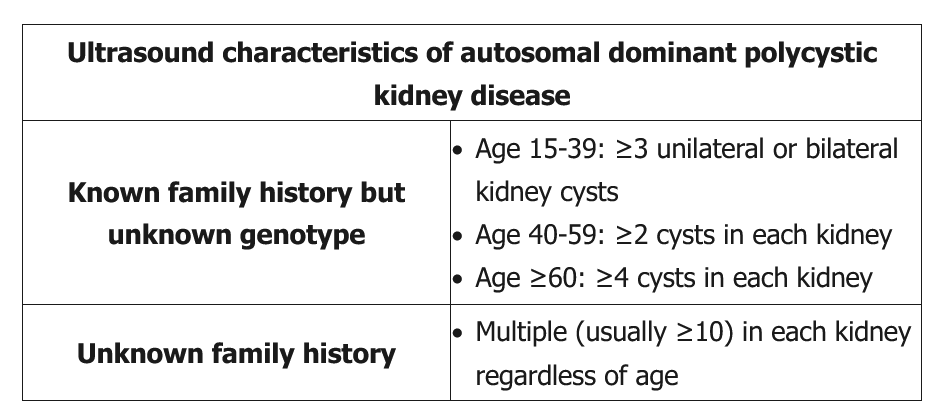
Ultrasonography is the best initial diagnostic test for ADPKD, and can detect cysts within the kidneys, liver, and pancreas.
CT and MRI are more sensitive and used when there is a negative ultrasound with a strong family history.
Genetic testing can provide a definitive diagnosis of ADPKD. Genetic testing is typically performed in patients who have a strong family history and in those with negative imaging studies who are being considered as potential kidney donors.
Genetic testing is usually reserved for those with suspected ADPKD who do not have a clear diagnosis by ultrasound. If US diagnosed ADPKD, genetic testing may not be needed.
Patients age ≥18 with a family history of autosomal dominant polycystic kidney disease (ADPKD) should be screened for the disorder using renal ultrasound. Early recognition of ADPKD aids in family planning and the management of potential disease complications (eg, hypertension, renal insufficiency). Counseling is performed as a diagnosis of ADPKD often can result in psychological consequences, have an impact on career decisions, and potentially affect ability to obtain life insurance.
Other helpful tests include the following:
- Urinalysis- typically reveals mild proteinuria and/or hematuria
- GFR - decreased, based on the degree of nephron involvement
- CBC - may reveal anemia
- Serum calcium and phosphorous levels - hypocalcemia and hyperphosphatemia may result depending on the degree of renal failure
This patient's number of kidney cysts, liver cysts, and possible family history of cerebral aneurysm (father's stroke) is consistent with likely autosomal dominant polycystic kidney disease (ADPKD). The characteristic ultrasound findings for ADPKD are listed in the above table. Autosomal dominant polycystic kidney disease is frequently associated with hepatic cysts (up to 20-80% of patients), pancreatic cysts, cerebral aneurysms (5-20% of patients), cardiac valvular disease (e.g., mitral or aortic regurgitation), and diverticulosis. Genetic testing should be performed in this patient to confirm the diagnosis. Treatment is mainly supportive with close follow-up to monitor renal function and treatment of associated conditions (e.g., hypertension).
Complications
Extrarenal congenital anomalies associated with ADPKD include:
- Extrarenal cysts: liver (hepatic cysts most common) > pancreas > spleen
- Intracranial berry aneurysm (most commonly at the junction of the anterior communicating artery with the ACA (anterior cerebral artery)
- Mitral valve prolapse (midsystolic click) and aortic regurgitation
- Colonic diverticula
- Abdominal wall and inguinal hernia
ADPKD may result in complications such as renal failure, liver failure, myocardial infarction, stroke, ruptured intracranial aneurysm, and even death.
Patients with ADPKD are also at an increased risk of renal cell carcinoma.
Treatment
Treatment is primarily supportive and typically consists of medications to help control complications such as hypertension, hyperlipidemia, fluid overload, and metabolic disturbances.
ACE inhibitors (e.g. captopril, lisinopril) and angiotensin receptor blockers (e.g. losartan, candesartan) are the first-line agents for treating patients with hypertension and ADPKD.
Additional treatments for patients with ADPKD include:
- Statins (e.g. pravastatin)
- Antibiotics to treat UTIs
- Surgical drainage of symptomatic cysts
- Dialysis in patients with ESRD
The only curative treatment for ADPKD is transplantation.
Examples questions
A 42-year-old woman comes to the office for evaluation of elevated blood pressure. She says, "I checked my blood pressure on a machine at the pharmacy, and it was 160/90 mm Hg. The pharmacist said I should see a doctor." The patient has no history of hypertension and has had no chest pain, headache, or focal weakness or numbness. She notes occasional episodes of pain in her flanks, which she ascribes to muscle tension. The patient has had several urinary tract infections over the course of her life but has no chronic medical problems and takes no medication regularly. She does not use tobacco, alcohol, or illicit drugs. The patient is married and has a son. Her mother has hypertension, her father died at an early age in a motor vehicle collision, and her uncle has renal failure and receives dialysis. Blood pressure is 156/94 mm Hg on the right arm and 152/96 mm Hg on the left arm. Pulse is 80/min and respirations are 16/min. Jugular venous pressure is within normal limits. Breath sounds are normal bilaterally with no crackles. Point of maximal impulse is displaced to the left and down. Heart sounds are normal with no murmur or gallops. The abdomen is soft with bilateral flank fullness. Bowel sounds are active. Laboratory results are as follows.
Urinalysis shows dysmorphic erythrocytes and mild proteinuria. ECG shows left ventricular hypertrophy with nonspecific ST-T wave changes.
After learning about the disease, the patient becomes worried that her 19-year-old son may also have the same condition. Which of the following is the most appropriate response to the patient? Screen US